Bloodstream infection by Candida species has a high mortality in Latin American countries. The aim of this study was to describe the characteristics of patients with documented bloodstream infections caused by Candida species in third level hospitals and determine the risk factors for in-hospital-mortality.
MethodsPatients from seven tertiary-care hospitals in Bogotá, Colombia, with isolation of a Candida species from a blood culture were followed prospectively from March 2008 to March 2009. Epidemiologic information, risk factors, and mortality were prospectively collected. Isolates were sent to a reference center, and fluconazole susceptibility was tested by agar-based E-test. The results of susceptibility were compared by using 2008 and 2012 breakpoints. A multivariate analysis was used to determinate risk factors for mortality.
ResultsWe identified 131 patients, with a median age of 41.2 years. Isolates were most frequently found in the intensive care unit (ICU). Candida albicans was the most prevalent species (66.4% of the isolates), followed by C. parapsilosis (14%). Fluconazole resistance was found in 3.2% and 17.6% of the isolates according to the 2008 and 2012 breakpoints, respectively. Fluconazole was used as empirical antifungal therapy in 68.8% of the cases, and amphotericin B in 22%. Hospital crude mortality rate was 35.9%. Mortality was associated with age and the presence of shock at the time of Candida detection. Fluconazole therapy was a protective factor for mortality.
ConclusionsCandidemia is associated with a high mortality rate. Age and shock increase mortality, while the use of fluconazole was shown to be a protective factor. A higher resistance rate with new breakpoints was noted.
Candidemia is the main invasive fungal infection that occurs in hospitalized patients; Candida species account for almost 80% of fungal pathogens causing nosocomial infections.1 The incidence of candidemia has increased more than five-fold in the last decade.2 Recent data show an overall incidence of candidemia ranging from 0.2 to 0.5 cases per 1000 admissions.3 An incidence ranging from 0.28 to 0.96 cases per 1000 admissions has been found in the United States; in Europe, an incidence of 0.2–0.38 cases per 1000 admissions is estimated.4 Recently, an incidence of 1.18 cases per 1000 admissions was found in Latin America; in particular, the highest incidence was found in Colombia, with 1.96 cases per 1000 admissions,5 much higher than the reported incidences in the northern hemisphere, with a trend to increase over the last decade.
Candidemia is associated with prolonged hospital stay, increased costs, and a higher mortality rate that can vary from 25% to 60%.6 In Latin America, particularly in Colombia, there is little information on epidemiological and clinical aspects of patients with candidemia. The present study describes the clinical and epidemiological characteristics of patients with candidemia in Colombian tertiary-care hospitals. The distribution of species, their fluconazole susceptibility profile, mortality rates, and a multivariate statistical analysis of factors associated with mortality are presented.
Materials and methodsStudy designThis was an observational, multicenter study conducted over a period of 12 months on patients who had experienced at least one episode of candidemia between March 8, 2008 and March 7, 2009 in seven tertiary-care hospitals of Bogotá, Colombia. Hospitals that participated in the study after having approved the research protocol were: Instituto Nacional de Cancerología (INC), Hospital Universitario San Ignacio (HUSI), Hospital de San José (HSJ), Fundación CardioInfantil (FCI), Hospital Universitario Clínica San Rafael (HUCSR), Hospital Militar Central (HMC), and Hospital Universitario de la Samaritana (HUS). All of them were high complexity institutions, with intensive care units (ICU, approximately 165 beds), internal medicine and surgery wards. One of them was a reference center for cancer (INC), and four of them had an oncology/hematology ward (INC, HUSI, HSJ, HMC). Three of them were public (INC, HMC, HUS).
ProceduresThe study included all patients of any age group admitted to participating institutions during the study period with a diagnosis of infection with yeast of the genus Candida in blood, confirmed by microbiology. The clinical laboratories of the institutions included in the study identified and typified the presence of Candida in blood cultures using automated methods (BACTEC, Becton Dickinson, USA). The isolates of Candida species were referred to the Instituto Nacional de Cancerología, where the strains were typed again in the mycology laboratory (Yeast ID, MicroScan, Dade Behring, Siemens, USA) and their susceptibility to fluconazole was tested by the agar based E-test method. At the same time, epidemiological and clinical information of the patients were prospectively collected, and the patients were followed until discharge or death.
