The serine-aspartate repeat proteins (Sdr) are members of a family of surface proteins and contribute to the pathogenicity of Staphylococcus aureus. Among 288 S. aureus isolates including 158 and 130 associated with skin and soft tissue infections and bloodstream infection, respectively; 275 (95.5%) were positive for at least one of three sdr genes tested. The positivity rates for sdrC, sdrD, and sdrE among S. aureus isolates were 87.8% (253/288), 63.9% (184/288), and 68.1% (196/288), respectively. 224 (77.8%) of 288 isolates were concomitantly positive for two or three sdr genes. There was an association between carriage of sdrE and methicillin-resistant S. aureus (MRSA) isolates, while the carriage rates of sdrC and sdrD in MRSA isolates were similar to those in methicillin-sensitive S. aureus (MSSA) isolates. The prevalence of co-existence of sdrC and sdrE among MRSA isolates was significantly higher than that among MSSA isolates (p<0.05). All ST1, ST5, ST7, and ST25 isolates were positive for sdrD. While all ST121 and ST398 isolates were negative for sdrD. All ST59 and ST88 isolates were positive for sdrE. All ST1 isolates were concomitantly positive for sdrC and sdrD. Concomitant carriage of sdrC, sdrD, and sdrE was found among all ST5, 75.0% (9/12) of ST1, 69.2% (9/13) of ST6, 78.6% (11/14) of ST25, and 90.9% (20/22) of ST88 isolates. sdrD was linked to CC5, CC7 and CC88 isolates, especially CC88 isolates. There was a strong association between the presence of sdrE and CC59, CC88, and CC5 isolates. A significant correlation between concomitant carriage of sdrC, sdrD, and sdrE and CC88 isolates was found. sdrC-positive, sdrD-positive and sdrE-negative gene profile was significantly associated with CC7 clone. There was an association between sdrC-positive, sdrD-negative, and sdrE-positive gene profile and CC59 isolates. A correlation between sdrC-positive, sdrD-negative, and sdrE-negative gene profile and CC121 clone was found. More CC59 isolates carried sdrC-negative, sdrD-negative, and sdrE-positive gene profile relative to other four CCs isolates. All ST1 and ST5, 95.2% (20/21) of ST188 and 95.2% (20/21) of ST630 isolates were positive for sdrC. Taken together, our investigation indicated that different S. aureus lineages were associated with specific patterns of carriage of sdr genes.
Staphylococcus aureus is a frequently encountered human pathogen which is the cause of a wide range of infectious diseases, such as skin and soft tissue infections (SSTIs), foreign-body infections, pneumonia, septic arthritis, osteomyelitis, sepsis, endocarditis, and bloodstream infection (BSI) in both hospital and community settings.1 The ability of S. aureus to successfully persist within the hosts is largely due to a battery of virulence factors which promote adhesion, acquisition of nutrients, and evasion of host immune responses.2,3 Many S. aureus isolates also produce one or more additional exoproteins including toxic shock syndrome toxin-1 (TSST-1), the staphylococcal enterotoxins (SEs), the exfoliative toxins (ETs), leukocidins, and so on.2–4 Most of the adhesins produced by S. aureus are cell wall-anchored proteins and are grouped into a single family which is named microbial surface components recognizing adhesive matrix molecules (MSCRAMM). MSCRAMM can bind extracellular matrix proteins such as fibronectin, fibrinogen, collagen, and elastin. The serine-aspartate repeat proteins (Sdr), encoded by the tandemly arrayed sdrC, sdrD, and sdrE genes located in the sdr locus, are members of the MSCRAMM family and members of a family of surface proteins with the presence of an R region containing various numbers of the Ser-Asp dipeptides encoded by the sdr genes.5 Sdr proteins are not closely related, with only 20 to 30% identical amino acid residues, indicating that different Sdr proteins have different roles in S. aureus pathogenicity.6 There are two, three, or five additional 110- to 113-residue sequences (B motifs) in Sdr proteins. B motifs are followed by segments composed of the SD repeats (R region) and tandemly repeated in SdrC, SdrE, and SdrD, respectively.5 The C-terminal end of the Sdr proteins is associated with anchoring the proteins to the bacterial cell wall.5 Josefsson et al. reported that at least two sdr genes were present in all tested S. aureus strains.5 The sdrC gene is always present in the sdr genes, while sdrD and sdrE are not.6,7 However, the correlation between the carriage of sdr genes and clonal lineage of S. aureus clinical isolates is unknown. The aim of the present study was to investigate the distribution of sdr genes among S. aureus isolates and the correlation between the carriage of sdr genes and clonal lineage of S. aureus isolates.
