This study evaluated the impact of urinary incontinence (UI) on sexuality, body image, mood, and quality of life of patients with myyelopathy associated with HTLV-1/tropical spastic paraparesis (HAM/TSP). The sample consisted of 31 HAM/TSP outpatients, of both sexes, followed-up at the Emílio Ribas Infectology Institute. The following instruments were used: sociodemographic questionnaire, Hospital Anxiety and Depression Scale (HAD), Body Image Assessment Scale, Sexual Quotient Female (QS-F) and Male (QS-M) Versions, King's Health Questionnaire (KHQ), and Revised OSAME Motor Disability Score. Data analysis was performed using descriptive statistics and the Mann–Whitney U-test was used for group comparison. The presence of UI was reported by 13 (41.9%) patients. Based on the quality of life questionnaire, patients with UI had a significant impact in the following domains: incontinence impact, daily life activities limitation, physical and social limitations, social relations, emotions, sleep and disposition, and severity measurements. Most participants had no anxiety (21; 67.7%) or depression symptoms (18; 58.1%). Regarding the sexual coefficient, 13 (41.9%) participants had sexual dissatisfaction. Conclusion: UI is common in HTLV-1 patients and may cause serious impairment in quality of life, with social, psychological and hygienic consequences. Nonetheless, there are few studies on this subject and their impact on mood and sexuality.
Myelopathy associated with HTLV-1/tropical spastic paraparesis (HAM/TSP) is characterized by insidious and progressive involvement of muscle weakness in the lower limbs and spasticity, associated in different degrees with sphincter and sensory disorders, which can occur in approximately 5% of patients with HTLV-1.1 HAM/TSP is a chronic and slowly progressive inflammatory myelopathy that may lead to severe neurological disability. It is characterized by muscle weakness, hyperreflexia, lower extremity spasticity, and urinary disturbance. The prevalence of erectile dysfunction in the absence of HAM/TSP varies between 4 and 43% in the literature.2 Urological manifestations are present in up to 90% of the myelopathy cases, characterized by increased frequency, urgency, and urinary incontinence (UI).1 Such manifestations may be an important sign of disease progression and may be indicative of myelopathy.2,3
Women with UI, secondary to HTLV, differ from other types of incontinence, as well as other urinary symptoms, such as perineal hypersensitivity, pain on vaginal palpation, and pelvic floor muscle hypertonia. Painful bladder filling and dyspareunia are also prevalent in HTLV-infected women, in addition to other neuromotor abnormalities that also significantly compromise daily activity, including sexual, self-care, sleep and disposition, which further aggravate the exercise of sexuality.4,5
In the early stages of HTLV-1 infection, storage symptoms such as nocturia, urgency, and urgency with incontinence are more frequent. In more advanced stages, the presence of neurogenic bladder can lead to urinary symptoms such as dysuria, hesitation, effort to urinate, and incomplete emptying sensation. In HAM/TSP patients, the most reported urinary symptoms are nocturia (81.4%), involuntary loss of urine (76.9%), urgency (74.4%), frequency increase (60.5%), and dysuria (39.5%).3 In addition to UI, erectile dysfunction is frequently observed in HTLV-1-infected male patients, with or without myelopathy. Urinary tract infection also has a high prevalence in these patients.6
According to Castro (2005),5 the prevalence of erectile dysfunction (ED) is high in HTLV-I-infected patients, and progressively increases according to the degree of neurological disability. Many factors may also influence erectile function of patients with HAM/TSP, such as functional limitation, reduced self-esteem due to stigma of myelopathy, fear of transmitting the disease to uninfected partners, UI, use of medications for pain control, and other chronic diseases. ED itself reduces the sexual frequency of these patients and sometimes the libido. The lack of specific studies on ED in patients with HAM/TSP makes it difficult to know clearly its pathophysiology, although it has been suggested that the neuronal injury that induces myelopathy also interferes in the conduction of the nerve stimuli at the medullary level, determining the IU.6
HAM/TSP is associated with issues related to the exercise of sexuality, personal losses and death, resulting in physical and psychological conflicts. Therefore, there is a growing concern about the effects these symptoms may cause in these patients, especially with regard to their quality of life.7 Therefore, considering the impact UI can cause and the scarce literature on the subject, the main objective of this study was to assess the impact of UI on sexuality, body image, mood, and quality of life of patients.