Study variables and definitionsEpidemiological variables, inpatient services, and inpatient days were included. The clinical variables and risk factors were the presence of various comorbidities (tumors, diabetes, chronic renal insufficiency, etc.), systemic inflammatory response syndrome (SIRS), organ dysfunction, or shock at diagnosis of candidemia. The main recorded microbiological variable was blood culture positivity time from sampling to the report from the blood culture team. We also recorded several treatment variables. An episode of candidemia was defined as the isolation of a Candida species from one or more blood cultures. The age ranges were defined as neonates: ≤28 days old or staying in the Neonatal Intensive Care Unit (for the premature); children: age over 28 days up to 18 years; adults: between 19 and 60 years; elderly: ≥60 years. For the number of organs involved, the Score Organic Failure (SOFA) scale was used. Abdominal surgery was defined as a recent surgical procedure that involved the gastrointestinal tract within the last two weeks. Prolonged corticotherapy was defined as doses >0.5mg/kg/day of prednisone or equivalent corticosteroid or cumulative dose higher than 700mg. Previous fluconazole exposure was any hospital use of fluconazole seven days before the blood cultures were taken in which the Candidia species was isolated. The interpretation of susceptibility to fluconazole was initially performed with breakpoints from the Clinical Laboratory Standards Institute (CLSI), 2008 (CLSI 2008) where a minimum inhibitory concentration (MIC) ≤8mg/L is considered susceptible (S), ≥64mg/L resistant (R), and intermediate values susceptible dose-dependent (SDD). A posteriori analysis taking into account the existing cutoffs proposed by Pfaller et al. in 20127 was conducted. For C. albicans, C. parapsilosis, and C. tropicalis, S was defined as a MIC≤2mg/L, R a MIC≥8mg/L, and SSD intermediate MIC values. For C. glabrata, MIC≤32mg/L was considered SDD, and MIC≥64mg/L were considered R. Inappropriate use of fluconazole was defined as the use of fluconazole in patients with resistance to fluconazole by susceptibility testing. Mortality was assessed at 14 days after detection of candidemia and hospital mortality.
Statistical analysisFor descriptive analyses mean and standard deviation (SD) for continuous variables and percentages for categorical data were calculated. For evaluating association between mortality and demographic and clinical variables, preliminary univariate analyses were performed calculating crude odds ratios (ORs). A multivariate analysis of all factors found to be significant on univariate analysis and of the most clinically relevant variables was performed to estimate adjusted ORs. Statistical analyses were performed with Stata 11. All reported p-values were two-sided and considered significant when less than 0.05 Confidence intervals of 95% were estimated.