Materials and methodsCollection of S. aureus clinical isolatesA total of 288 non-duplicate S. aureus clinical isolates (single isolate per patient), including 158 associated with SSTIs and 130 associated with bloodstream infection (BSI), were collected for this investigation. The 130 S. aureus BSI isolates were identified in patients from four hospitals in eastern China, including the first Affiliated Hospital of Wenzhou Medical University from January 2004 to December 2010 (66 isolates), Lishui Center Hospital in 2010 (10 isolates), Taizhou Center Hospital in 2010 (7 isolates) and Shaoxing Municipal Second Hospital in 2010 (8 isolates) and Jiangxi Provincial Children Hospital in central China in 2010 (39 isolates). The 158 S. aureus isolates were identified in patients with SSTIs at the first Affiliated Hospital of Wenzhou Medical University from January 2012 to September 2013(128 isolates) and Jiangxi Provincial Children Hospital in 2010(30 isolates). Of 288 S. aureus isolates tested, 217 and 71 were isolated from adults and children, respectively. All isolates tested were identified as S. aureus using Gram stain, positive catalase and coagulase test results, and Vitek microbiology analyzer (bioMérieu, Marcy l’Etoile, France). All S. aureus isolates were tested at the clinical microbiology laboratory, Department of clinical laboratory, the first Affiliated Hospital of Wenzhou Medical University. The Ethics Committee of the first Affiliated Hospital of Wenzhou Medical University exempted this study from review because the present study focused on bacteria.
DNA extractionS. aureus isolates tested were cultured on blood agar overnight. Three to four bacterial colonies were suspended in 150μL sterile distilled water with 10μL lysostaphin (1mg/mL) (Sangon, China) and incubated at 37°C for 30min. DNA was extracted using the Genomic DNA Extraction kit in accordance with the manufacturer's instructions (Sangon, China). The extracted DNA was stored at −20°C and prepared for PCR amplification.
Detection of sdr genessdrC, sdrD, and sdrE were detected by PCR assays with primers and conditions previously described.8 PCR products were sequenced for the confirmation of sdrC, sdrD and sdrE. S. aureus isolates positive for sdrC, sdrD, and sdrE determined by PCR and DNA sequencing were used as control strain for every PCR assay for the detection of sdrC, sdrD, and sdrE.
Multilocus sequence typing (MLST)MLST typing of S. aureus isolates tested was determined using PCR amplification of internal fragments of the seven housekeeping genes of S. aureus as described previously, including carbamate kinase (arcC), shikimate dehydrogenase (aroE), glycerol kinase (glp), Guanylate kinase (gmk), phosphate acetyltransferase (pta), triosephosphate isomerase (tpi), and acetyl coenzyme A acetyltransferase (yqi).9 All PCR productions of seven housekeeping genes tested were sequenced. The DNA sequences were compared with the existing sequences available on the MLST website for S. aureus (http://saureus.mlst.net), and STs were determined according to the allelic profiles. Novel STs were deposited in the MLST database (http://saureus.mlst.net/). Clonal complexes were analyzed using eBURST v3 available on the MLST website for S. aureus (http://saureus.mlst.net).
Statistical analysisDifferences between groups were assessed by using the chi-square test.
Analyses were carried out with the statistical software SPSS 13.0. p-values <0.05 were considered a statistically significant.
Results and discussionPrevalence of sdr genes among S. aureus clinical isolatesSdrC promotes both bacterial adherence to surfaces and biofilm formation.10 The expression of SdrC and SdrD each contributed to the ability of S. aureus to adhere to human desquamated nasal epithelial cells, while the expression of SdrE did not promote adhesion.11 However, Peacock et al. found a strong correlation between S. aureus invasiveness and the presence of one of the allelic variants of the sdrE gene.7 Presence of sdrD gene in S. aureus isolates was significantly more prevalent in bone infections.12 Sitkiewicz et al. reported that SdrD played a role in the interactions between S. aureus and human immune system.13 In the present study, 275 (95.5%) of 288 S. aureus isolates were positive for at least one sdr genes tested. The positivity rates of sdrC, sdrD, and sdrE among S. aureus isolates were 87.8% (253/288), 63.9% (184/288), and 68.1% (196/288), respectively. The carriage of sdrC, sdrD, and sdrE among S. aureus isolates are shown in Table 2. Previous investigations showed that sdrC was present in all S. aureus isolates tested.6,7 However, 12.2% (35/288) of S. aureus isolates tested were negative for sdrC in the present study. The positivity rates of sdrD and sdrE in the present study were higher than in the previous study that showed positivity rates of sdrD and sdrE in S. aueus isolates of 48% and 56%, respectively.7 Out of 288 isolates, 134 (46.5%) were concomitantly positive for sdrC, sdrD and sdrE; 31.2% (90/288) were concomitantly positive for two of the three sdr genes tested. While 17.4% (51/288) of the isolates were only positive for one of the three sdr genes tested.
