Dengue fever is a vector-transmitted viral infection. Non-vectorial forms of transmission can occur through organ transplantation. We reviewed medical records of donors and recipients with suspected dengue in the first post-transplant week. We used serologic and molecular analysis to confirm the infection. Herein, we describe four cases of dengue virus transmission through solid organ transplantation. The recipients had positive serology and RT-PCR. Infection in donors was detected through serology. All cases presented with fever within the first week after transplantation. There were no fatal cases. After these cases, we implemented dengue screening with NS1 antigen detection in donors during dengue outbreaks, and no new cases were detected. In the literature review, additional cases had been published through August 2017. Transmission of Dengue virus can occur through organ donation. In endemic regions, it is important to suspect and screen for dengue in febrile and thrombocytopenic recipients in the postoperative period.
The most common mechanism of transmission of dengue virus is via Aedes aegypti mosquitoes. There are few reports of other routes of transmission such as percutaneous transmission, blood transfusion1 or bone marrow and solid organ transplantation.2,3
The risk of virus transmission by donating blood or organs is related to the presence of asymptomatic carriers and the short incubation period that precedes viremia. There is insufficient data to allow an accurate estimation of the incidence of dengue transmission through transplanted organs in developing tropical countries, as diagnostic tests for detecting infected donors is not routinely performed.
This article describes four cases of solid organ recipients with signs and symptoms of dengue infection in the postoperative period following transplantation, in whom the probable transmission mechanism was the graft.
Materials and methodsThis is a description of dengue virus infection in four recipients of solid organ grafts taken from donors with dengue infection. All cases received care at Fundación Valle del Lili (FVL) in Cali, Colombia. The Institutional Committee of Ethics in Biomedical Research approved this study.
The diagnosis of dengue in donors and recipients was made by detecting IgM and IgG antibodies and antigenemia (NS1).4 In recipients, Reverse Transcriptase Polymerase Chain Reaction (RT-PCR)5 for dengue was also carried out, in the Microbiology Laboratory of the Universidad Del Valle. In 2007, a rapid chromatographic immunoassay was used for the qualitative detection of IgG and IgM antibodies against dengue virus in human blood (ACON®). In 2010, NS1Ag+AB SD BIOLINE (Standard Diagnostic®) immunochromatography test was used to detect the virus NS1 antigen and antibodies (IgM and IgG) in serum. A review of the literature on non-vectorial transmission due to organ transplantation, using Mesh terms is presented.
ResultsCases 1 and 2In 2007, cases 1 and 2 received a heart and liver transplant, respectively, from the same deceased donor, who died of an intracranial hemorrhage secondary to a hypertensive emergency in Medellin, Colombia. After the transplant, the institution that rescued the organs notified our hospital that the donor had consulted a week before his death with fever and mild thrombocytopenia. Due to the epidemic season of dengue, we tested the donor samples and were positive for dengue IgM and IgG.
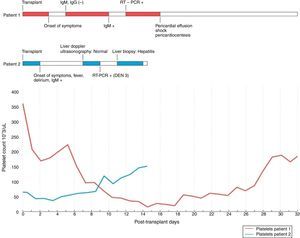
Recipient 1A 41-year-old male, was a recipient of a heart transplant due to dilated cardiomyopathy (Table 1). After transplantation, he was put on immunosuppression with methylprednisolone, cyclosporine, and mycophenolate. On the third postoperative day, the patient developed myalgia, arthralgia, and general discomfort associated with thrombocytopenia, and lymphopenia, which did not improve by decreasing the dose of mycophenolate. Subsequently, there was an elevation of transaminases, bilirubin, and alkaline phosphatase. Positive IgM for dengue was detected (Fig. 1) and RT-PCR was positive for DEN 3. On the sixteenth day after surgery, the patient developed dengue shock syndrome (DSS), severe thrombocytopenia, and a transesophageal echocardiogram showed a cardiac tamponade. A pericardiocentesis drained 1530mL of hemorrhagic fluid. Endomyocardial biopsies showed no rejection. The bacterial cultures of the pericardial fluid were negative. Three weeks after the start of these symptoms, lymphopenia, and thrombocytopenia improved, the dose of mycophenolate was increased, and the patient was discharged.