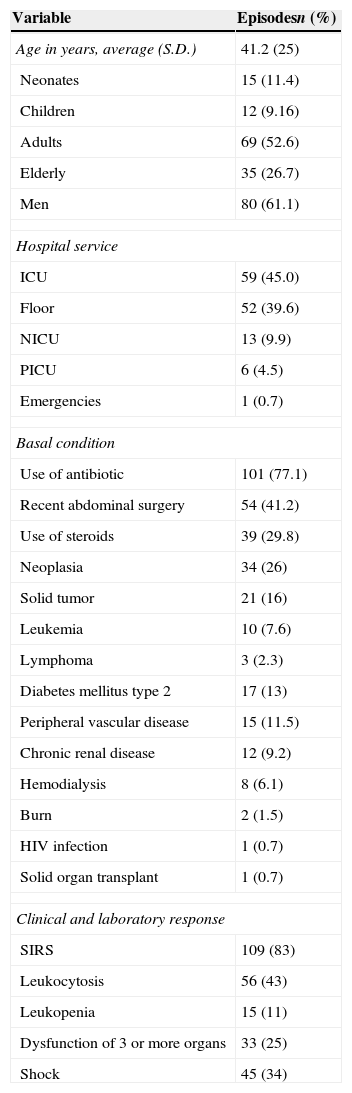
ResultsA total of 131 patients with candidemia were included in the study. The mean age was 41.2 years, with a standard deviation (SD) of 25 years, ranging from 9 days to 87 years. The male:female ratio of these patients was 1.6:1. The inpatient service with the greatest frequency of isolates was the adult ICU, with 45% (n=59 patients), followed by the inpatient floors, with 39.6% (n=52 patients). The mean duration of hospitalization was 53 days (range 3–219 days). In total, 78.6% of patients had been to the ICU at some point during their hospitalization (n=103 patients) and had an average ICU stay of 29 days (range 1–125 days). The mean time from hospital admission to a later identification of candidemia was 24 days (range 1–101 days). To perform blood cultures, the most used venipuncture site was the peripheral vein, in 75.5% of cases (n=99 patients). Seventy-three patients (55.7%) had a single positive blood culture, 46 (35.1%) two positive blood cultures, and 12 (9.1%) three positive blood cultures. On average, blood cultures yielded positive results 36.3h after collection (range 0–5 days; 90th percentile=56h). In 51 (38.9%) patients, bacteremia was documented by blood culture in the days prior. Gram-positive cocci were the most frequent type of isolated bacteria (n=23 patients, 45.2%), followed by Gram-negative bacilli (n=20, 39.2%). Polymicrobial bacteremia was identified in 8 (15.7%) patients. Some epidemiological findings are summarized in Table 1.
Demographic and clinical features in patients with candidemia (n=131).
| Variable | Episodesn (%) |
|---|---|
| Age in years, average (S.D.) | 41.2 (25) |
| Neonates | 15 (11.4) |
| Children | 12 (9.16) |
| Adults | 69 (52.6) |
| Elderly | 35 (26.7) |
| Men | 80 (61.1) |
| Hospital service | |
| ICU | 59 (45.0) |
| Floor | 52 (39.6) |
| NICU | 13 (9.9) |
| PICU | 6 (4.5) |
| Emergencies | 1 (0.7) |
| Basal condition | |
| Use of antibiotic | 101 (77.1) |
| Recent abdominal surgery | 54 (41.2) |
| Use of steroids | 39 (29.8) |
| Neoplasia | 34 (26) |
| Solid tumor | 21 (16) |
| Leukemia | 10 (7.6) |
| Lymphoma | 3 (2.3) |
| Diabetes mellitus type 2 | 17 (13) |
| Peripheral vascular disease | 15 (11.5) |
| Chronic renal disease | 12 (9.2) |
| Hemodialysis | 8 (6.1) |
| Burn | 2 (1.5) |
| HIV infection | 1 (0.7) |
| Solid organ transplant | 1 (0.7) |
| Clinical and laboratory response | |
| SIRS | 109 (83) |
| Leukocytosis | 56 (43) |
| Leukopenia | 15 (11) |
| Dysfunction of 3 or more organs | 33 (25) |
| Shock | 45 (34) |
S.D., standard deviation; ICU, intensive care unit; NICU, neonatal intensive care unit; PICU, pediatric intensive care unit, SIRS, systemic inflammatory response syndrome.
