The 10-valent pneumococcal conjugate vaccine (PCV10) has been included in Bulgarian Childhood Immunization Program since 2010. This study aimed to assess serotype distribution and antimicrobial resistance of 198 invasive and non-invasive Streptococcus pneumoniae strains that had been isolated in Bulgaria during 2011–2016 from patients with invasive (IPD) and non-invasive (NIPD) pneumococcal diseases. The most common invasive serotypes were 3 (10.1%), 19F (4.0%), and 7F (3.0%). A significant decrease in the proportion of invasive vaccine types (VTs) from 64.2% to 35.2% was found in comparison with pre-vaccine era. The most common serotypes among middle ear fluids were 3, 19A and 19F (5.6% each), and VTs fell down from 66.4% to 40.0% in post-PCV10 period. Among respiratory isolates, the most prevalent serotypes were some emergent serotypes such as 15A/B/C (5.0%), 19A, and 6C (4.0% each). VTs decreased significantly (16.3%) among vaccinated children compared to unvaccinated children and adults (44.0%). Two non-VTs (19A and 6C) have increased significantly more (p<0.05) in vaccinated children than in unvaccinated patients. The rates of antibiotic nonsusceptible S. pneumoniae in Bulgaria remained high in post-PCV10 era. Among all source of isolates, antimicrobial nonsusceptibility rates were: oral penicillin – 46.5%, trimethoprim-sulfamethoxazole – 45.4%, erythromycin – 43.9%, tetracycline – 37.4%, and multidrug-resistance (MDR) was 44%. The most common MDR serotypes were 19F, 19A, 6A/C, 15A/B/C and 23A. Our results proved that PCV10 vaccination substantially reduced VTs pneumococcal IPD and NIPD. There has been a shift in the distribution of S. pneumoniae serotypes mostly in vaccinated children but also in the whole population and strong serotype-specific antibiotic resistance was observed after vaccine implementation. Therefore, it is important to continue monitoring serotype changes and pneumococcal resistance among all patient ages in addition to aid in determining the long-term effectiveness of PCV10 interventions.
Despite the development of antipneumococcal vaccines Streptococcus pneumoniae is still an important cause of severe invasive pneumococcal diseases (IPD) worldwide. Pneumococcus is also a global cause of less serious but more frequent respiratory tract infections, such as otitis media, sinusitis, and non-bacteremic pneumonia.1 The prevention of pneumococcal disease is hampered by antigenic diversity of the pneumococcal capsule, a major virulence factor of this species and a target of all current commercially available vaccines.2 There are at least 95 capsule types (serotypes) that differ by invasiveness, disease severity, antibiotic resistance profiles, and case fatality ratio.2 Since the currently available vaccines provide protection only against a limited number of serotypes their distribution and characteristics warrant careful continuous monitoring.
The first, heptavalent pneumococcal conjugate vaccine (PCV7), targeting seven serotypes of S. pneumoniae (serotypes 4, 6B, 9V, 14, 18C, 19F, 23F) has been available for infant vaccination programs in the United States since the 2000s, subsequently in European and other countries.2 Following the introduction of PCV7 vaccination there has been a reduction of IPD caused by serotypes included in the vaccine among the adult population (indirect or herd effects) which has been attributed to a reduction of nasopharyngeal colonization in vaccinated children.3 Furthermore, as serotypes included in the PCV7 were those which expressed the highest rates of antibiotic resistance, PCV7 vaccination had a concomitant decreasing effect on the incidence of IPD and other non-invasive pneumococcal diseases (NIPD) caused by antibiotic-resistant S. pneumoniae.4 However, after the introduction of PCV7 the incidence of pneumococcal diseases caused by non-PCV7 serotypes such as 1, 3, 6A, 6C, 7F, and 19A increased in countries with routine vaccination.5 Vaccine serotypes (VTs) have nearly disappeared and have been largely replaced by non-vaccine serotypes (NVTs).6 PCV7 programs have not been affected because the increases in incidence of NVTs infections are small compared with the decreases in incidence of IPD caused by VTs.5
Since 2010, two broad spectrum PCVs, the 10-valent (PCV10) and 13-valent (PCV13) are available and both vaccines proved to be more effective than PCV7.7 The 10-valent pneumococcal nontypeable Haemophilus influenzae protein D conjugate vaccine (PHiD-CV or PCV10) contains the PCV7 serotypes, as well as serotypes 1, 5, and 7F. As has been shown, PCV10 has greatly reduced VTs IPD and provides indirect protective effects via reduced VTs carriage.8–11 Additionally, the PHiD-CV vaccine has showed significant protection against NTHi otitis media.12
In April 2010, the Bulgarian Immunization Program introduced PCV10 as a first PCV for universal childhood vaccination of all infants in a three-dose schedule at 2, 3, and 4 months of age with a booster at 12 months (3+1 schedule). PCV10 vaccination of targeted age-groups is very high (>90%) according to the national epidemiological data (National Center of Health Information). Prior to PCV10 implementation, PCV7 had not been used in our country despite being available in the market since 2008.