Clinical characteristics of transplanted patients with dengue virus infection.
| Patient | Donor | Age (yr)/gender | Clinical manifestations | Organ | Days of onset | Mortality | Test results |
|---|---|---|---|---|---|---|---|
| Recipient 1 | A | 41/male | Myalgia, arthralgia. Thrombocytopenia, lymphopenia DSS | Heart | 8 | Alive | IgG− IgM+ RT-PCR+ (DEN3) |
| Recipient 2 | 53/male | Fever, transient encephalopathy. Thrombocytopenia, lymphopenia, anemia. Hepatitis. | Liver | 2 | Alive | IgG− IgM+ RT-PCR+ (DEN 3) | |
| Recipient 3 | B | 31/female | Fever, vomiting, diarrhea, jaundice. Thrombocytopenia, lymphopenia. Hepatitis. | Kidney | 8 | Alive | IgG+IgM+ NS1+RT-PCR+ (DEN4) |
| Recipient 4 | 48/female | Fever | Kidney | 4 | Alive | IgG− IgM+ NS1− PCR− | |
| Donor A | – | 40/male | Mild fever, thrombocytopenia, lymphopenia | – | – | Death intracranial hemorrhage | IgM+ IgG+ |
| Donor B | – | 32/male | Asymptomatic | – | – | Death traumatic brain injuries | IgG− IgM− NS1+ |
+, Positive result; −, Negative result; CRD, chronic kidney disease; DSS, dengue shock syndrome.
A 53-year-old male, had undergone liver transplantation without complications. We initiated immunosuppression with methylprednisolone, cyclosporine, and mycophenolate after surgery. Two days post-transplant the patient presented fever, anemia, lymphopenia, thrombocytopenia, and alteration of liver function tests. Subsequently, he developed transient encephalopathy. The initial tests for dengue were positive for IgM and negative IgG. RT-PCR was positive for serotype DEN 3. During hospitalization, the transaminase levels fell, but the bilirubin and alkaline phosphatase increased until day 14, and the platelet count showed a tendency to increase on day 10 (Fig. 1). Blood and urine cultures were negative. Graft thrombosis and obstruction of the bile duct were ruled out using Doppler ultrasound and endoscopic retrograde cholangiopancreatography respectively. The liver biopsy found lymphoplasmacytic inflammatory infiltrate, neutrophils, and cholestasis. The diagnosis was of acute hepatitis due to dengue. The immunosuppression regimen was not changed. The patient was discharged at day 14 post-transplant.
Cases 3 and 4Cases 3 and 4 were recipients of a kidney transplant in May 2010, from the same deceased donor, who passed away due to a severe traumatic brain injury. Due to the diagnosis of dengue in recipient 3, serum from the donor was tested post-transplant, detecting a positive dengue antigen NS1.
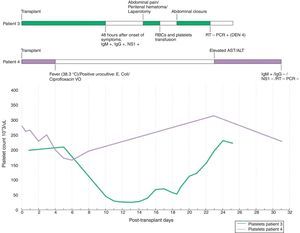
Recipient 3A 31-year-old female, with chronic renal failure, received a kidney transplant with no complications (Table 1). We started immunosuppression with prednisolone, cyclosporine, and mycophenolate sodium after transplantation. The patient was discharged on the fifth post-transplant day. On the eighth day post-transplant, she was readmitted with fever, vomiting, diarrhea, and jaundice. The patient presented pain in the right iliac fossa, anemia, and thrombocytopenia. An ultrasound at day 15 after transplantation showed a perirenal hematoma of 1300mL, which was drained. Laboratory tests showed thrombocytopenia, leukopenia, and lymphopenia with an elevation of transaminases, bilirubin, and LDH, with no alterations in renal function. The patient required transfusion of red blood cells, platelets, and fresh frozen plasma. The serology for cytomegalovirus and toxoplasma antibodies were negative. IgG, IgM, and the dengue NS1 antigen were positive, and subsequently RT-PCR (serotype DEN 4) was also positive. Severe dengue was diagnosed, due to hepatitis and major hemorrhagic manifestations. The patient was discharged after 25 days and continued outpatient follow-up with satisfactory evolution (Fig. 2).