MethodsA cross-sectional descriptive study was performed from August to November 2016. Among the 100 active individuals in this cohort, 50 were approached, and 31 adult HTLV-1 infected patients with HAM/TSP accepted to participate in this study. Patients were invited to participate in the study on the day of the medical consultation and those who accepted to participate were referred interviewed in a private room at the clinic using standardized questionnaires described below. The average time for data collection was 30 min. The eligibility criteria were: 18 years of age or older, of both sexes, and outpatients receiving care at the Emílio Ribas Institute of Infectology, and aware of their diagnosis. Patients with HCV and/or HIV co-infection were excluded.
InstrumentsSeven questionnaires were used: a socio-demographic questionnaire, Hospital Anxiety and Depression Scale (HAD),8 Body Image Measurement Scale,9 Sexual Quotient Female (QS-F) and Male (QS-M) versions,10–12 King’s Health Questionnaire (KHQ),13 Revised Motor Disability Scale (OSAME),14 and ICIQ-SF.15
After processing, the results were organized into tables and cross-tabulated into two variables when suitable. Percentages and average values were used according to the variable analyzed. Data analysis was performed using SPSS version 16 for Windows. Results are presented as mean, absolute and relative frequencies. Mann–Whitney U-test was used to compare groups. The significance level was set at 0.05 (alpha = 5%).
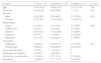
ResultsThe sample consisted of 21 (67.5%) women, average age 51.65 years (SD = 9.53), predominantly married (17; 54.8%), and average schooling time of 8.23 (SD = 4.04) years. Of the 31 participants, 18 (58.06%) had UI and 13 (41.93%) had no symptoms of urine leakage. Table 1 shows the demographic and clinical characteristics of the participants according to the presence of UI.
Sociodemographic and clinical data of the studied sample according to the presence of urinary symptoms.
| Variable | Total (n = 31) | UI present (n = 18) | UI absent (n = 13) | p-Value |
|---|---|---|---|---|
| Age | 51.65 (9.53) | 50.88 (2.47) | 51.31 (2.19) | 0.87 |
| Schooling | 8.23 (4.04) | 8.53 (0.98) | 7 (1.15 ) | 0.65 |
| Gender | ||||
| Male | 10 (32.3%) | 8 (44.44%) | 2 (15.38%) | 0.09 |
| Female | 21 (67.5%) | 10 (55.55%) | 11 (84.61%) | |
| Marital status | ||||
| Single | 4 (12.9%) | 2 (11.11%) | 2 (15.38%) | 0.98 |
| Stable union | 2 (6.5%) | 1 (5.55%) | 1 (7.69%) | |
| Married | 17 (54.8%) | 10 (55.55%) | 7 (53.84%) | |
| Divorced | 3 (9.7%) | 1 (5.55%) | 2 (15.38%) | |
| Widow(er) | 5 (16.1%) | 4 (22.22%) | 1 (7.69%) | |
| Occupation | ||||
| Employed | 7 (22.6%) | 5 (27.77%) | 2 (15.38%) | 0.24 |
| Unemployed | 8 (25.8%) | 4 (22.22%) | 4 (30.76%) | |
| Social security leave | 1 (3.2%) | 1 (5.55%) | 0 | |
| Retired due to disability | 4 (12.9%) | 4 (22.22%) | 0 | |
| Retired due to service time | 4 (12.9%) | 2 (11.11%) | 2 (15.38%) | |
| Housewife | 7 (22.6%) | 2 (11.11%) | 5 (38.46%) | |
The mean time of HTLV-1 infection diagnosis was 10.71 years (SD = 5.24), most of the participants (n = 26; 83.9%) rely on people who help them on a day-to-day basis and with treatment, mostly first-degree relatives (n = 21; 80.8%). The average time of UI was 5.72 years (SD = 5.17). Table 2 presents data related to diagnosis time and social support.