The main goal of this study was to provide an inventory of S. pneumoniae strains which were responsible for invasive and non-invasive infections in children and adults in the era of PCV10 vaccination. The objectives were to determine whether the use of PCV10 caused a shift in the pnemococcal serotype distribution and serotype relationship to antibiotic-resistance patterns in order to evaluate the impact of the vaccine in our country where mass vaccination of infants has been implemented.
Material and methodsPatients and specimen collectionThis post-PCV10 surveillance study was conducted in a total of 198 non-duplicated S. pneumoniae strains collected between May 2011 and May 2016 at several clinical microbiological laboratories throughout Bulgaria. The study has been initiated one year after PCV10 introduction into our routine vaccination schedule. Our Department of Medical Microbiology received these isolates from three laboratories located in Sofia and another three hospital laboratories located elsewhere in the country (Medical Universities of Plovdiv, Pleven, and Varna) on a voluntary basis. Clinical and demographic data (date of birth or age, date of admission in hospital, diagnosis) were collected by review of the medical charts or from the data recorded on the request of cultures to laboratories. The pneumococcal strains were isolated from invasive and non-invasive specimens of patients at different ages. The collection did not represent all sequential strains which had been isolated in collaborating laboratories, but there were no selection criteria for sending the strains.
Among this collection, 71 were invasive strains isolated from cerebrospinal fluid (n=38), blood (n=24), and pleural fluid (n=9). A case of IPD was defined as the recovery of an isolate of S. pneumoniae from a normally sterile site.
The second pneumococcal collection included 127 respiratory isolates cultured from samples of patients diagnosed with NIPD. The non-invasive isolates were obtained from nasopharynx of children (n=69), middle ear fluid (MEF) (n=45), from conjunctiva (n=8), and sputum of adults (n=5). NIPD was defined as S. pneumoniae strains causing infection detected in ear, eye, tracheal aspirate specimens or nasopharynx, and in which no invasive (sterile sites) isolates were collected from the same patient. From children diagnosed with acute otitis media (AOM), one middle ear fluid sample or one nasopharyngeal sample per child was collected. The AOM episodes were confirmed by an otorrinolaryngologist or pediatrician. We categorized AOM episodes as severe, complicated AOM (n=45) which either required tympanocentesis or presented with spontaneous otorrhea, and in such cases MEF sample was taken. Additionally, 45 AOM episodes diagnosed in children without perforation were also included, in which nasopharyngeal samples were taken through the nose, because tympanocentesis was not done.
PCV status was determined on the base of patients’ age at the date when the pneumococcal strain was isolated. Each patient was categorized according to his/her immunization status at pneumococcal disease presentation as either “unvaccinated”, if they had not received PCV10 vaccination according to age, or “PCV10 vaccinated”. All children born in April 1st, 2010 or thereafter were eligible for vaccination regardless whether they had received the vaccine or not, as coverage rate of PCV10 was high among age-eligible children (>90%). We defined them as a group of vaccinated children who had received ≥3 doses of PCV10. Another group of older children and adults not eligible for PCV10 vaccination (those born before April, 2010) from the data recorded on the request of cultures to laboratories was defined as an unvaccinated population. We compared serotype distribution rates for both groups of patients (vaccinated children and unvaccinated children and adults).