Prevalence of sdr genes among MRSA and MSSA isolatesIn the United States, MRSA isolates from patients with complicated SSSI were more likely than MSSA isolates to carry sdrC sdrD and sdrE genes.8 Carriage of sdrC, sdrD, and sdrE among S. aureus isolates causing SSTIs and BSI is shown in Table 1. There were no significant differences in frequencies of sdrC, sdrD, and sdrE between S. aureus isolates from SSTIs and BSI. Carriage of sdrC, sdrD, and sdrE among MRSA and MSSA isolates is shown in Table 2. In the present study, although the positivity rates of three sdr genes tested among MRSA isolates were higher than among MSSA isolates, the significant difference was only found in the prevalence of sdrE (p<0.05). Previous study found a strong association between the presence of the sdrD gene and MRSA isolates, while the prevalence of sdrE among MRSA and MSSA isolates was not different.6 Conversely, there was an association between carriage of sdrE and MRSA isolates, while the prevalence of sdrD in MRSA isolates was similar to that in MSSA isolates in the present study. A previous study also found that all MRSA isolates were positive for two or the three sdr genes.6 Our investigation showed that the prevalence of co-existence of sdrC and sdrE among MRSA isolates was significantly higher than among MSSA isolates (p<0.05). However, there was no significant difference between the concomitant carriage of sdrC, sdrD, and sdrE among MRSA and MSSA isolates (p<0.05). In 35.8% (39/109) of MRSA isolates and in 29.1% (52/179) of MSSA isolates there were concomitant positivity for two genes tested. Compared with MRSA isolates (11.0%, 11/109), more MSSA isolates (22.3%, 40/179) were only positive for one sdr locus. The sdrC-positive, sdrD-negative, and sdrE-negative gene profile was exclusively found among 29 MSSA isolates.6 In contrast, this gene profile was found both in MRSA and MSSA isolates in the present study. All gene profiles of sdr genes were found among MSSA isolates. However, sdrC-negative, sdrD-positive, and sdrE-negative gene profile was not found among MRSA isolates except one isolate.
Carriage of sdrC, sdrD, and sdrE among S. aureus isolates causing SSTIs and BSI.
| S. aureus SSTIs isolates (n=158) (%) | S. aureus BSI isolates (n=130) (%) | p-Values | |
|---|---|---|---|
| sdrC | 136 (86.1) | 117 (90.0) | >0.05 |
| sdrD | 101 (63.9) | 83 (63.8) | >0.05 |
| sdrE | 112 (70.9) | 84 (64.6) | >0.05 |
| sdrC+, sdrD+ and sdrE+ | 75 (47.4) | 59 (45.4) | >0.05 |
| sdrC+, sdrD+ and sdrE− | 17 (10.8) | 20 (15.4) | >0.05 |
| sdrC+, sdrD− and sdrE+ | 26 (16.5) | 21 (16.2) | >0.05 |
| sdrC−, sdrD+ and sdrE+ | 5 (3.2) | 1 (0.9%) | >0.05 |
| sdrC+, sdrD− and sdrE− | 18 (11.4) | 17 (13.1) | >0.05 |
| sdrC−, sdrD+ and sdrE− | 4 (2.5) | 3 (2.3) | >0.05 |
| sdrC−, sdrD− and sdrE+ | 6 (3.8) | 3 (2.3) | >0.05 |
Carriage of sdrC, sdrD, and sdrE among S. aureus, MRSA and MSSA isolates.