Data related to diagnosis time and social support on the studied sample according to the groups with and without urinary symptoms.
| Total (n = 31) | UI present (n = 18) | UI absent (n = 13) | p-Value | |
|---|---|---|---|---|
| Time of HTLV-1 diagnosis (years) | 10.71 (5.24) | 10.78 (1.17) | 10.62 (1.61) | 0.93 |
| Have someone to assist | ||||
| Yes | 26 (83.9%) | 14 (77.77%) | 12 (92.30%) | |
| No | 5 (16.1%) | 4 (22.22%) | 1 (7.69%) | |
| If so, who? | ||||
| 1st degree relatives | 21 (80.8%) | 10 (55.55%) | 11 (84.61%) | |
| (n = 26) 2nd degree relatives | 1 (3.2%) | 1 (5.55%) | 0 | |
| Caregiver | 4 (15.4%) | 3 (16.66%) | 1 (7.69%) | |
| Time of urinary incontinence (years) | 5.72 (5.17) | |||
| Catheter utilization | ||||
| Yes | 9 (50%) | |||
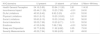
Out of the 18 patients with UI, nine (50%) reported having urine leakage once a week, mostly small volume (13; 72.2%), more frequently before arriving in the bathroom (12; 66.6%). Table 3 describes the answers to questions of the ICIQ-SF questionnaire.
Answers to the ICIQ-SF questionnaire of patients with urinary symptoms.
| ICIQ-SF | N (18) |
|---|---|
| Urine loss frequency | |
| Once a week | 9 (50.00%) |
| Once a Day | 2 (11.11%) |
| Several times a Day | 3 (16.66%) |
| All the time | 4 (22.22%) |
| Volume of urine lost | |
| Small | 13 (72.22%) |
| Moderate | 3 (16.66%) |
| Large | 2 (11.11%) |
| Interferes with quality of life | 2.52 (3.22) |
| Total | 5.55 (5.84) |
| Urine loss | |
| Before getting to the bathroom | 12 (66.66%) |
| When coughing or sneezing | 6 (33.33%) |
| Sleeping | 4 (22.22%) |
| While performing physical activities | 1 (5.55%) |
| When finishing urinating and getting dressed | 1 (5.55%) |
| No obvious reason | 1 (5.55%) |
| All the time | 3 (16.66%) |
All 18 participants with UI were diagnosed with neurogenic bladder, 11 (61.11%) had effort incontinence, three (16.66%), and urgency (n = 6, 33.33%) combined with incontinence (n = 9, 50%); 14 (77.77%) reported painful bladder; 15 (83.33%) reported losing urine during sexual intercourse, and the 18 patients used some type of hygienic protector, had to change their underwear when feeling wet, control the amount of ingested fluid, and worry about urine odor.
Regarding the quality of life questionnaire, UI had a significant impact in the following domains: incontinence impact, limitation of DLAs (daily life activities), physical and social limitations, social interactions, emotions, sleep and disposition, and severity measurements. Table 4 shows the comparison of average scores of KSH domains in patients with and without UI.
Quality of life scores according to the presence of urinary symptoms.
| KHQ domains | UI present | UI absent | p-Value | U Mann–Whitney |
|---|---|---|---|---|
| Health General Perception | 54.16 (5.80) | 53.84 (11.26) | 0.91 | 114.50 |
| Incontinence Impact | 65.44 (11.26) | 10.23 (7.89) | <0.01 | 24.00 |
| DLAs Limitations | 40.50 (8.42) | 8.92 (5.20) | <0.01 | 53.00 |
| Physical Limitations | 50.61 (8.13) | 19.23 (10.65) | 0.11 | 56.00 |
| Social Limitations | 50.60 (8.10) | 19.33 (10.64) | 0.01 | 56.00 |
| Social Interactions | 33.05 (7.69) | 10.23 (6.71) | 0.10 | 55.50 |
| Emotions | 41.55 (9.06) | 7.69 (7.69) | <0.01 | 52.50 |
| Sleep and Disposition | 33.77 (8.29) | 11.92 (6.82) | 0.05 | 73.00 |
| Severity Measurements | 43.22 (7.64) | 12.69 (6.25) | 0.01 | 49.00 |
DLAs, daily life activities.
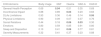
Most participants (21; 67.7%) had no symptoms of anxiety or depression (18; 58.1%). Regarding sexual coefficient, most participants presented null-bad scores (13; 41.9%). Table 5 shows the results of mood, body image, and sexual coefficient scales.