All pneumococcal strains were confirmed with both methods – optochin susceptibility test and bile solubility.
SerotypingSerogrouping of S. pneumoniae was performed using the latex agglutination method (Pneumotest-Latex kit, Statens Serum Institute-SSI, Copenhagen, Denmark). The isolates that reacted negatively were non-typeable. Serotyping was performed with the capsular Neufeld Quellung method using some common factor antisera provided by the SSI. For more accurate serotyping, serogroup 6 isolates were subjected to PCR serotyping. Primers wciP584gS and wciP, designed by Jin et al.13 were used for detection of serotype 6A (149bp). S. pneumoniae 6A strains were further subjected to PCR targeting wciNβ to identify 6C (359bp) with primers wciNbS1 and wciBbA2, published by Park et al.14 The serotype 6B isolates were tested by PCR with primers wciP584aS and wciP,13 which amplify a part of wciP gene (155bp product). The PCV10 coverage was estimated by calculating the percentage of isolates that expressed the serotypes included in the vaccine and the coverage rate did not included cross-reactive NVTs.
Antimicrobial susceptibility testingThe antibiotic susceptibilities (minimal inhibitory concentrations – MICs) were determined by the broth microdilution method on Microtiter plates (HPB-Haemophilus/Streptococcus pneumoniae, Sensititre, Trek Diagnostic Systems Ltd., UK). The plate was inoculated with cation-adjusted Mueller-Hinton broth and 5% lysed horse blood. Final bacterial density was 5×105CFU/mL and the plates were incubated at 35°C for 20–24h in 5% CO2. Antibiotic susceptibilities were defined according to the breakpoints of the European Committee on Antimicrobial Susceptibility Testing (EUCAST). Pneumococcal isolates were classified as penicillin-nonsusceptible (benzylpenicillin MIC≥0.1μg/mL) and ampicillin/ceftriaxone/cefuroxime, iv – nonsusceptible (MIC≥1.0μg/mL) according to EUCAST breakpoints.15S. pneumoniae ATCC 49619 was used as the control strain for the susceptibility test. Multidrug resistance (MDR) was defined as nonsusceptibility to three or more antimicrobial agents.
Detection of macrolide resistance determinantsThe macrolide resistant genes ermB and mefA/E were amplified by PCR methods for all erythromycin-resistant isolates.16 The PCR products of the mef genes were digested with BamHI to distinguish the mefA and mefE gene subclasses.17
Statistical analysisThe rates of serotype distribution among vaccinated and unvaccinated patients were compared using Fisher's exact test (http://www.socscistatistics.com/tests/fisher/Default2.aspx). Differences in proportions of PCV10 vaccine types from pre- and post-vaccine era were compared using Chi-squared test (χ2). A p value <0.05 was considered statistically significant.
ResultsDemographic and clinical data of patientsWe analyzed 198 invasive and non-invasive S. pneumoniae isolates recovered from specimens of children and adults with invasive and respiratory tract infections. Among them 141 isolates (71.2%) were obtained from children aged between 1 month to 14 years, the remaining 57 strains (28.8%) were recovered from adult patients. Out of the 141 children, 98 had received PCV10 vaccination (age-based vaccine status), comprising 49.5% out of all patients with IPD and NIPD analyzed here (Table 1). Meningitis (n=38) was the most common manifestation of the IPD cases (n=71), bacteraemic pneumonia and bacteraemia without focus accounted for 25 and 8 cases, respectively. The non-invasive pneumococcal strains (n=127) were isolated mostly from children diagnosed with AOM (n=90), patients with pneumonia (n=16), respiratory tract infection (n=13), or eye infection (n=8).