Recipient 4A 48-year-old female who received a kidney transplant with no complications. She was started on immunosuppressive treatment via prednisolone, cyclosporine, and mycophenolate sodium. On the fourth day post-transplant, she developed fever, associated with mild anemia but with no other hematological alteration. Bacterial culture of blood and peritoneal fluid were negative. Escherichia coli was isolated in a urine culture, and the patient received treatment with oral ciprofloxacin. At day 23 post-transplant, the patient was asymptomatic, with an elevation of transaminases. Due to the history of dengue in recipient 3, who had also received a kidney from the same donor, diagnostic tests were performed, which were positive for IgM and negative for IgG, NS1, and RT-PCR (Fig. 2). During the outpatient follow-up, the patient became asymptomatic, with adequate functioning of the graft and normalization of the liver profile.
DiscussionHerein we reported a series of highly probable donor transmission of dengue in four solid organ transplant recipients. Dengue infection in an early postoperative period could be a major challenge for infectious diseases physicians due to the possible vectorial and non-vectorial transmission. We will briefly discuss this differentiation.
Vectorial versus non-vectorial transmission of dengueDengue virus is an RNA virus with four described serotypes widely distributed in tropical regions where A. aegypti is endemic.6 In recent years the American region has become a hyperendemic area for dengue. This infection has an incubation period of 7–14 days, and most of the infected patients have mild symptoms or are asymptomatic (78%). In hyperendemic areas, potential recipients could get infected before their transplant, and those patients will develop dengue in an early stage after transplantation. In those cases, no other recipients of the same donor will get this infection. In contrast, in this hyperendemic regions potential donors could get infected prior organ procuration and could transmit the dengue virus to the recipient. In these cases, other recipients from the same donor will more likely present with early dengue infection.
Multiples forms of non-vectorial transmission have been reported: blood products, solid organ transplant, bone marrow, and nosocomial transmission through a contaminated needle stick.7–9 Dengue infection due to blood products is probably the most reported non-vectorial infection, with a clinical spectrum similar to a vectorial transmission, although, most of these infections are underreported even in endemic countries like Brazil and Puerto Rico.7 Recently, the American Association of Blood Banks and the Centers of Diseases Control and Prevention have recommended the screening of blood products for dengue in endemic countries.10 However, this recommendation is not included in the guidelines for organ transplant of the American Society of Transplantation. Nosocomial transmission has been reported through needlestick injury from dengue infected patients.11 Cases of vectorial transmitted dengue have been reported as nosocomial acquired infection as well, in endemic countries such as Brazil and India, with some papers reporting the presence of the vector inside the Hospital.12,13
Non-vectorial transmission of dengue due to infected donors have rarely been reported.8 There have been limited descriptions of possible non-vectorial transmission of dengue through solid organ transplant (SOT).14 The majority of reports are classified as possible transmission due to lack of viral PCR confirmation in the donor. None of these cases reported have more than one recipient infected from the same donor. Therefore, a vectorial infection prior transplant cannot be ruled out. A summary of all cases reported is presented in Table 2. To our knowledge, our report is the first to describe more than one recipient infected from the same donor and is also the largest. A central clue to suspect transmission through an infected donor, besides viral PCR5 confirmation in the donor, is the presence of more than one recipient infected by the same donor. Simultaneously vectorial infection in more than one recipient of the same donor would be very improbable.
Dengue transmission through transplantation of an infected organ.
| Authors | Age | Organ | Days of onset | Symptoms | Mortality | Test recipient | Test donor |
|---|---|---|---|---|---|---|---|
| Gupta et al.20 | 40 | Liver | 2 | Fever, thrombocytopenia | Alive | NS1+ | NS1+ |
| Lanka et al.17 | 51 | Bone Marrow | 3 | Fever, thrombocytopenia, hematochezia | Decease (enterocolitis) | IgM/IgG− NS1+ PCR (DEN1) | IgM/IgG+ NS1+ PCR (DEN1) |
| Tan et al.9 | 23 | Kidney | 5 | Fever, thrombocytopenia, Gi bleeding, hematuria | Alive | PCR+ (DEN 1) | No test reported |
| Present Study Case 1 | 41 | Heart | 8 | Fever, thrombocytopenia, shock | Alive | IgM+ IgG− PCR (DEN3) | IgM+ IgG+a |
| Present Study Case 2 | 53 | Liver | 2 | Fever, thrombocytopenia, anemia, hepatitis | Alive | IgM+ IgG− PCR (DEN3) | |
| Present Study Case 3 | 31 | Kidney | 8 | Fever, thrombocytopenia, diarrhea, hepatitis | Alive | IgM+ IgG+ NS1+ PCR+ (DEN4) | IgM− IgG− NS1+b |
| Present Study Case 4 | 48 | Kidney | 4 | Fever | Alive | IgM+ IgG− NS1− PCR− |
PCR, polymerase chain reaction; NS1, non-structural protein 1; DEN, dengue serotype.