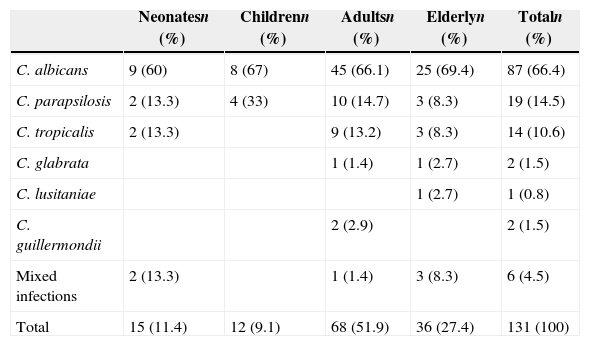
A total of 137 isolates of Candida species were found in the 131 patients; 6 patients (4.6%) presented mixed yeast infection. The most common species among monomicrobial isolates was C. albicans, in 87 (66.4%) patients, followed by C. parapsilosis in 19 (14.5%), and C. tropicalis in 14 (10.6%). Six cases of mixed infections were found: three cases of C. albicans and C. tropicalis infection, and three cases of mixed infections with C. parapasilopsis (C. albicans, C. famata, and C. tropicalis, each one). Species distribution according to age groups is shown in Table 2 and no statistical differences were seen among those groups. Sixty-eight patients (51.9%) were adults. The global mortality rate was 35.9% (n=47 patients) and was higher in the group of elderly people (n=22, 61.1%). The mortality rate in the group of patients with C. albicans was 37.9% (n=33), while those with non-albicans Candida (NAC) species had a mortality rate of 31.5% (n=12). The mortality rate in the group of mixed infections was 33.3% (n=2). Mortality rate was higher in C. glabrata and C. lusitanae cases (100%), than in C. parapsilopsis and C. tropicalis cases (26.3% and 28.5%, respectively). The two cases of C. guillermondii survived. There was no significant difference in mortality rates among different Candida species. Mortality was higher among those aged more than 60 years old (61.1%), than adults (39.4%), children (16.6%), and neonates (11.4%) (p<0.05 for the comparison between eldery and the other age groups).
Frequency of identified species by age group.
| Neonatesn (%) | Childrenn (%) | Adultsn (%) | Elderlyn (%) | Totaln (%) | |
|---|---|---|---|---|---|
| C. albicans | 9 (60) | 8 (67) | 45 (66.1) | 25 (69.4) | 87 (66.4) |
| C. parapsilosis | 2 (13.3) | 4 (33) | 10 (14.7) | 3 (8.3) | 19 (14.5) |
| C. tropicalis | 2 (13.3) | 9 (13.2) | 3 (8.3) | 14 (10.6) | |
| C. glabrata | 1 (1.4) | 1 (2.7) | 2 (1.5) | ||
| C. lusitaniae | 1 (2.7) | 1 (0.8) | |||
| C. guillermondii | 2 (2.9) | 2 (1.5) | |||
| Mixed infections | 2 (13.3) | 1 (1.4) | 3 (8.3) | 6 (4.5) | |
| Total | 15 (11.4) | 12 (9.1) | 68 (51.9) | 36 (27.4) | 131 (100) |
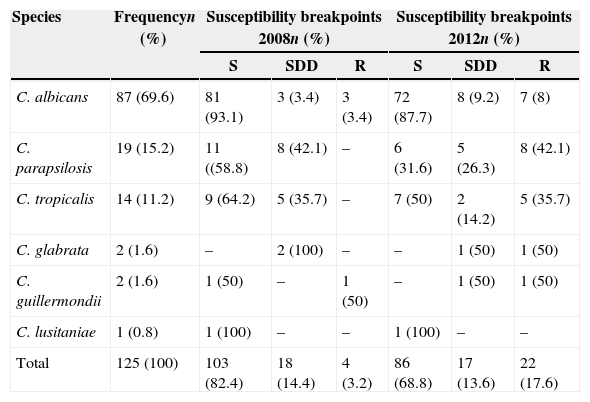
The susceptibility profile to fluconazole was identified with the breakpoints from the CLSI-2008 and those proposed in 2012 by Pfaller et al. For this analysis, 125 isolated species were considered (the six cases of mixed infection were not included). The average MIC for fluconazole was 0.87mg/L for all single isolates, and the MIC90 was 14mg/L. For C. albicans, a mean MIC for fluconazole of 0.5mg/L was found, with a MIC90 of 5.28, while for C. parapsilosis and C. tropicalis, the average MIC was 3.9mg/L and 2.85mg/L, and the average MIC90 was 29mg/L and 15mg/L, respectively. Table 3 shows fluconazole susceptibility testing by the E-test with the two breakpoints. Fluconazole susceptibility differed significantly when the different breakpoints were used. With the CLSI-2008 breakpoints, 103 (82.4%) isolates were S, 18 (14.4%) were SDD, and 4 (3.2%) R. Considering the 2012 breakpoints, 86 (68.8%) isolates were S, 17 (13.6%) were SDD, and 22 (17.6%) were R. With the CLSI-2008 breakpoints, 6.8% (n=6) of isolates were SDD or R; with the new cutoffs, this percentage rose to 17.2% (15 isolates). Similarly, NAC species presented higher frequency of SDD and R with the new breakpoints, changing from 12.8% (16 isolates) to 19.2% (24 isolates). Nine patients have received fluconazole at least one week before Candida isolation. The mean MIC was higher (21.3mg/L vs. 7.3mg/L) for those isolates from patients that had received fluconazole, but the difference was not statistically significant (p=0.063).