| S. aureus isolates (n=288) (%) | MRSA isolates (n=109) (%) | MSSA isolates (n=179) (%) | p-Values | |
|---|---|---|---|---|
| sdrC | 253 (87.8) | 101 (92.7) | 152 (84.9) | 0.063 |
| sdrD | 184 (63.9) | 70 (64.2) | 114 (63.7) | >0.05 |
| sdrE | 196 (68.1) | 85 (78.0) | 111 (62.0) | 0.013 |
| sdrC+, sdrD+ and sdrE+ | 134 (46.5) | 56 (51.4) | 78 (43.6) | 0.274 |
| sdrC+, sdrD+ and sdrE− | 37 (12.8) | 12 (11.0) | 25 (14.0) | >0.05 |
| sdrC+, sdrD− and sdrE+ | 47 (16.3) | 25 (22.9) | 22 (12.3) | 0.032 |
| sdrC−, sdrD+ and sdrE+ | 6 (2.1) | 1 (0.9) | 5 (2.8) | 0.4141 |
| sdrC+, sdrD− and sdrE− | 35 (12.2) | 8 (7.3) | 27 (15.1) | 0.063 |
| sdrC−, sdrD+ and sdrE− | 7 (2.4) | 1 (0.9) | 6 (3.4) | 0.086 |
| sdrC−, sdrD− and sdrE+ | 9 (3.1) | 3 (2.7) | 6 (1.7) | >0.05 |
+, positive; −, negative.
A total of 59 STs were identified among 288 S. aureus isolates tested. Five clonal complexes (CCs) accounting for more than 20 isolates, including CC5, CC7, CC59, CC88, and CC121 were identified by clustering analysis using eBURST v3 available on the MLST website for S. aureus (http://saureus.mlst.net). CC5, CC7, CC59, CC88, and CC121 accounted for 146, 34, 26, 23 and 27 S. aureus isolates, respectively. Among146 CC5 isolates 27 STs were identified, including ST188 (21 isolates), ST630 (21 isolates), ST25 (14 isolates), ST239 (13 isolates), ST6 (13 isolates), ST1 (11isolates), ST5 (11 isolates), and ST965 (9 isolates). Five STs including ST7, ST774, ST789, ST943, and ST 2833 were found among 34 CC7 isolates, among which ST7 was the predominant ST accounting for 30 isolates. Among 26 CC59 isolates, 23, 1, 1, and 1 belonged to ST59, ST749, ST2201, and ST2832, respectively. Only two STs, ST88 (22 isolates), and ST1219 (one isolate) were identified among CC88 isolates. A total of seven STs were found among 27 CC121 isolates, including ST121 (11 isolates), ST120 (10 isolates), ST946 (two isolates), ST2209 (one isolate), ST2210 (one isolate), ST2213 (one isolate), and ST2213 (one isolate). These data indicate that included S. aureus isolates exhibited considerable genetic heterogeneity.
The distribution of some virulence genes was correlated with the different MRSA lineages.14,15 All ST1 and ST5, 95.2% (20/21) of ST188 and 95.2% (20/21) of ST630 isolates were positive for sdrC. All ST1, ST5, ST7, and ST25 isolates were positive for sdrD. While all ST121 and ST398 isolates were negative for sdrD. All ST59 and ST88 isolates were positive for sdrE. All ST1 isolates were concomitantly positive for sdrC and sdrD. Concomitant carriage of sdrC, sdrD, and sdrE was found among all ST5, 75.0% (9/12) of ST1, 69.2% (9/13) of ST6, 78.6% (11/14) of ST25, and 90.9% (20/22) of ST88 isolates. However, five of seven ST39 isolates were negative for sdrC, sdrD, and sdrE.