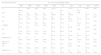
Serotype/serogroup distribution of 198 invasive and non-invasive S. pneumoniae isolates according to source of strain isolation and vaccine status.
| Serotype/serogroup(s) | Total No. (%) of particular serotype | % of serotype by source | % of serotype by vaccine status | ||||
|---|---|---|---|---|---|---|---|
| Invasive | Middle ear fluid | Respiratory | Vaccinated children | Non-vaccinated patients | p-Value | ||
| 3 | 37 (18.7) | 10.1 | 5.6 | 3.0 | 13.3 | 24.0 | 0.068 |
| 19F | 26 (13.1) | 4.0 | 5.6 | 3.5 | 11.2 | 15.0 | 0.529 |
| 19A | 23 (11.6) | 2.0 | 5.6 | 4.0 | 18.4 | 5.0 | 0.004 |
| 6A | 12 (6.1) | 2.0 | 1.0 | 3.0 | 6.1 | 6.0 | 1.0 |
| 15A/B/Cc | 11 (5.6) | 0.5 | 0.0 | 5.0 | 8.2 | 3.0 | 0.132 |
| 6C | 9 (4.5) | 0.0 | 0.5 | 4.0 | 9.2 | 0.0 | 0.001 |
| 7F | 8 (4.0) | 3.0 | 0.0 | 1.0 | 2.0 | 6.0 | 0.279 |
| 23A | 7 (3.5) | 0.5 | 0.0 | 3.0 | 6.1 | 1.0 | 0.064 |
| 11 | 7 (3.5) | 1.5 | 0.0 | 2.0 | 3.1 | 4.0 | 1.0 |
| 9V | 6 (3.0) | 1.5 | 1.5 | 0.0 | 0.0 | 6.0 | 0.029 |
| 24/31/40a | 5 (2.5) | 2.5 | 0.0 | 0.0 | 1.0 | 4.0 | 0.369 |
| 29,34,35,42,47a | 5 (2.5) | 0.5 | 0.0 | 2.0 | 3.1 | 2.0 | 0.681 |
| 14 | 5 (2.5) | 1.5 | 1.0 | 0.0 | 1.0 | 4.0 | 0.369 |
| 18C | 5 (2.5) | 1.0 | 0.5 | 1.0 | 0.0 | 5.0 | 0.059 |
| 23F | 4 (2.0) | 1.0 | 0.0 | 1.0 | 1.0 | 3.0 | 0.621 |
| 6B | 4 (2.0) | 0.0 | 0.5 | 1.5 | 1.0 | 3.0 | 0.621 |
| 9N/Ld | 4 (2.0) | 0.5 | 0.0 | 1.5 | 4.1 | 0.0 | 0.058 |
| NTb | 4 (2.0) | 0.0 | 0.0 | 2.0 | 3.1 | 1.0 | 0.366 |
| 13,28a | 3 (1.5) | 0.5 | 0.0 | 1.0 | 1.0 | 2.0 | 1.0 |
| 18A/B | 3 (1.5) | 0.5 | 0.5 | 0.5 | 2.0 | 1.0 | 0.619 |
| 22 | 3 (1.5) | 0.5 | 0.5 | 0.5 | 2.0 | 1.0 | 0.619 |
| 8 | 2 (1.0) | 1.0 | 0.0 | 0.0 | 0.0 | 2.0 | 0.498 |
| 4 | 1 (0.5) | 0.0 | 0.0 | 0.5 | 0.0 | 1.0 | 1.0 |
| 1 | 1 (0.5) | 0.5 | 0.0 | 0.0 | 0.0 | 1.0 | 1.0 |
| 25,38,43–46,48a | 1 (0.5) | 0.5 | 0.0 | 0.0 | 0.0 | 1.0 | 1.0 |
| 16/36/37a | 1 (0.5) | 0.0 | 0.0 | 0.5 | 1.0 | 0.0 | 0.495 |
| 21/39a | 1 (0.5) | 0.0 | 0.0 | 0.5 | 1.0 | 0.0 | 0.495 |
| Total No. (% of vaccinated children) | 198 (49.5) | 71 (8.4) | 45 (64.4) | 82 (76.8) | 98 (100.0) | 100 (0.0) | – |
| % of PCV10 vaccine types | 30.3 | 35.2 | 40.0 | 20.7 | 16.3 | 44.0 | – |
Bold values: Significant differences (p-value<0.05).
