Chronic hepatitis B is a major cause of cirrhosis, and the natural history of the disease has several clinical stages that should be thoroughly understood for the implementation of proper treatment. Nonetheless, curing the disease with antiviral treatment remains a challenge.
AimsTo describe the clinical course, response to treatment, and poor prognostic factors in 247 hepatitis B virus chronic infection patients treated in a tertiary hospital in Brazil.
MethodsThis was a retrospective and observational study, by analyzing the medical records of HBV infected patients between January 2000 and January 2015.
ResultsMost patients were male (67.2%) and 74.1% were HBeAg negative. Approximately 41% had cirrhosis and 8.5% were hepatitis C virus coinfected. The viral load was negative after two years on lamivudine, entecavir and tenofovir in 86%, 90.6%, and 92.9% of the patients, respectively. The five-year resistance rates for lamivudine, adefovir, entecavir, and tenofovir were 57.5%, 51.8%, 1.9%, and 0%, respectively. The overall seroconversion rates were 31.2% for HBeAg and 9.4% for HBsAg. Hepatocellular carcinoma was diagnosed in 9.7% of patients, liver transplantation was performed in 9.7%, and overall mortality was 10.5%. Elevations of serum alanine aminotransferase (p=0.0059) and viral load (p<0.0001) were associated with progression to liver cirrhosis. High viral load was associated with progression to hepatocellular carcinoma (p<0.0001). Significant risk factors associated with death were elevated alanine aminotransferase (p=0.0039), liver cirrhosis (p<0.0001), high viral load (p=0.007), and hepatocellular carcinoma (p=0.0008). HBeAg positive status was not associated with worse outcomes, and treatment may have been largely responsible.
ConclusionsElevations of viral load and serum alanine aminotransferase may select patients with worse prognosis, especially progression to cirrhosis and hepatocellular carcinoma, which were strongly association with death.
Hepatitis B virus (HBV) affects over 240 million people worldwide, with 780,000 deaths each year from complications of the disease.1 In Brazil, 7.4% of the population have been exposed to the virus and about 0.37% have chronic disease.2
The stages of the disease must be understood to define the need for treatment. The natural prognosis of the infection depends on several aspects, such as geographic location, age at primary infection, viral genotype, host immune system, association with alcoholism, steatosis, and coinfections such as hepatitis C, hepatitis D and HIV.3,4
The first stage of the infection is the immunotolerant phase, in which individuals are positive for HBeAg, the antigen associated with viral replication, and there is absence of hepatocellular aggression. Subsequently, the patient experiences a reactive phase, during which inflammation is present and liver enzymes are elevated in attempt to eliminate the HBe antigen. Anti-HBe antibody appears and the patient enters the dormant stage of the disease, when viral replication is minimal or absent. At this point, HBsAg can be negative and anti-HBs positive, the patient can progress to healing; or the virus may become active again, even in the absence of HBeAg, setting the stage of HBeAg negative chronic hepatitis B (CHB).3,5
The disease is slowly progressive. The virus binds to hepatocyte DNA, causing inflammation and fibrosis, which may progress to liver cirrhosis (LC) and its complications, especially hepatocellular carcinoma (HCC), a major cause of death in this group of patients.6 Treatment slows the progression of the disease, decreasing morbidity and mortality. However, despite advances in antiviral therapy, a cure for hepatitis B remains challenging, since the drugs can eliminate the virus from the blood, but not from the hepatocytes.7,8
Few publications have detailed all factors associated with the disease in a population. The objectives of this study were to describe (1) the clinical and laboratory features of chronic hepatitis B virus infection in patients seen in a tertiary hospital, (2) the response to treatment and development of virological resistance, and (3) to analyze the factors that influence progression to LC, HCC, and death.
MethodsThis was an observational and retrospective study conducted by reviewing the medical records of patients treated at the Liver Unit of the Hospital de Clínicas-UNICAMP between January 2000 and January 2015. This study was approved by the local ethics committee (21589513.7.0000.5404).
