To evaluate the clinical effects of blood purification for treating fulminant hepatic failure (FHF).
MethodsThirty-three severe FHF patients with hepatic encephalopathy (HE) above grade III were subjected to a combined blood purification treatment in addition to the comprehensive liver protection therapy. Patients underwent continuous hemofiltration on a daily basis during the daytime followed by sequential treatment with plasma exchange or hemodialysis every 2–3 days. The therapeutic effects of this treatment were evaluated.
ResultsAfter treatment with blood purification, restoration of consciousness (those who abandoned the treatment without restoration of consciousness were excluded) was achieved in 6 of 8 cases (75%) in acute liver failure (ALF) group, 3 of 3 cases (100%) in subacute liver failure (SALF) group, and 9 of 14 cases (64.29%) in acute/subacute on chronic liver failure (A/SCLF) group. Of all cases, 11 patients restored consciousness after 7 days in a coma. The rate of long-term survival (those who abandoned the treatment were excluded) was 3/7 (42.86%) for ALF group, 2/2 (100%) for SALF group, and 1/11 (9.09%) for A/SCLF group. The levels of hemoglobin and platelet in peripheral blood were significantly reduced after blood purification.
ConclusionsTreatment of FHF patients with daily continuous hemofiltration during the daytime is effective in treating HE and in improving health status in the early stages of the disease. Long-term prognosis also benefits from this treatment. The rate of consciousness recovery and long-term survival is highest in SALF group followed by ALF group. This treatment is less effective in A/SCLF patients. It should be noted that blood purification procedure may cause damage to blood cells.
In clinical practice, fulminant hepatic failure (FHF) begins with acute liver failure, subacute liver failure, or acute/subacute on chronic liver failure. Because FHF causes mass cell death and severe damage to liver function, patients with FHF develop hepatic encephalopathy above grade II in early stages. The illness progresses rapidly, and patients usually die from multiple organ failure if immediate and effective treatment is not available. In this study, we treated FHF patients with daily continuous hemofiltration, followed by sequential plasma exchange or hemodialysis every 2–3 days in addition to a comprehensive liver protection therapy, and achieved positive outcomes.
Subjects and methodsSubjectsThirty-three FHF patients with HF above grade III in early stages were recruited for this study. These patients were admitted to the hospital from October 2006 to May 2011. This study was conducted in accordance with the declaration of Helsinki and approved by the Ethics Committee of No. 5 People's Hospital of Wuxi. Written informed consent was obtained from all participants. According to the diagnostic standards described in the “Diagnostic and treatment guidelines for liver failure”1 (by the Chinese Society of Infectious Diseases and Chinese Society of Hepatology, Chinese Medical Association), 8 patients were diagnosed with ALF, 5 with SALF, and 20 with A/SCLF. There were 29 patients with hepatitis B virus infection, 1 with Hepatitis E virus infection, and 3 patients with unknown etiology; 18 were male and 15 female; age ranged from 23 to 65.
MethodsWhen symptoms of HE appeared, the patients were treated with blood purification as soon as possible until the restoration of consciousness. The modes of blood purification used in this study were as follows:
Daily continuous hemofiltration: YF-70PAN membrane (area 0.7m2) was used as a hemofilter. Port solution2 was used as replacement fluids. The concentration of KCl in the replacement fluids was adjusted according to blood potassium concentration. All solutions except for bicarbonate were loaded into the infusion bag, and transferred in synchrony. The replacement fluids were transferred by a pre-dilution method. Blood flow rate was 150–200ml/min. For anticoagulation, an initial dose of 2000–4000U low-molecular-weight heparins was used, followed by 4–20U/min standard heparin. The additional heparins were omitted for those who had severe bleeding. In case of fever, the temperature of blood replacement fluids was adjusted to around 35°C. The volume of ultrafiltrate was determined by the condition of chemosis and other clinical features of the patients. The treatment lasted for 6–8h each day.
Plasma exchange: IQ blood purification instrument and MicroPES plasmacureunit were used for plasma exchange. The total volume of plasma exchanged was 1800–2400ml. The rate of plasma separation was 30ml/min. Fresh cold plasma of the same type was used as the replacement fluid.
Hemodialysis: MicroPES A2 plasmacureunit and YF-70PAN plasmacureunit were used. The volume for each exchange was 1600–2000ml. Port solution was used for hemodialysis.