Serotype distribution of both invasive and non-invasive isolates according to source of the strain isolation and vaccine status is given in Table 1. Among the total 198 isolates at least 26 different serotypes/serogroups and four nontypeable (NT) S. pneumoniae strains (2%) were identified. Overall, the most common serotypes were 3 (18.7%), 19F (13.1%), 19A (11.6%), 6A (6.1%), 15A/B/C (5.6%), and 6C (4.5%). All of these serotypes, except type 19F, are non-vaccine serotypes. In the whole isolate collection, the theoretical serotype coverage of PCV10, not including cross-reactive non-vaccine serotypes was 30.3% (n=60).
Depending of source of pneumococcal isolates, the most common serotypes among invasive cases were 3 (10.1%), 19F (4.0%), and 7F (3.0%), and PCV10 vaccine coverage rate was 35.2% for patients with IPD. Out of the 71 invasive isolates, only six were obtained from vaccinated children (8.4%). Among them (vaccine-eligible children), five were NVTs pneumococci and one was vaccine serotype 7F. Among isolates from MEF, the most common serotypes were 3, 19A, and 19F (5.6% each), and PCV10 serotypes accounted for 40.0% of the MEF isolates obtained from children with severe AOM. In the remaining non-invasive isolates from respiratory tract, the most prevalent serotypes were 15A/B/C (5.0%), 19A, and 6C (4.0% each), and the coverage rate of PCV10 was 20.7% for respiratory strains. The proportions of vaccinated children among 127 non-invasive S. pneumoniae isolates were higher (64.4% in MEF specimens, and 76.8% in respiratory isolates) than the proportion of vaccinated population with invasive strains (8.4%). This is because non-invasive isolates were received more often from patients with AOM who were mostly children up to six years of age. In contrast, patients with IPD were mostly adults who were unvaccinated.
Serotypes distribution in the whole studied population was also analyzed according to vaccine status. In isolates obtained from vaccinated children (n=98), the most prevalent serotypes were 19A (18.4%), 3 (13.3%), 19F (11.2%), 6C (9.2%), 15A/B/C (8.2%), 6A, and 23A (6.1% each). Once again, all of these serotypes (except serotype 19F) are NVTs. In this group of vaccinated children, 16.3% of the serotypes were VTs (n=16). Among pneumococci obtained from unvaccinated patients with IPD and NIPD (n=100) the most prevalent serotypes were 3 (24.0%), 19F (15.0%), 6A, 7F, and 9V (6.0% each), and 19A (5.0%). In this group of unvaccinated patients, PCV10 serotypes were 44.0%. In order to determine if there were significant differences in serotype distribution among vaccinated and unvaccinated patients, we used Fisher's exact test for each serotype/serogroup. The proportions of some NVTs (19A, 15A/B/C, 6C, 23A) were higher in vaccinated children than in unvaccinated patients. Conversely, some VTs isolates (19F, 7F, 9V, 14, 18C, 23F, 6B) were more often found in the unvaccinated patients than in the vaccinated ones. Despite these proportional differences, only two NVTs (19A and 6C) showed significantly higher rates in vaccinated children, and the vaccine type 9V was found only in unvaccinated patients (p<0.05).
Antimicrobial nonsusceptibility and association with serotypeAntibiotic nonsusceptibility and serotype-specific resistance of all pneumococcal isolates to most important antimicrobial agents was analyzed in Table 2. On the basis of the EUCAST MIC breakpoints for susceptibility testing, a total of 92 isolates (46.5%) were nonsusceptible to benzylpenicillin (resistant and intermediately resistant to penicillin S. pneumoniae; MIC>0.06μg/mL). In the total of isolates nonsusceptibility rates to ceftriaxone, erythromycin, tetracycline, and trimethoprim-sulfamethoxazole were 19.7%, 43.9%, 37.4%, and 45.4%, respectively. None of the S. pneumoniae isolates was resistant to vancomycin. All of the isolates were susceptible to levofloxacin, with the exception of two strains (1.0%) which were intermediately resistant. Eighty-seven (44%) of the isolates were multidrug-resistant. In general, when the proportions of antibiotic nonsusceptibility depending on the site of isolation were compared we found that resistance rates were higher in non-invasive isolates (MEF and respiratory) than in invasive strains. Non-susceptibility to benzylpenicillin was 29.6%, 68.9%, and 48.8% in invasive, MEF, and respiratory isolates, respectively. For erythromycin, non-susceptibility rates were 26.8%, 55.6%, and 52.4% among invasive, MEF, and respiratory isolates, respectively.