Susceptibility to fluconazole in monomicrobial isolates identified by E-test with the 2008 and 2012 breakpoints.
| Species | Frequencyn (%) | Susceptibility breakpoints 2008n (%) | Susceptibility breakpoints 2012n (%) | ||||
|---|---|---|---|---|---|---|---|
| S | SDD | R | S | SDD | R | ||
| C. albicans | 87 (69.6) | 81 (93.1) | 3 (3.4) | 3 (3.4) | 72 (87.7) | 8 (9.2) | 7 (8) |
| C. parapsilosis | 19 (15.2) | 11 ((58.8) | 8 (42.1) | – | 6 (31.6) | 5 (26.3) | 8 (42.1) |
| C. tropicalis | 14 (11.2) | 9 (64.2) | 5 (35.7) | – | 7 (50) | 2 (14.2) | 5 (35.7) |
| C. glabrata | 2 (1.6) | – | 2 (100) | – | – | 1 (50) | 1 (50) |
| C. guillermondii | 2 (1.6) | 1 (50) | – | 1 (50) | – | 1 (50) | 1 (50) |
| C. lusitaniae | 1 (0.8) | 1 (100) | – | – | 1 (100) | – | – |
| Total | 125 (100) | 103 (82.4) | 18 (14.4) | 4 (3.2) | 86 (68.8) | 17 (13.6) | 22 (17.6) |
S, susceptible; SDD, susceptible dose-dependent; R, resistant.
In total, 109 patients received antifungal treatment (including the six with mixed infections), of whom 44 (40%) started treatment before a positive blood culture result. The other 65 (60%) patients started treatment after blood culture results were known. The most widely used antifungal was fluconazole, in 75 (68.8%) cases, followed by amphotericin B in 24 (22%), caspofungin in 9 (8.2%), and itraconazole in 1 (0.9%). In the case of C. albicans (71 patients), the most used antifungal was fluconazole, in 51 (71.8%) patients, followed by amphotericin B in 12 (16.9%) and caspofungin in 7 (9.8%). In the case of NAC (32 patients), the most used antifungal was fluconazole, in 20 (62.5%) patients, followed by amphotericin B in 10 (31.3%) and caspofungin in 2 (6.2%). Similarly, the most used antifungal in the case of mixed infections (six patients) was fluconazole in three patients (50%). Sixty-two (56.8%) received only one antifungal, and 33 (30.2%) received two antifungals during their hospital stay. The most frequent changes were fluconazole to amphotericin B and from fluconazole to caspofungin, both in 9 (27.2%) patients, followed by amphotericin B to fluconazole in 5 (15.1%). The average duration of antifungal treatment before any change or addition was 10 days (range 0–49 days). A third antifungal was used in 14 (12.8%) patients. Of the 14 patients who used three antifungals, 4 (28.5%) presented mixed infection, 9 (64.2%) were infected with NAC, and 1 (7.1%) was infected with C. albicans. When considering the 71 patients with monomicrobial infection who were treated with fluconazole, inappropriate use of fluconazole increased from 2%, 0%, and 0% to 5.8%, 46.1%, and 25% for patients infected with C. albicans, C. parapsilosis, and C. tropicalis, respectively. The increases were significant for C. parapsilosis and C. tropicalis (p<0.05).