Depression, anxiety, body image, and sexual coefficient according to the presence of urinary symptoms.
| Scales | Total (n = 31) | UI present (n = 18) | UI absent (n = 13) | p-Value | U Mann-Whitney |
|---|---|---|---|---|---|
| HAD – Anxiety | 7.00 (3.67) | 6.05 (0.85) | 8.23 (1.00) | 0.10 | 72.00 |
| Yes | 10 (32.3%) | 3 (16.66%) | 7 (53.84%) | ||
| No | 21 (67.7%) | 15 (83.33%) | 6 (46.15%) | ||
| HAD – Depression | 7.13 (4.73) | 7.29 (1.23) | 6.92 (1.23) | 0.88 | 107.00 |
| Yes | 13 (41.9%) | 7 (38.88%) | 6 (46.15%) | ||
| No | 18 (58.1%) | 11 (61.11%) | 7 (53.84%) | ||
| Body Image | 90.03 (17.87) | 92.61 (3.58) | 86. 46 (5.86) | 0.49 | 100.00 |
| Sexual coefficient | 39.64 (36.12) | 42.27 (8.40) | 36.00 (10.51) | 0.68 | 107.00 |
| Good – Excellent | 7 (22.6%) | 5 (27.77%) | 2 (15.38%) | ||
| Regular – Good | 3 (9.7%) | 1 (5.55%) | 2 (15.38%) | ||
| Unfavorable – Regular | 4 (12.9%) | 2 (22.22%) | 2 (15.38%) | ||
| Bad – Unfavorable | 4 (12.9%) | 4 (22.22%) | 0 | ||
| Null – Bad | 13 (41.9%) | 6 (33.33%) | 7 (53.84%) | ||
Analyzing the body image, sexual coefficient, mood (depression and anxiety) and Osame revised motor scale questionnaires and the different domains of the quality of life questionnaire, a higher degree of disability in the Osame scale influenced the impact of incontinence, social relations, sleep and disposition domains. Additionally, a low score in the sexual coefficient was associated with worse general health perception; high score in the depression scale was associated with increased daily life activities limitation; and finally, high score in the anxiety scale was associated with worsening social relations. Table 6 shows the correlations between the scales and the KHQ domains.
Pearson's correlation between body image, sexual coefficient, mood and motor (Osame) scales, and the KHQ questionnaire domains according to the presence of urinary symptoms.
| KHQ domains | Body image | QSF | Osame | HAD-A | HAD-D |
|---|---|---|---|---|---|
| General Health Perception | 0.69 | 0.04 | 0.51 | 0.35 | 0.69 |
| Incontinence Impact | 0.88 | 0.89 | 0.03 | 0.23 | 0.63 |
| DLAs Limitations | 0.93 | 0.36 | 0.46 | 0.14 | 0.06 |
| Physical Limitations | 0.90 | 0.09 | 0.07 | 0.37 | 0.76 |
| Social Relations | 0.44 | 0.18 | 0.06 | 0.03 | 0.30 |
| Emotions | 0.80 | 0.59 | 0.85 | 0.91 | 0.80 |
| Sleep and Disposition | 0.10 | 0.41 | 0.06 | 0.77 | 0.81 |
| Severity Measurements | 0.32 | 0.41 | 0.37 | 0.23 | 0.88 |
Urinary incontinence is a common condition in patients with HAM/TSP and one that can cause serious impairment in quality of life, with social and psychological data. Nonetheless, there are few studies on this subject and the impact on mood and sexuality.
The clinical and socio-demographic findings of the present study are in agreement with other studies conducted in Northeast Brazil and in the states of São Paulo and Rio de Janeiro.16 It is also noted that the frequency of patients with UI in the studied sample is similar to that observed by Barroso,17 with female predominance, low schooling, and symptoms beginning around the fourth and fifth decades of life.
Andrade et al.4 evaluated 118 patients with HTLV-1 and found a prevalence of 42.4%, lower than that observed in the present study, but with similar results: female predominance, basic education, and married women. The group with symptoms showed significantly lower scores in all domains of the SF-36 questionnaire.