Antimicrobial non-susceptibility among 198 invasive and non-invasive S. pneumoniae isolates of different serotypes.
| Serotype/serogroup(s) | No. (%) of nonsusceptible isolates | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PEN | AMP | CXM | CRO | ERY | CLI | TET | CHL | SXT | LEVO | |
| 3 | 4 (10.8) | 0 (0) | 0 (0) | 0 (0) | 3 (8.1) | 3 (8.1) | 3 (8.1) | 3 (8.1) | 0 (0) | 0 (0) |
| 19F | 25 (96.2) | 24 (92.3) | 21 (80.8) | 14 (53.8) | 26 (100.0) | 25 (96.2) | 26 (100.0) | 0 (0) | 24 (92.3) | 1 (3.8) |
| 19A | 19 (82.6) | 18 (78.3) | 18 (78.3) | 16 (69.6) | 16 (69.6) | 15 (65.2) | 15 (65.2) | 3 (13.0) | 18 (78.3) | 0 (0) |
| 6A | 5 (41.7) | 1 (8.3) | 1 (8.3) | 1 (8.3) | 7 (58.3) | 2 (16.7) | 1 (8.3) | 5 (41.7) | 7 (58.3) | 0 (0) |
| 15A/B/C | 6 (54.5) | 1 (9.1) | 0 (0) | 0 (0) | 5 (45.4) | 3 (27.3) | 5 (45.4) | 0 (0) | 5 (45.4) | 0 (0) |
| 6C | 7 (77.8) | 1 (11.1) | 1 (11.1) | 1 (11.1) | 6 (66.7) | 6 (66.7) | 7 (77.8) | 0 (0) | 2 (22.2) | 0 (0) |
| 23A | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 6 (85.7) | 6 (85.7) | 3 (42.9) | 4 (57.1) | 6 (85.7) | 0 (0) |
| Other PCV10 | 18 (52.9) | 12 (35.3) | 9 (26.5) | 6 (17.6) | 11 (32.3) | 8 (23.5) | 9 (26.5) | 6 (17.6) | 18 (52.9) | 1 (2.9) |
| Other Non-PCV10 | 5 (14.3) | 1 (2.9) | 0 (0) | 0 (0) | 4 (11.4) | 3 (8.6) | 5 (14.3) | 0 (0) | 7 (20.0) | 0 (0) |
| NT | 3 (75.0) | 2 (50.0) | 1 (25.0) | 1 (25.0) | 3 (75.0) | 1 (25.0) | 0 (0) | 0 (0) | 3 (75.0) | 0 (0) |
| Total No. (%) | 92 (46.5) | 60 (30.3) | 51 (25.8) | 39 (19.7) | 87 (43.9) | 72 (36.4) | 74 (37.4) | 21 (10.6) | 90 (45.4) | 2 (1.0) |
PEN, benzylpenicillin; AMP, ampicillin; CXM, cefuroxime iv; CRO, ceftriaxone; ERY, erythromycin; CLI, clindamycin; TET, tetracycline; CHL, chloramphenicol; SXT, trimethoprim-sulfamethoxazole; LEV, levofloxacin; NT, nontypable isolates.
The following non-susceptible MIC (μg/mL) breakpoints were used: benzylpenicillin≥0.12; ampicillin/ceftriaxone/cefuroxime iv≥1.0μg/mL according to the EUCAST.15
The most frequently found serotypes in benzylpenicillin non-susceptible pneumococci were 19F (96.2%) and 19A (82.6%), followed by 6C (77.8%), and 15A (54.5%). Serotypes 19F and 19A showed the highest resistance rates to penicillin, cefuroxime and ceftriaxone. The predominant serotypes among erythromycin-resistant S. pneumoniae (ERSP) were 19F (100%), 23A (85.7%), 19A (69.6%), 6C (66.7%), and 6A (58.3%). The distribution of macrolide resistance determinants among 87 ERSP isolates showed that 72 isolates (82.8%) carried erm(B) gene, including 31 strains (35.6%) with the presence of both erm(B) and mef(E) genes, and 15 strains (17.2%) carried the mef(E) gene solely. The dual resistance mechanism erm(B)+mef(E) was found in serotypes 19F (n=17), 19A (n=13), and 23F (n=1).