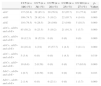
Carriage of sdrC, sdrD, and sdrE among five major CCs isolates is shown in Table 3. In addition to CC59 isolates with an sdrC prevalence of 76.9%, the prevalence of sdrC among CC5, CC7, CC88, and CC121 isolates were more than 85.0%, among which CC88 isolates had the highest prevalence of sdrC (95.7%). There were no differences in the positivity rates of sdrC among five major S. aureus clones (p=0.067). However, the positivity rates of sdrD among CC5, CC7, and CC88 isolates were high to 74.7%, 82.4%, and 95.7%, respectively, while the rates among CC59 and CC121 isolates were only 19.2% and 14.8%, indicating that sdrD was linked to CC5, CC7, and CC88 isolates, especially CC88 isolates. Compared with CC59 and CC88 isolates with an sdrE prevalence of 100% and CC5 isolates with an sdrE prevalence of 79.5%, the prevalence of sdrE among CC7 (26.5%) and CC121isolates (18.5%) were significantly lower (p<0.05). There was a strong association between presence of sdrE and CC59, CC88, and CC5 isolates. Surprisingly, 91.3% of CC88 isolates were concomitantly positive for sdrC, sdrD and sdrE, followed by CC5 isolates (58.2%), while concomitant carriage of the three sdr genes tested among CC7 (23.5%), CC59 (19.2%), and CC121 (3.7%) isolates was much lower, indicating a significant correlation between concomitant carriage of sdrC, sdrD, and sdrE and CC88 isolates. The prevalence of sdrC-positive, sdrD-positive, and sdrE-negative gene profile among CC7 isolates (52.9%) was higher than in other CCs isolates, especially CC59, CC88, and CC121 isolates where this gene profile was not found, indicating that such profile was significantly associated with the CC7 clone. sdrC-positive, sdrD-negative, and sdrE-positive gene profile was found in 57.7% of CC59 isolates, which was significantly higher than that in other CCs isolates (p<0.05). There was an association between sdrC-positive, sdrD-negative, and sdrE-positive gene profile with CC59 isolates. The positivity rates of sdrC-negative, sdrD-positive, sdrE-positive gene profile among five major clones were very low, and absent among CC7, CC59, and CC121 isolates. The prevalence of sdrC-positive, sdrD-negative, and sdrE-negative gene profile among CC121 isolates (67.3%) was much higher than in other CCs isolates (p<0.05), indicating a correlation between sdrC-positive, sdrD-negative, and sdrE-negative gene profile with CC121 clone. Sabat et al. reported that S. aureus isolates with sdrC-positive, sdrD-negative, and sdrE-negative gene profile belonged to ST1, ST12, ST25, ST30, ST34, ST39, ST47, and ST49.6 More CC59 isolates (23.1%) carried sdrC-negative, sdrD-negative, and sdrE-positive gene profile relative to other four CCs isolates.
Carriage of sdrC, sdrD and sdrE among five major CCs S. aureus isolates.
| CC5 (n=146) (%) | CC7 (n=34) (%) | CC59 (n=26) (%) | CC88 (n=23) (%) | CC121 (n=27) (%) | p-Values | |
|---|---|---|---|---|---|---|
| sdrC | 137 (93.8) | 29 (85.3) | 20 (76.9) | 22 (95.7) | 21 (77.8) | 0.067 |
| sdrD | 109 (74.7) | 28 (82.4) | 5 (19.2) | 22 (95.7) | 4 (14.8) | 0.000 |
| sdrE | 116 (79.5) | 9 (26.5) | 26 (100) | 23 (100) | 5 (18.5) | 0.000 |
| sdrC+, sdrD+ and sdrE+ | 85 (58.2) | 8 (23.5) | 5 (19.2) | 21 (91.3) | 1 (3.7) | 0.000 |
| sdrC+, sdrD+ and sdrE− | 18 (12.3) | 18 (52.9) | 0 (0) | 0 (0) | 0 (0) | 0.000 |
| sdrC+, sdrD− and sdrE+ | 24 (16.4) | 1 (2.9) | 15 (57.7) | 1 (4.3) | 3 (11.1) | 0.000 |
| sdrC−, sdrD+ and sdrE+ | 5 (3.4) | 0 (0) | 0 (0) | 1 (4.3) | 0 (0) | 0.519 |
| sdrC+, sdrD− and sdrE− | 10 (6.8) | 2 (0.59) | 0 (0) | 0 (0) | 17 (63.0) | 0.000 |
| SdrC−, sdrD+ and sdrE− | 1 (0.7) | 2 (0.59) | 0 (0) | 0 (0) | 0 (0) | 0.103 |
| SdrC−, sdrD− and sdrE+ | 2 (1.4) | 0 (0) | 6 (23.1) | 0 (0) | 1 (3.7) | 0.000 |
+, positive; −, negative.
S. aureus infections usually result from the combined action of a variety of virulence factors. However, the contribution of particular virulence factors to S. aureus infection is unclear. To further cast light on the role of sdr genes in S. aureus infections caused by different clones, a larger number of S. aureus clinical isolates with specific clones should be investigated.
In conclusion, our investigation indicated that different S. aureus lineages were associated with specific patterns of carriage of sdr genes.
Conflicts of interestThe authors declare no conflicts of interest.
This study was supported by grants from National Natural Science Fund of China (81271906H2002).