Empyema is a severe complication of different diseases and traumas. Management of this complication is difficult and should comprise general and local procedures. The general procedure is mainly based on administering wide-spectrum antibiotics. Local management depends on patient general condition, but in all cases the essential procedure is to insert a drain into the pleural cavity and to evacuate the pus. Sometimes pus is very thick and its evacuation and following re-expansion of the lung is rather impossible. In these patients surgical intervention is needed. The use of intrapleural enzymes to support the drainage was first described in 1949 by Tillett and Sherry using a mixture of streptokinase and streptococcal deoxyribonuclease. Nowadays, purified streptokinase has come into widespread use, but recent studies reported no streptokinase effect on pus viscosity. On the other side, deoxyribonuclease reduces pus viscosity and may be more useful in treatment. We report two cases of intrapleural administration of Pulmozyme (alfa dornase – deoxyribonuclease (HOFFMANN-LA ROCHE AG) in dosage 2×2.5mg with a significant improvement caused by changes in pus viscosity.
In this study we describe case reports of two patients with pleural empyema treated by intrapleural administration of deoxyribonuclease (DNase).
Patient no. 1A 33-year-old male was admitted to the Pneumonology Department because of chest pain on the right side, high temperature (±39°C) and weight loss of about 5kg which has been observed within 3 weeks. Clinical examination and chest X-ray revealed a pleural empyema. Laboratory examination of the peripheral blood was done. (There were 20.9K/μL leucocytes, 4.32K/μL erythrocytes, 12.4g/dL haemoglobin, 1.1μmol/L creatinine, 357.1mg/L CRP protein, thrombocytes 406K/μL, 4.6mmol/L kalium, LDH 694U/L, albumin 2.6g/dL, GOT/AspAT 43U/L, and GPT/ALAT 42U/L) The patient was treated with intravenous broad spectrum antibiotics: cefuroxim (Zinacef 3×750mg iv), amikacin (Biodacin 2×500mg iv), Metronidazol (3×500mg iv). At the beginning microbiological cultivation was negative. Later Staphylococcus aureus K (−) metycilin resistant was detected. According to the sensitivity Lincomycin 600mg iv every 8h was introduced. Zinacef and Biodacin were put aside.
Thoracentesis was performed but no fluid was obtained. The patient was relocated to the Thoracic Surgery Centre, where the chest tube was inserted into the pleural cavity. Drain was inserted into the pleural cavityin local analgesia (1% lignocain). Drain (size 36) was introduced in the posterior axillary line in the VIII intercostal space and was connected to the sucking system 20mmH2O. Ultrasonography of pleural cavity was done and loculated fluid was diagnosed. Second drain was introduced into the empyema cavity. Additionally the suppurative infiltration of the chest wall was confirmed. The incision of the chest wall was done and the second drainage (drain size 28) was introduced into the suppurative space of the chest wall. Drains were connected into the two different sucking systems. The position of both drains was controlled by X-ray. The effect of treatment was not satisfactory. During the first days only a small amount of pus from pleural cavity was removed because of high pus density. Within the first day the amount of pleural fluid was 300mL, within the second only 30mL, and on the third 20mL. In the subsequent two days Pulmozyme was administered directly into the pleural cavity through the drain. The total amount of Pulmozyme administered was 5mg. 2.5mg of dornase alfa and 50mL of normal saline were instilled into the pleural cavity daily for 2 consecutive days. The tube was clamped for 4h after instillation of this agent. During this period patient changed the position (lateral, supine, face down position). On the day 1 after Pulmozyme application 900mL of thin pus was drained; on the day 2, a further 300mL of drainage was collected with considerable improvement in the X-ray and the patient's clinical status. His appetite improved and temperature decreased. The chest drain was removed on day 10.
Patient No. 2A 21-year-old male was admitted with a 4 weeks history of fevers and rigours with breathlessness. The patient was treated in out-patient regime by antibiotics (erythromycin) without microbiological investigation or antibiotic sensitivity testing. Thoracentesis was performed with evacuation of 100mL of pus. The patient was relocated to the Thoracic Surgery Centre, where the chest tube was inserted into the pleural cavity. Drain was inserted into the pleural cavity in local analgesia (1% lignocain). Drain (size 32) was introduced in the posterior axillary line in the VIII intercostal space and was connected to the sucking system 20mmH2O. Control ultrasonography and X-ray of pleural cavity were performed. The patient was treated with intravenous broad spectrum antibiotics: cefuroxim (Zinacef 3×750mg iv) amikacin (Biodacin 2×500mg iv), Metronidazol (3×500mg iv). The Streptococcus pneumoniae was detected and examined as sensitive for applied antibiotics mentioned above.