DiscussionThe implementation of the pneumococcal conjugate vaccines in the last decade has resulted in significant changes in the pneumococcal serotypes circulating all over the world.10,18–21 We aimed to evaluate whether the implementation of PCV10 as a routine, first pneumococcal vaccine in Bulgaria had resulted in similar changes in the serotypes causing IPD and NIPD diseases in our area. During the first five years after the PCV10 implementation, a change in the relative rates of the most common serotypes was observed, due to a reduction of PCV10 VTs and a concurrent increase in NVTs. In other words, serotype prevalence in Bulgaria has undergone a significant shift since routine vaccination with PCV10 commenced. In the present study we found a decrease in the incidence of VTs of 30.3% among all (invasive and non-invasive) isolates detected from both vaccinated and unvaccinated children and adults with IPD and NIPD diseases. However, as expected we observed that use of PCV10 in Bulgaria has led to serotype replacement not only in vaccinated children, but also in the whole population (indirect effect), a result that is in line with findings in other countries.2,6 The reduction in VTs was consistent with findings from other post-PCV surveillance studies and reflects the effectiveness of pneumococcal immunization.8,18,22
Compared to our previous study23 for IPD isolates in the pre-vaccine era (2006–2010), a significant decrease in the proportion of PCV10 VTs from 64.2% to 35.2% (p=0.0002) was found in the present study. Additionally, a significant reduction of VTs among MEF isolates from 66.4% to 40.0% (p=0.002) was detected, when we compared results in the current study with the pre-vaccine era24 for the same kind of specimen. We concluded that PCV10 was highly successful in reducing IPD and NIPD caused by VTs in our country. Increasing experience with PCV10 has shown effectiveness against IPD in children in Finland,8 Brazil,9 Netherlands,10 and Canada.11 Additionally, a reduction in incidence of both AOM presentations and pneumonia has been observed in Iceland after introduction of PHiD-CV10 to their national schedule.25 Some significant associations were also found between serotype distribution of the isolates and vaccine status of the patients. As expected, throughout the study period, a significant decrease of VTs (p<0.01) was found among vaccine-eligible children (16.3%) than in older children and adults (44.0%) ineligible for vaccination (indirect effect). Our findings suggest that after introduction of PCV10 into our Childhood Immunization Program the majority of the circulating pneumococci among vaccine-eligible children were NVTs.
Our results demonstrated that in the total pneumococcal collection studied here a change in serotype prevalence was observed during the first 5-year period following the introduction of PCV10. Overall, serotype 3 appeared as the most common serotype among all patients, showing the real magnitude of this serotype in our geographical area at present time. However, in the analysis of serotype changes, except for a shift toward NVTs, we observed differences in the temporal serotype prevalence depending of source of isolates. In fact, we found that VTs were almost eliminated from IPD in those vaccinated children aged <5 years, providing clear evidence of a strong vaccine effect for this group as has been documented in other countries.9,11,26 PCV10 was highly effective in preventing vaccine-serotype IPD. Serotypes 3 and 19F appeared as the most common serotypes in invasive and MEF isolates. Serotype 3 (NVT) is not included in PCV10, because no efficacy was demonstrated for that serotype with an 11-valent prototype vaccine.12 Vaccine serotype 19F was the most common type in the pre-vaccine era23,24 among invasive (15.8%; 2006–2010) and MEF (20.3%) isolates in our country despite having proportionally fallen down to 4.0% and 5.6%, respectively, in the present study. Our data suggest low but persistent circulation of this MDR 19F serotype in all age groups during the first five years. In time, the impact of PCV10 on the pneumococcal reservoir will become more evident, and will likely lead to a decline in serotype 19F, which was still prominent in our study among both invasive and non-invasive isolates. Despite the introduction of PCV10, serotype 19A continued to be among the most common serotypes causing mainly NIPD but was found also in IPD cases. In the current study serotype 19A was one of the most prominent MDR serotype in both MEF and respiratory