The clinical spectrum of vectorial dengue in transplant recipients is broad, with some studies suggesting that there is a similarity to the non-transplanted population.15,16 In the possible organ transmission, more severe cases have been reported.17Table 2 summarizes the most important clinical manifestations of the cases that have been reported. All patients develop symptoms during the first week post-transplant. Fever and thrombocytopenia were the most frequent findings. Fatal cases have been reported, one kidney and one bone marrow transplants. In our series, non-fatal cases were presented. Two recipients presented severe manifestations, namely severe postoperative hemorrhage in a kidney recipient and dengue shock syndrome in a cardiac recipient. Regardless of the immunosuppression status, severe dengue could be more frequent in acute secondary infections, which are more probable in tropical areas where these patients are likely exposed to multiple serotypes of the virus.6
There are no reports of graft rejection among dengue infected cases. In our series, patients were followed up for more than one year with no humoral or cellular significant changes and maintained the immunosuppressive dose.
Screening organ donors for dengue infection in hyperendemic regionsAs previously stated, routine screening for dengue is not recommended by the American Society of Transplantation guidelines. On the other hand, it has been just recently recommended by both the American Association of Blood Banks and by the Centers of Diseases Control and Prevention guidelines. Few dengue infected organ transmissions have been reported as this arbovirus was not in the scope of donor related infections. However, an increase in dengue cases and the risk of another recent arbovirus, such as Zika and Chikungunya could be a significant threat in organ donation. Screening for dengue could be available through rapid test detecting NS1 antigen. This antigen is highly preserved through the different dengue serotypes and can be detected before clinical manifestations develop. In most tropical regions, this rapid test is available in combination with IgM/IgG antibodies. The low cost of this test could facilitate the screening in transplant programs. Viral PCR confirmation5 is not available on regular basis in most tropical countries.
Worldwide PCR availability for the diagnosis of dengue is very low,5 but some rapid tests are inexpensive and can be easily done. The turnaround time for having the results of NS1 Ag and IgG/IgM tests is 15–20min with very high sensitivity and specificity in primary infections. (NS1: Sens 92% Spec: 98%; IgG/IgM Sens: 94% Spec: 96%) However, in the secondary infections the sensitivity can decrease to 80%.18
In areas where dengue is endemic, the ability to run low-cost and high-performance tests, such as the antigen NS1 test,4,19 during outbreaks, could allow the detection of organ donors who are asymptomatic carriers of the virus.20 Early detection in donors could prevent late recipient infections, and could modify clinical management reducing complications and mortality. Our institution decided to screen all donors during outbreak season only because our cases occur during this outbreak periods.
More studies are required to accurately recommend routine screening organ donors for dengue virus in hyperendemic regions during outbreaks and to establish cost-effectiveness, so the pool of donors is not reduced with this additional testing.
Should we use organs from infected donors?The decision to use organs from infected donors has been controversial and must be based on case-by-case estimating the risk/benefit ratio. In our review of the reported possible donor infections most authors did not reach to any definitive conclusion on this subject. Some authors suggest to screen for dengue infection during outbreak periods21 but do not give any recommendation regarding organ use. Other authors recommend that organs could be used in individual case analysis.9
In our own experience we have excluded patients with positive NS1 antigen but not with positive antibodies and negative antigen. Since we started this screening strategy, we did not have any new dengue recipients infected due to organ transplant. Based on our experience and the cases reported, a screening method at low cost could be feasible. In our review, fatal cases have occurred in less than 20% of patients. Nevertheless, support measurements can be effective in reducing dengue mortality and complications.
Dr. Beatriz Parra, chief of the Virology Laboratory, Department of Microbiology, Universidad del Valle, Cali, Colombia.