Rabies is a fatal disease resulting from rabies virus infection, causing severe neurological symptoms and ultimately death by destroying the nervous system. In general, a patient tends to see a neurologist or an infectious diseases physician, with very common and typical discipline-related signs and symptoms, such as hydrophobia, aerophobia, and mental disorders. However, we reported a rabies patient who was first admitted to see a thoracic surgeon with spontaneous pneumomediastinum.
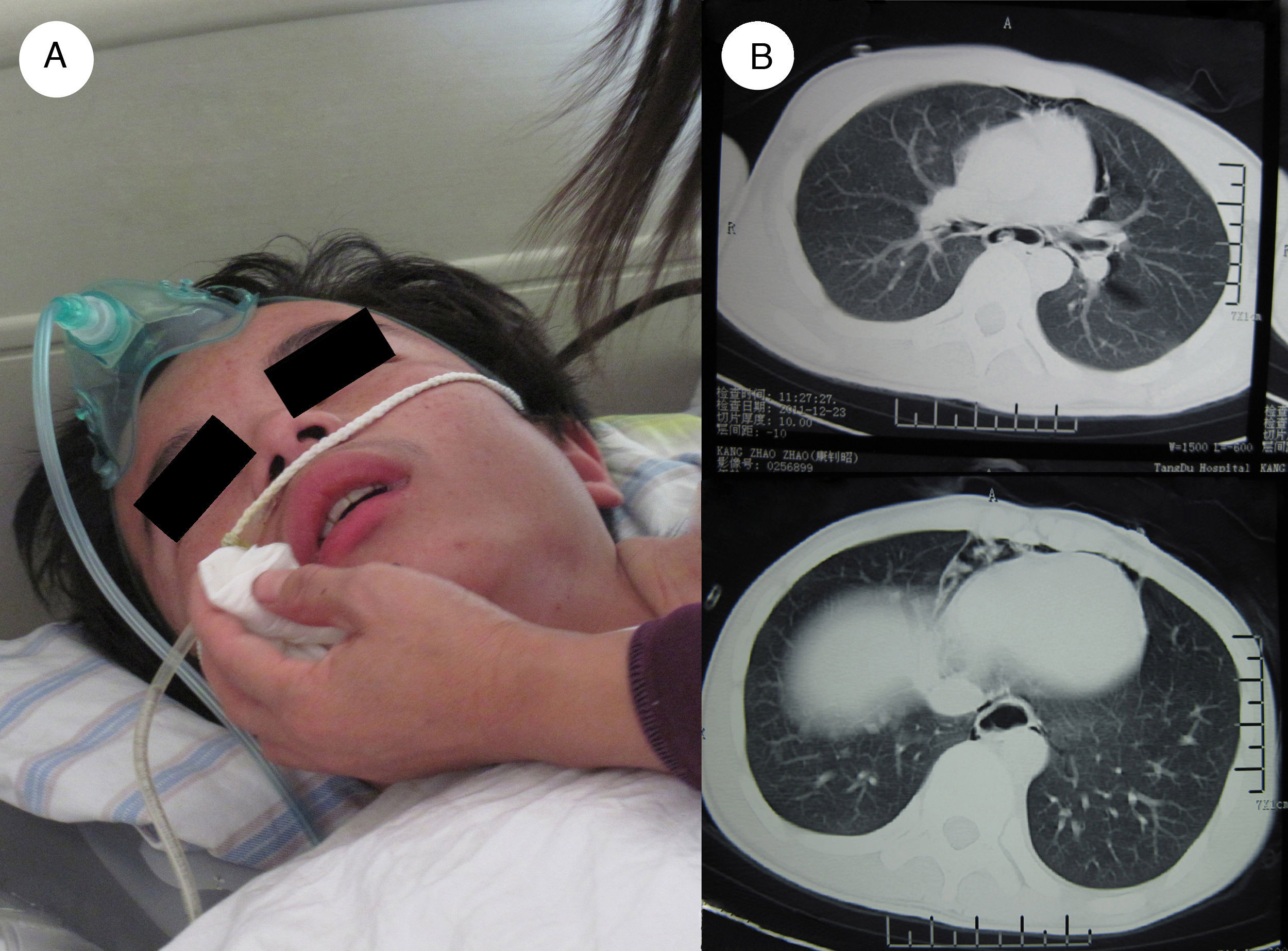
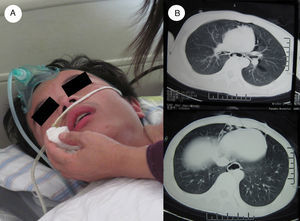
A 16-year-old patient was admitted to our hospital with an intermittent dysphasia, vomiting and high fever over 39°C for three days. The physical examinations found mild subcutaneous emphysema in the anterior and upper chest wall. An emergent chest computerized tomography (CT) scan showed a significant pneumomediastinum with a dilation of esophagus lumen. Spontaneous esophagus rupture was first considered, and oral diet was forbidden. Supportive care was provided at the same time. However, the following fibrobronschopy, gastroscopy as well as barium swallow showed no leakage of the airway and the esophagus. On the third day after admission, he was suddenly unconscious, with production of large quantity of saliva, complicated with a urinary incontinence and paralysis. However, about half an hour later, he regained the consciousness, but accompanied with an obvious facial muscle spasms and uncontrolled dysphoria. His mental status alternated between normal periods and confusion. The cardiogram monitor showed cardiac arrhythmia. The CT scan of the brain was unremarkable. He had a history of being bitten by a pet dog 10 years ago, but without a post-exposure prophylaxis. The paralytic rabies was considered then, and he was transferred to the department of infectious disease. Brain liquid examination was normal, and blood tests showed the AST of 257μ/L, CK of 7527μ/L, CK-MB of 124μ/L, LDH of 559μ/L. The rabies virus RNA from saliva was positive. Patient finally died from respiratory failure five days later. The autopsy of the brain found Negri bodies, which confirmed a diagnosis of paralytic rabies (Fig. 1).
Rabies is a viral disease with uncertain incubation period that causes acute encephalitis (inflammation of the brain) in warm-blooded animals. For a human, rabies is almost invariably fatal if post-exposure prophylaxis is not administered prior to the onset of severe symptoms. The rabies virus infects the central nervous system, ultimately causing disease in the brain and death. No successful treatment of rabies was reported until the one by Willoughby et al. in 2005.2 Patients were treated with ketamine, midazolam, ribavirin, and