In this study, the most affected domains were: incontinence impact, DLAS limitation, physical and social limitations, social relations, emotions, sleep and disposition, and measurements of severity. One of the hypotheses for these results is that patients with UI have lower self-esteem, interference in their sexual life, restrictions on social contact, domestic tasks, and work. The main complaint of these patients is their difficulty of leaving home, their need for constant trips to the bathroom, and their fear of not arriving there ``in time". The dependence on the bathroom becomes common for these patients who reported the constant need to find a bathroom as soon as they arrive at supermarkets, parties and friends' houses or even when they are doing some physical activity, interfering significantly in their daily life activities and leisure.18,19
In our study, 54.8% of the participants reported sexual relations bad or null, and no statistical difference was observed between the groups. Oliveira et al.20 evaluated 105 patients with a mean age of 48 ± 10.7 years. Overall, ED was observed in 55.2% and documented in all patients with HAM/TSP, in 79% of patients with oligosymptomatic myelopathy, and in 35.9% among asymptomatic HTLV-1-infected individuals.
The prevalence of UI in men in our study was 44.4%. The pathophysiology of ED in men is still unknown and UI appear as a determining factor for a negative impact on the quality of life in seropositive patients since the majority of this population refers to their sexual activity as bad or unfavorable. Furthermore, male patients with neurogenic bladder report ED and poor sexual activity.21 According to Tanus et al. the association of a higher HTLV-1 proviral load in men with ED lends support to the idea that ED is part of the autonomic syndrome related to viral infection and should be investigated for early identification of the syndrome.22
In women, the prevalence of UI in this study was 55.5% compared to a national prevalence of 26.2% found in another study.23 These patients reported psychological and emotional problems associated with UI such as shame, fear, nervousness, and depression. Women with incontinence reported receiving treatment for depression (5.3%), fear of losing urine during intercourse (4.2%), feel embarrassment and sadness due to UI (2.1%), are ashamed of herself in front of the husband when losing urine during intercourse (3.8%), while women with urge-incontinence reported being nervous and uncomfortable with UI (6.2%).
In this study, all participants with UI reported loss of urine during sexual intercourse, humidity present in the clothes, fluid intake control, unpleasant urine odor. These results corroborates the findings of Paranhos et al.24 pointing to fragility of incontinent women, mainly because UI occur in intimate moments associated with sexuality, promoting social, family and conjugal embarrassment. Thus, UI contributes to changes in quality of life and difficulties in relationships as a result of interrupted sexual intercourse.
The study carried out by Lopes and Higa23 with 164 women with UI shows that 40.9% of them reported UI interference in their sexual life. The restriction was caused by losing urine, feeling pain during intercourse, not feeling pleasure or desire to have intercourse, decrease or lack of sexual activity, need to interrupt sexual activity to urinate, and feel the urge to urinate during intercourse. These findings are also in line with the results of this study.
The discomfort during sexual intercourse and concern about losing urine in front of his partner was observed in the study by Pedrozo et al.25 The concern of these women to suffer some embarrassment with the partner became a barrier to their own sexuality, especially during intercourse. The fear of more suffering, caused by the possible loss of urine, generated a feeling of low self-esteem, as well as decreased libido.
With specific regards to the population of this study, it was possible to observe that what impacted most in sexuality was HAM/TSP, there being no statistical difference between the groups, and more than 50% of the sample considering their sexual life to be bad or null. Feelings of guilt, shame, anguish, fear and isolation and impotence behaviors related to disease progression, loss of autonomy and ability to work and leisure often can justify the lack of sexual interest, the negative perception of health, the depression frequency and possible impacts on the body image observed in this population.23
The small sample of patients evaluated is a limitation of this study, which was mainly due to the shame of patients to respond to a questionnaire about sexuality. The advantage was to address a topic that has been poorly studied and discussed during medical consultations, but significantly influences quality of life, marital relationships and mood states. We believe that some aspects regarding sexuality have not been sufficiently addressed in this quantitative study and a research using psychotherapeutic groups could deepen on such issues, as well as a comparison before and after this intervention. Another suggestion would be the implementation of a multiprofessional psychoeducational group to approach the theme during the medical visits.
ConclusionThe prevalence of UI was 58.06% in outpatient with HAM/TSP receiving care at a clinic in the city of São Paulo. The main impact of UI was on the perception of quality of life of these patients and on sexuality.
UI significantly impacts quality of life, especially in relation to activities of daily living, social life and emotional state. UI is associated with difficulty in sexual practice because of constraints caused by loss of urine and other possible discomforts during intercourse, lack of interest and sexual desire.
No statistical difference was observed regarding the frequency of anxiety, depression and perception of body image in participants with HTLV-1 with or without UI.
Conflicts of interestThe authors declare no conflicts of interest.