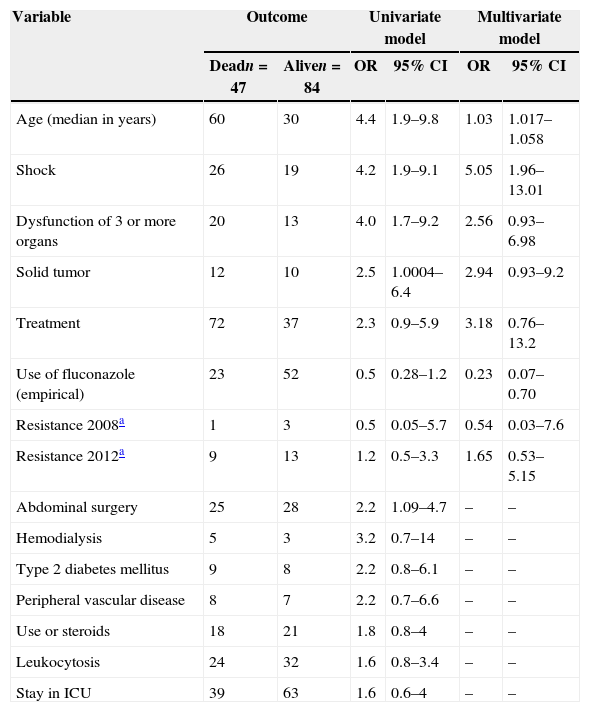
The mortality rate at 14 days after diagnosis of candidemia was 19.8% (26 cases), while mortality rate until the time of discharge was 35.9% (47 cases). In the group of patients who received antifungal therapy (109 patients), hospital mortality rate was 33.9%, while mortality in patients who received no treatment (22 patients) was 45.4% (OR 1.6; 95% CI 0.6–4.0). Mortality among patients with NAC and patients with C. albicans was 31.5% and 37.9%, respectively. Significant variables identified and included in the multivariate model were shock, dysfunction of three or more organs, neutrophilia (peripheral blood neutrophils >7500/mm3), solid tumor, and abdominal surgery (Table 4). When performing the multivariate logistic regression, age (OR 1.03; 95% CI 1.01–1.05) and the presence of shock (OR 5.05; 95% CI 1.96–13) at diagnosis were identified as the only variables independently associated with mortality. The use of fluconazole was a protective factor for mortality (OR 0.23; 95% CI 0.07–0.70).
Predictors of mortality in bivariate and multivariate logistic regression analysis.
| Variable | Outcome | Univariate model | Multivariate model | |||
|---|---|---|---|---|---|---|
| Deadn=47 | Aliven=84 | OR | 95% CI | OR | 95% CI | |
| Age (median in years) | 60 | 30 | 4.4 | 1.9–9.8 | 1.03 | 1.017–1.058 |
| Shock | 26 | 19 | 4.2 | 1.9–9.1 | 5.05 | 1.96–13.01 |
| Dysfunction of 3 or more organs | 20 | 13 | 4.0 | 1.7–9.2 | 2.56 | 0.93–6.98 |
| Solid tumor | 12 | 10 | 2.5 | 1.0004–6.4 | 2.94 | 0.93–9.2 |
| Treatment | 72 | 37 | 2.3 | 0.9–5.9 | 3.18 | 0.76–13.2 |
| Use of fluconazole (empirical) | 23 | 52 | 0.5 | 0.28–1.2 | 0.23 | 0.07–0.70 |
| Resistance 2008a | 1 | 3 | 0.5 | 0.05–5.7 | 0.54 | 0.03–7.6 |
| Resistance 2012a | 9 | 13 | 1.2 | 0.5–3.3 | 1.65 | 0.53–5.15 |
| Abdominal surgery | 25 | 28 | 2.2 | 1.09–4.7 | – | – |
| Hemodialysis | 5 | 3 | 3.2 | 0.7–14 | – | – |
| Type 2 diabetes mellitus | 9 | 8 | 2.2 | 0.8–6.1 | – | – |
| Peripheral vascular disease | 8 | 7 | 2.2 | 0.7–6.6 | – | – |
| Use or steroids | 18 | 21 | 1.8 | 0.8–4 | – | – |
| Leukocytosis | 24 | 32 | 1.6 | 0.8–3.4 | – | – |
| Stay in ICU | 39 | 63 | 1.6 | 0.6–4 | – | – |
OR, odds ratio; 95% CI, 95% confidence interval.