amantadine, induced coma without rabies vaccine at the same time. The treatment was known as Milwaukee Protocol. On the basis of clinical manifestations, rabies can be classified into 2 types: furious and paralytic rabies.1 The former is characterized by the well-known symptoms of hydrophobia, aerophobia, and hypersalivation. However the latter type is likely to be misdiagnosed because of its similarity to Guillian–Barré syndrome and neuropsychiatric illnesses. Sometimes an atypical clinical presentation or complications also contribute to a delay in diagnosis of this fatal disease.3 The standard for the diagnosis of rabies included the finding of Negri bodies, and positive staining by direct fluorescence assay (DFA) and RT-PCR in patient's brain.
Our patient had symptoms compatible with paralytic rabies 10 years after being bitten by dog. He had no aerophobia and hydrophobia, and presented with typical spontaneous pneumomediastinum initially, which prompted us to rule out the common etiologies of pneumomediastinum, such as spontaneous esophagus rupture or tracheal fistula. And the initial presentation with pneumomediastinum might still have resulted in delay in diagnosis of the fatal rabies.
The mechanism of spontaneous pneumomediastinum was unclear in rabies patients, but might be associated with an un-self-controlled, violent spasm of pharynx and the larynx observed during episodes of rabies, which resulted in acute and transit obstruction of airway and the esophagus lumen, causing alveolar or esophagus rupture under a transit higher pressure.3,4 That is why Boerhaave's syndrome sometimes occurred in rabies patient.5 In this patient the esophagus lumen was over-dilated with difficulty in swallowing, which also resulted from the abnormal and overexcited relax muscle movement.
To our knowledge, this is the third case reported with pneumomediastinum as the initial presentation of rabies in literatures published in English language.3,4 All the patients were finally confirmed as paralytic ones. For its rarity, the doctors should keep in mind that the pneumomediastinum is also an unusual complication of rabies, and which should be considered in case of pneumomediastinum, especially for those co-existed with signs of neurological symptoms. When the diagnosis of rabies is being considered, it would be helpful in diagnosing the treatment of the disease.
ConclusionThe pneumomediastinum is a rare and uncommon manifestation of paralytic rabies, which can present initially during the disease progression, resulting in delay of diagnosing rabies. And rabies should be considered in patients with pneumomediastinum.
Conflict of interestThe authors have no conflicts of interest to declare.