Continuous hemofiltration at daytime was the main purification method and administered daily. Every 2–3 days, patients underwent sequential plasma exchange or hemodialysis. During blood purification treatment, comprehensive liver protection therapy was performed to protect liver cells and prevent complications. Delivery of 200–400ml human serum albumin and/or fresh frozen plasma by an intravenous drip was given as support treatment. Patients with a positive hepatitis B virus test were treated with antiviral therapy using nucleotide analogs.
Statistical analysisThe t test was used to determine whether there was a significant difference between two group means. Differences of enumeration data were compared with χ2 test. Statistical significance was defined by p<0.05.
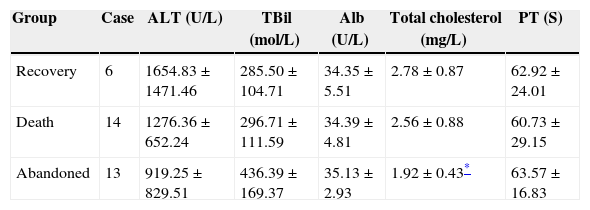
ResultsEvaluation of liver function in patientsThe patients we analyzed had severe FHF. There was serious damage to the liver function. Prothrombin activity in all patients was less than 30%, and even less than 10% in some cases. According to the clinical outcome after blood purification treatment, patients were divided into three groups: recovery group (discharged from hospital with liver function restored to normal), death group (died in hospital), and abandoned group (abandoned treatment and discharged from hospital with no significant improvement in liver function). As shown in Table 1, only total cholesterol level in abandoned group was lower than in recovery and death groups. There was no significant difference in other indexes, suggesting that liver function in all patients was comparable at the time of admission to the hospital.
Liver function before blood purification (x±s).
| Group | Case | ALT (U/L) | TBil (mol/L) | Alb (U/L) | Total cholesterol (mg/L) | PT (S) |
|---|---|---|---|---|---|---|
| Recovery | 6 | 1654.83±1471.46 | 285.50±104.71 | 34.35±5.51 | 2.78±0.87 | 62.92±24.01 |
| Death | 14 | 1276.36±652.24 | 296.71±111.59 | 34.39±4.81 | 2.56±0.88 | 60.73±29.15 |
| Abandoned | 13 | 919.25±829.51 | 436.39±169.37 | 35.13±2.93 | 1.92±0.43* | 63.57±16.83 |
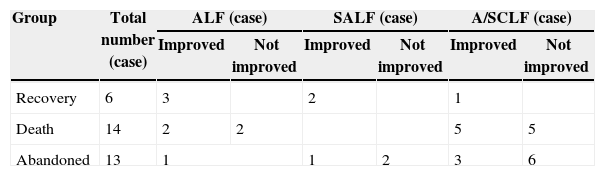
After blood purification, significant improvement was achieved and consciousness was completely restored in 18 FHF patients with HE. However, some patients despite improving eventually died. The clinical outcome of blood purification in treatment of severe FHF is shown in Table 2.
The rate of consciousness recovery (patients who abandoned treatment while still in a coma were excluded) in all patients was 72% (18/25). It was 75% in ALF group, 100% in SALF group, and 64.29% in A/SCLF group. The recovery rate in A/SCLF group was much lower than that in ALF and SALF groups (p<0.01). Long-term survival rate calculated according to the number of patients who were discharged from the hospital with restored liver function (those who abandoned treatment were excluded) was 42.86% in ALF group, 100% in SALF group, and 9.09% in A/SCLF group. The survival rate in A/SCLF group was much lower than that in ALF and SALF groups (p<0.05).
Hospitalization and blood purification of the recruited patientsAmong the 33 patients with severe FHF, 11 suffered from HE for 7 days. Of patients who died after restoration of consciousness, 3 received blood purification for more than 10 times and 4 survived for more than 30 days.
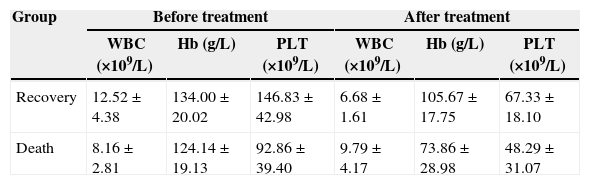
Comparison of peripheral blood cells before and after blood purification in patients who restored consciousnessTable 3 showed that the levels of hemoglobin and platelet were markedly reduced in either recovery group or death group after blood purification. The amount of platelets was already much lower in death group before treatment. The amount of hemoglobin was decreased more prominently in death group than recovery group after treatment.