specimens, despite having proportionally fallen down in comparison with its rate for 19A otitis media in the pre-vaccine era.24 Moreover, we observed a significantly increased proportion of serotype 19A among vaccine-eligible children (p=0.004) than in the group of unvaccinated children and adults. On one hand, PCV10 provides a high level of protection against IPD caused by 19A as has been shown in two epidemiologic studies from Brazil and Quebec, Canada.9,11 However, Best et al.,27 reported that serotype 19A is the commonest serotype causing IPD in New Zealand and their study does not support PHiD-CV10 preventing carriage of non-vaccine serotype 19A on AOM microbiology. Croucher et al.,28 have suggested that some pneumococcal MDR genotypes with the serotypes 19F and 19A belonging to PMEN14 clone have “soft” selective sweeps by PCVs, which might be the explanation for continuing circulation of both MDR serotypes in our post-vaccine period. In the future this serotype should be carefully monitored in the country. Another interesting result five years following the implementation of PCV10 was the most common prevalence in respiratory isolates and among the group of vaccinated children of some emerging NVTs as serotypes 15A/B/C, 6C and 23A. Most of these new emergent serotypes were MDR. Similar results have been reported from other studies in the post-PCV vaccination era.20,21 In future, serogroups 15 and 6 and serotype 23A should be followed up carefully as they were the most prominent NVTs associated with antibiotic resistance in our study. There were a few limitations to address in our study. First, the number of S. pneumoniae isolates was relatively small. Despite this, our cohort could still reflect the predominance of non-vaccine serotypes in the post-PCV10 era. Second, we categorized our patients as vaccinated or not vaccinated on the basis of patients’ age but we did not check the vaccine card of each patient. However, PCV10 uptake is known to be around 90% nationally, and this should not alter the overall conclusions drawn.
In Bulgaria, the rates of antibiotic nonsusceptible S. pneumoniae remained high in post-PCV10 vaccine era. The highest nonsusceptibility observed was to oral penicillin (47%), followed by trimethoprim-sulfamethoxazole (45%), macrolides (44%), and tetracycline (37%). With the exception of serotype 3, the most prevailing serotypes in our pneumococcal collection analyzed here were also the most common MDR serotypes. We concluded that the rates of antibiotic nonsusceptibility were still high in post-vaccine era, because of the wide prevalence of some MDR serotypes as 19F, 19A, 6C, 15A, 6A, and 23A. All of them, except serotype 19F, are NVTs. PCV10 reduced the resistant VTs pneumococci, while the proportion of those with reduced susceptibility due to wide distribution of some resistant NVTs is high. On the other hand an additional reason for wide prevalence of MDR isolates might be high antibiotic usage in Bulgaria. Although, PCV10 is extremely effective in reducing pneumococcal infections due to both resistant and susceptible VTs strains, resistant NVTs continue to emerge and expand in post-vaccine period. It is generally difficult to compare antimicrobial resistance data before PCV10 implementation that were found in our previous studies for invasive23 and MEF isolates24 because the guidelines for interpretation of antibiotic susceptibility in Bulgaria have changed from CLSI to EUCAST breakpoints since 2014.
In conclusion, this study reports the temporal changes in IPD and NIPD serotypes and antimicrobial nonsusceptibility of S. pneumoniae isolates among all patient ages during the first 5-year period following the introduction of PCV10 as routine vaccine in the Bulgarian immunization program. PHiD-CV vaccination substantially reduced vaccine-serotype pneumococcal IPD and NIPD diseases. However, a shift in the distribution of S. pneumoniae serotypes mostly in vaccinated children but also in the whole population and strong serotype-specific resistance to antibiotics was observed after vaccine implementation in our country. Therefore, it is important to continue monitoring serotype changes and pneumococcal resistance among all patients in addition to aid in determining the long-term effectiveness of PCV10 interventions.
Conflicts of interestThe authors declare no conflicts of interest.
This study was supported by Medical University of Sofia – Grant No. D21/2015. We thank all participating microbiological laboratories for their cooperation and for providing the isolates.