Our results confirm previous findings with respect to the epidemiology of candidemia in Colombia and its high mortality rate. A surveillance study of seven Latin American countries included information on Colombia, and patients there had lower mean age than in other countries but similar frequencies of other comorbidities, such as cancer and diabetes.5 A similar mean age and rates of cancer and diabetes to those identified in a multicenter study in Brazil were also observed.8 An advantage of the present study is that it provides information from a larger number of hospitals in Colombia. The overall mortality rate at discharge in our clinical series was 35.9%, similar to the 31.4% described in Japan9 and 44% in Spain,10 but lower than that reported in Brazil, which varied between 54% and 61%,8,11 or Italy, at 54%.2 It is also slightly lower than that identified in the aforementioned Latin American study.5 A recent multicenter study suggests that mortality attributable to candidemia has increased by approximately 30% in the ICU and by approximately 10% in inpatient services.12
The present study found that the majority of isolates were C. albicans, and C. parapsilosis, and C tropicalis were the most common NAC species. The Latin American study,5 as well as previous studies in Colombia,13,14 reported similar findings, although with a tendency toward more NAC species. In Brazil, the species most frequently identified was C. albicans, followed by C. parapsilosis and C. tropicalis.8,11 In other geographic areas, such as in India,20 NAC predominates, with a prevalence of 78%. In Taiwan,21 69.6% of isolates are NAC, with C. tropicalis and C. glabrata being the most frequent. These findings confirm the increased frequency of C. tropicalis and C. parapsilosis among species of NAC in Latin American.15
We chose to assess susceptibility to fluconazole by E-test because in previous studies this showed good correlation with the standard methods, with a low frequency of minor and major errors.16 However, this method has shown higher MICs compared to the standard microdilution methods, ranging from 2- to more than 6-fold higher.16 Another study that compared the same methods found smaller differences between the E-test and the standard test, with a level of agreement >93% and with smaller difference between the MICs, especially among the C. albicans isolates.17 One of the problems with the comparisons is the use of different methods for measuring susceptibility. A microbiological study in Colombia13 collected 2139 Candida isolates from different clinical samples and, using disk diffusion method, reported a resistance rate of 6.8%, with SSD strains constituting 5.1%. In the present study, using the E-test, we found a fluconazole resistance rate of 3.2% using the CLSI 2008 breakpoints. However, taking into account the new breakpoints proposed by Pfaller et al. in 2012 (resistance considered with MICs≥8mg/L), resistance up to 17.6% was encountered. In the group of NAC, a significant increase in the frequency of resistant species was observed. One study found higher MICs when the E-test was used than when microdilution tests were used, especially with isolates of C. tropicalis and other less common species of Candida.18 This change in the susceptibility results had an impact on the frequency of inappropriate therapy, with an increase of patients with resistant isolates treated with fluconazole. It is possible that differences in the MICs obtained by the E-test are relevant given the new breakpoints, which partially explains the high resistance rates identified. The previously mentioned Latin American study identified a low rate of resistance, even with the new breakpoints used for fluconazole, although the assessment was performed using broth microdilution.5 There is still controversy about the clinical usefulness of the proposed breakpoints since there is a lacking of clinical data to validate them.7 A previous pharmacodynamic study has shown a good correlation between dose and MIC, a more useful clinical information.19 There is still a need for clinical validation of in vitro breakpoints and clinical interpretation in Candida species. A Spanish surveillance study compared rates of resistance to fluconazole and other antifungals using the microdilution method with the previous breakpoints and the more recently recommended breakpoints, without finding important differences in resistance rates.20 A study similar to ours conducted in Brazil,21 in a reference institution using the E-test for susceptibility testing, showed a rate of susceptibility >97%, but 90% of the isolates had a MIC≥4mg/L, considered dose-dependent with the new breakpoints for some species. Another reason we identified higher rates of resistance may be that we included an oncology institution. The presence of hematological neoplasias is one of the few known predictors of resistance to fluconazole.9,22