Results of standard test for peripheral blood cells before and after blood purification (x±s).
| Group | Before treatment | After treatment | ||||
|---|---|---|---|---|---|---|
| WBC (×109/L) | Hb (g/L) | PLT (×109/L) | WBC (×109/L) | Hb (g/L) | PLT (×109/L) | |
| Recovery | 12.52±4.38 | 134.00±20.02 | 146.83±42.98 | 6.68±1.61 | 105.67±17.75 | 67.33±18.10 |
| Death | 8.16±2.81 | 124.14±19.13 | 92.86±39.40 | 9.79±4.17 | 73.86±28.98 | 48.29±31.07 |
Three patients had severe hematoma resulting from local damage caused by venipuncture. Of these patients, two were in death group. One died without restoration of consciousness.
DiscussionThe mortality rate in FHF patients with HE is more than 85%.3–5 Immediate and proper treatment of these patients is critical to achieve a successful salvage, which is worthy of further investigation.
In FHF patients, HF occurs rapidly. Encephaledema is the main cause for HE6 and is also a major determinant for survival. When patients are suffering from liver failure, metabolism slows down, and blood ammonia and other toxicants accumulate in the body. It is reported that the mortality rate of encephaledema or cerebral hernia in ALF patients is correlated with the levels of artery blood ammonia.7 Patients with liver failure are also accompanied by severe infection. Infection and its induced inflammatory mediators such as TNF-α, IL-1, and IL-6 enhance the disturbance caused by high blood ammonia.8
Electrolyte and acid–base balances in patients with HE are often disturbed,9 which complicates the disease. Therefore, disturbance of internal environment occurs in patients with severe FHF. It is important to improve the internal environment. Continuous hemofiltration is the most effective treatment to achieve rapid improvement of the disturbance of internal environment. On one hand, it can eliminate blood ammonia, inflammatory factors, and other toxic substances,10 in addition to restoring the function of damaged endothelial cells in patients with pyaemia to alleviate the severity of the illness, and maintain water electrolyte and acid–base balance.11 On the other hand, it can also relieve encephaledema and stabilize the internal environment of patients.11
FHF patients with severe HE above grade III underwent sequential plasma exchange or hemodialysis every 2–3 days in addition to routine continuous hemofiltration performed on daytime for 6–8h to eliminate macromolecular protein-binding toxins and to supplement bioactive substances that the body needs such as blood coagulation factors. The use of continuous hemofiltration at daytime instead of discontinuous hemofiltration for 24h has several advantages. It can effectively eliminate toxic substances and meanwhile reduce the loss of therapeutic drugs that have protective effects on cell membranes, promoting liver cell growth, and anti-infection. This mode of treatment also helps patients to change body position and to prevent the corresponding complications. This combined method of blood purification significantly improved the clinical outcome of FHF patients and achieved in a 72% restoration of consciousness in patients with grade III or IV severe HE. This suggested a good life-supporting effect and fairly high rate of successful salvage. We observed that FHF patients with severe HE were often in a coma for a long time. Among them 61.11% were in a coma for 7 days. However, these patients restored consciousness through the combined blood purification. Thus, the time for treatment and persistence on the use of daily blood purification until recovery are critical. We also found that treatment with blood purification for more than 10 times had no apparent effects on the improvement of long-term prognosis.
After treatment with the combined blood purification therapy, 6 patients fully restored liver function and discharged from hospital, suggesting that this treatment not only extends life, but also promotes the survival of FHF patients. The mortality rate of these patients is less than that reported in literature.
We observed that the rate of consciousness recovery and long-term survival after the combined blood purification therapy was highest in SALF group followed by ALF group. It was much lower in A/SCLF group compared to the other two groups. In patients who died after restoration of consciousness, four of them survived for more than 30 days. Furthermore, additional treatment did not improve the prognosis of these patients. The amount of platelet in these patients was less than that in those who completely recovered and were discharged from hospital. Furthermore, after the treatment reduction in the level of hemoglobin was also more significant in death group than recovery group. These results indicate that the clinical outcome in patients treated with the combined blood purification is influenced by the condition of liver function, technique of the treatment, and the management of complications.
We found that the levels of hemoglobin and platelet were significantly decreased in both recovery group and death group after blood purification, suggesting that this treatment can cause mechanical damage to peripheral blood cells. Three patients had severe hematoma resulting from local damage caused by venipuncture. Therefore, it is important to reduce side effects during treatment.
In summary, continuous hemofiltration on a daily basis during daytime combined with sequentially treatment with plasma exchange or hemodialysis every 2–3 days are effective in treating patients with FHF.
Conflict of interestThe authors declare no conflict of interest.