Clinical examination and chest X-ray revealed a pleural empyema. Laboratory examination of the sample of the peripheral blood was done. (There were 16.7K/μL leucocytes, 4.2K/μL erythrocytes, 16.7g/dL haemoglobin, 254mg/L CRP protein, thrombocytes 412K/μL, bilirubin total 0.5mg/dL, kalium 4.1mmol/L, LDH 594U/L, albumin 2.9g/dL, GOT/AspAT 47U/L, and GPT/ALAT 45U/L.)
During the first days only a small amount of pus from pleural cavity was removed because of high pus density. On day 1 the amount of pleural fluid was 220mL, day 2 only 80mL, and day 3 – 40mL. In the subsequent two days Pulmozyme was administered directly into the pleural cavity through the drain. The total amount of the administered Pulmozyme was 5mg. 2.5mg of dornase alfa and 50mL of normal saline were instilled into the pleural cavity daily for 2 consecutive days. The tube was clamped for 4h after instillation of this agent. On first day after Pulmozyme application 700mL of thin pus was drained; on second day a further 400mL of drainage was obtained with considerable improvement in the X-ray and the patient's clinical status. His appetite improved and temperature decreased. The chest drain was removed on day 12.
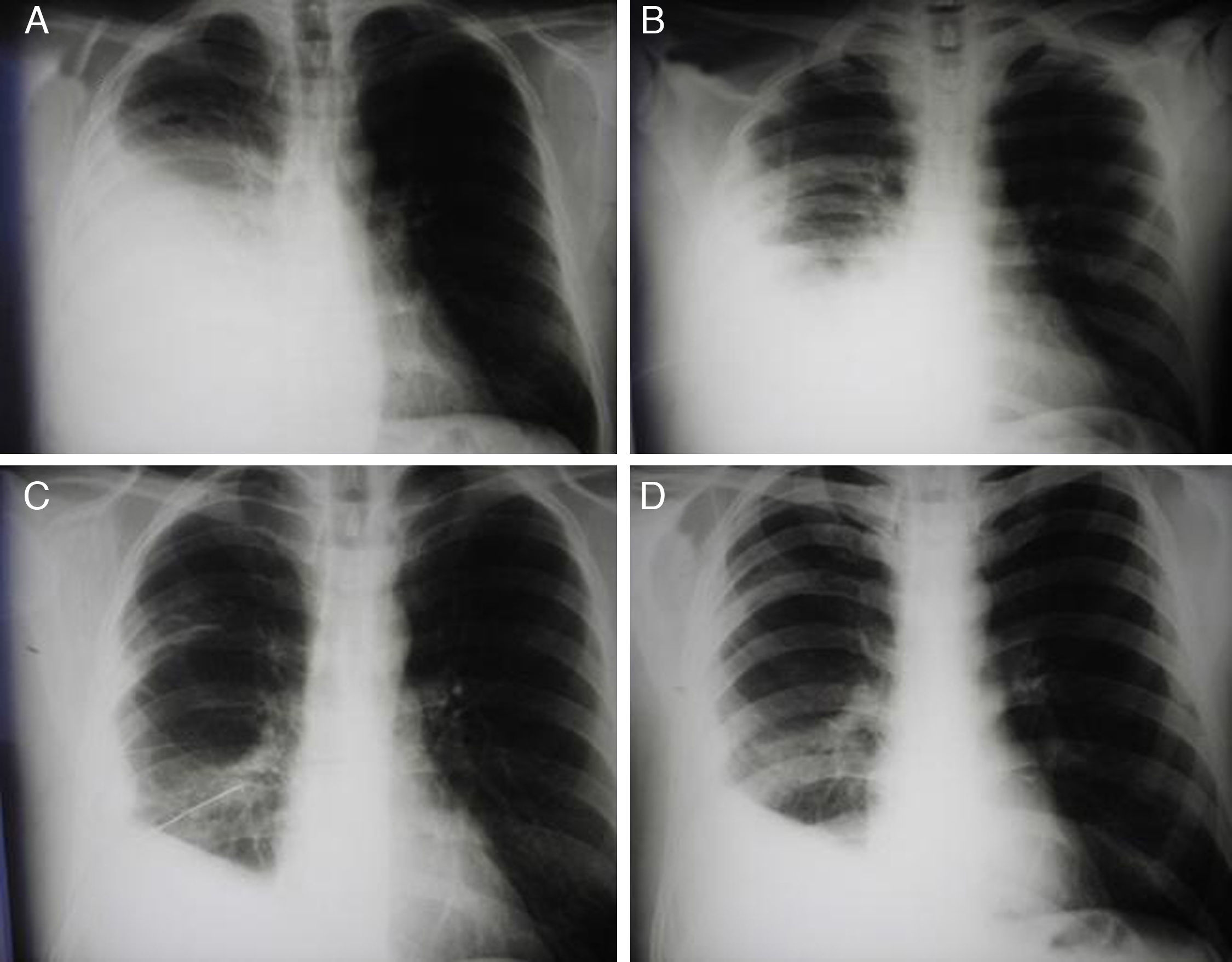
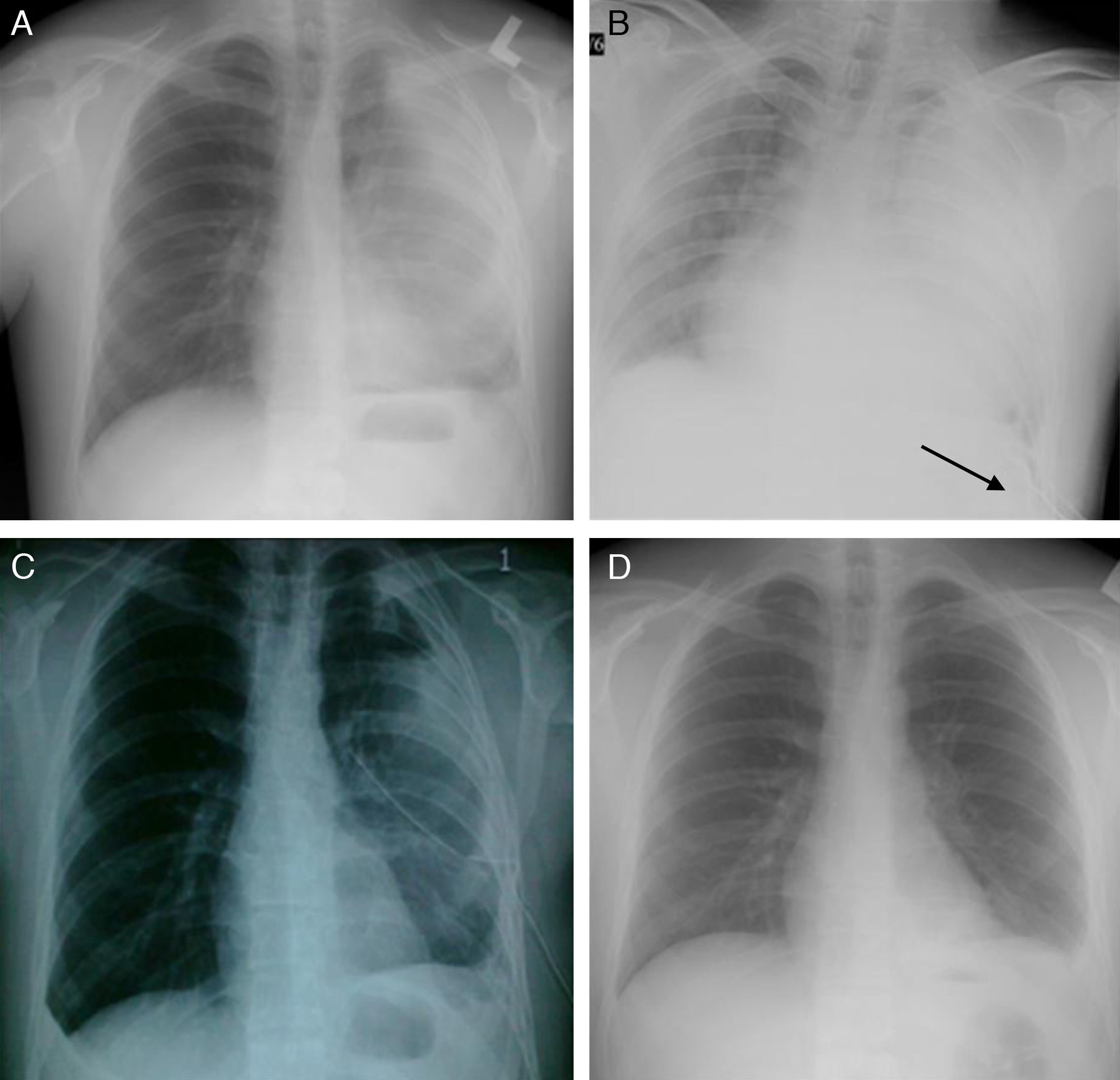
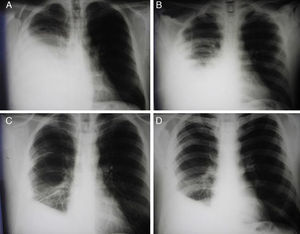
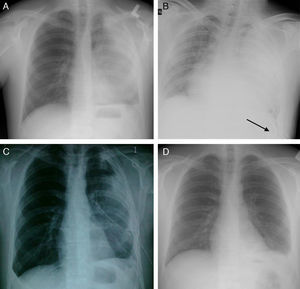
In both patients the first chest X-ray (Figs. 1A and 2A) was performed before treatment and the last one (Figs. 1D and 2D) after removing the drain. After release from the hospital the patient was controlled in the hospital outpatient clinic. The X-ray done after 1 month was better than the ones shown in Fig. 2.