In our clinical series the most commonly used antifungal in patients was fluconazole, followed by amphotericin B, in accordance with what has been described in the rest of Latin America5 and in contrast to rates identified in Brazil,11 where amphotericin B predominated, followed by the azoles. It is noteworthy that 22 patients (16.8%) received no treatment. There was no difference in mortality between treated and untreated patients, similar to the previous series in Brazil11 where 30% of patients received no treatment and mortality did not differ between treated and untreated. Other studies have identified a delay in the initiation of antifungal therapy as a predictor of mortality.23,24 Delays longer than 12–15h after the identification of positive blood cultures correlates with an increased risk of death in patients with candidemia. The allowable delay can be even shorter in patients identified to be in shock at the time of candidemia.25 Although our study shows that the use of fluconazole was associated with lower mortality, this result may have been related to less frequent use of other antimycotic agents. In the current recommendations in unstable patients, an echinocandin is preferred for its lower associated mortality and better safety profile compared to azoles and amphotericin, respectively.4,26
Our multivariate analysis showed that age and presence of shock at diagnosis of candidemia were significantly associated with mortality. In another series,27 APACHE II score, steroid use, inadequate dose of fluconazole, and indwelling central venous catheter were independent factors associated with mortality. In studies in Brazil11 and Italy,2 APACHE II score has also been independently associated with mortality. Importantly, our multivariate analysis found that despite the new breakpoints, fluconazole resistance was not associated with mortality, and treatment (grouping together all antifungals) was not associated with mortality. However, it must be highlighted that the use of initial therapy with fluconazole was a significant protective factor, reducing mortality by approximately 30%.
There are limitations to our study. Although tertiary-care hospitals were chosen, these hospitals are all located in the same city and therefore results might not generalizable to Colombia as a whole. However, there is limited information in Colombia of surveillance studies, so this contribution can be significant. It is also important to note that despite the fact that SOFA definitions were used for estimating the number of failing organs, neither SOFA score itself nor other prognostic index were used. In addition, the method considered standard for measuring susceptibility was not used (considering either CLSI or EUCAST methodology), and resistance may have been overestimated. As mentioned before, it limits the possibility of comparing our results with previous studies or the study of Latin American countries.
In conclusion, we found that bloodstream infection by Candida species followed the same patterns of risk in Colombia as elsewhere in Latin America, with shock and age being predictors of mortality. The identified isolates had low susceptibility to fluconazole, which may have been secondary to the assessment method, the change in breakpoints, or a real decrease in susceptibility observed over time, especially considering that the study population included an oncology institution.
Conflicts of interestThe authors declare no conflicts of interest.
We thank the staff of the Clinical or Microbiology Laboratory and the participating institutions: Instituto Nacional de Cancerología, Hospital Universitario San Ignacio (Beatriz Ariza), Hospital de San José (Adriana Jiménez), Fundación CardioInfantil (Alvaro Arango), Hospital Universitario Clínica San Rafael (Carlos Saavedra), Hospital Militar Central, and Hospital Universitario de la Samaritana (Carlos Pérez).