To measure drainability a 2mL medical syringe fitted with 1.2×40 (18G×11/2″) needle was used.
Patient no. 1The measurement of viscosity before instillation of the dornase alfa was 56drops/min. After instillation of the first dornase alfa dose it was 210drops/min and after the second dose 225drops/min.
Patient no. 2The viscosity before instillation of dornase alfa was 10drops/min and after instillation of dornase alfa 86drops/min.
DiscussionSuccessful treatment of pleural empyema depends on adequate drainage of pleural cavity. There are other factors which prevent successful drainage by intercostals tube: chest tube size, loculation of the fluid and increasing viscosity, and adherence of the pus to the pleural surfaces, possibly preventing lung re-expansion by coating the visceral pleura. There are many studies which suggest to use intra-pleural fibrinolytic therapy especially streptokinase and urokinase in treatment of multiloculated pleural empyemas with good success rate. Some authors suggest that intrapleural instillation of fibrinolytic agents appears to be an effective and less invasive alternative to surgical treatment.3–6 The results of some control studies using purified streptokinase are divergent.7,8 Simpson et al. suggest that purified streptokinase was less effective than the older drug preparation which has contained a small proportion of streptococcal DNase.2,9
In the randomized, multicentre trial (MIST-1) the positive effect of streptokinase in pleural infections could not be substantiated.10
Although streptokinase lyses adhesions, it does not reduce pus viscosity.2 It is possible that combination of agents that reduce pus viscosity and break down loculations may be more effective in the infected pleural space drainage. Recently, an intrapleural DNase-administration could be used in combination with thrombolytic therapy to enhance pus drainage. In an animal model, the combination of recombinant tissue plasminogen activator (alteplase) and recombinant human deoxyribonnuclease (rhDNase) has been shown to be more effective in treating empyema than either agent used alone.11
Intrapleural use of a fibrinolytic agent (to disrupt adhesions) and DNase (to decrease pus viscosity) may promote efficient drainage of pus in empyema. This should be confirmed by the recently completed Multi-centre Intrapleural Sepsis Trial (MIST-2 To date, this is the largest, multi-centre, randomized, controlled trial, in which patients were randomized in a 1:1 fashion into 4 treatment arms. The four treatment groups included: (1) fibrinolytics plus DNase; (2) fibrinolytics alone; (3) DNase alone; and (4) saline.
Combination of intrapleural tPA/DNase was significantly superior to the other combinations in improving pleural fluid drainage. DNase or tPA alone are ineffective. The proportion of patients dying or requiring surgery for their infection was higher in the DNase and saline group.
Pulmozyme is a recombinant DNAse that digests DNA in the mucous secretions in lungs. Alteplase and Reteplase are the second generation recombinant tPAs. Pulmozyme cleaves extracellular DNA in mucus of cystic fibrosis patients, reducing the adhesiveness and viscoelasticity of the mucus.
Human recombinant DNase seems to be extremely safe and effective when it is administered by nebulization in the treatment of cystic fibrosis.1 Similarly, treating empyema by DNase could be promising for patients in future.
ConclusionPulmozyme may be used in some patients with pleural empyema with good results.
Conflict of interestAll authors declare no conflict of interest.
Supported by the Research project P 27/2012 awarded by Charles University in Prague, 3rd Faculty of Medicine, Prague, Czech Republic.