Inclusion criteria: HBsAg positive patients aged between 16 and 81 years, who were followed at the clinic for more than six months. Exclusion criteria: patients with incomplete data related to the studied variables and HIV coinfected patients, as they are not treated in our center.
Clinical and laboratory classificationThe parameters analyzed were gender, hepatitis B virus serology, liver histology, alanine aminotransferase (ALT), hepatitis B viral load (VL), presence of nephropathy, and coinfection with hepatitis C virus (HCV). Poor prognosis factors were progression to LC, HCC, and death.
Patients were classified into two main groups: HBeAg positive (HBeAg+) and negative (HBeAg−), according to the initial HBeAg status.
In addition, patients were classified according to the developmental stages of hepatitis B virus chronic infection. HBeAg+ patients with repeatedly normal liver enzymes were classified as immunotolerant. HBeAg+ patients with abnormal liver enzymes and/or evidence of significant histological changes were classified as having HBeAg+ CHB. HBeAg− patients with VL less than 2000IU/mL or without evidence of significant histological changes were classified as inactive carriers. HBeAg− patients with VL greater than 2000IU/mL or with evidence of significant histological changes were classified as having HBeAg− CHB. Histological changes were considered significant in patients who had inflammatory activity ≥2 and/or fibrosis ≥2 in the METAVIR classification.9
Liver biopsy was performed when necessary for a definitive diagnosis or to assess indications for treatment. All biopsies were performed with a Tru-Cut 14G needle guided by ultrasound. The material was fixed in 10% formaldehyde and analyzed by an experienced pathologist using the METAVIR classification.9
The laboratory kits of serology, ALT dosage, and VL varied during the study period. The limits of detection and normal values were established according to the kit used by our laboratory.
LC was diagnosed according to the following criteria: liver histology showing grade 4 fibrosis, according to the METAVIR classification,9 or liver ultrasonography suggestive of cirrhosis, as well as evidence of portal hypertension on endoscopy or Doppler. Abdominal ultrasound examinations were performed with a Powervision 6000 SSA-370A C8612580 series (Toshiba) apparatus, using a 5MHz linear convex transducer. HCC diagnosis was established by biopsy or through three-phase imaging examination, with increased uptake by affected tissue in the arterial phase and rapid contrast wash-out in the portal and equilibrium phases. Patients were diagnosed with renal disease when they had an estimated creatinine clearance of <60mL/min or if they had undergone a kidney transplantation.
Treatment responseResponse to oral antivirals was defined as a negative VL after one and two years of treatment. Time to resistance was defined as the time between the start of medication and a VL increase of at least 1log.4 Response to treatment with conventional or pegylated interferon was considered satisfactory if there was drop in VL to less than 500IU/mL or negative HBeAg.
Statistical analysisChi-square test and Fisher's exact test were used to compare categorical clinical variables between groups. The Mann–Whitney test was employed to compare numeric clinical variables. Cox regression analysis was used to evaluate the relationship between risk factors and outcomes (LC, HCC and death). The significance level for this study was 5%. Statistical analysis was performed using the SAS System for Windows 2015.
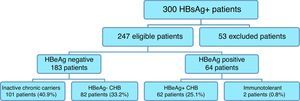
ResultsPopulation characteristicsBetween January 2000 and January 2015, 300 HBsAg positive patients who had been followed for more than six months were identified. However, 53 did not have complete information for the studied variables and were therefore excluded (Fig. 1). Thus, 247 patients were eligible and 166 were male (67.2%). The initial HBeAg was negative in 183 patients (74.1%) and positive in 64 (25.9%). The average age of patients at the inclusion was higher in the HBeAg− group: 42.5±12.7 years vs. 35.5±11.8 years (p=0.0478). The mean follow-up of patients was 8.9 years, ranging from 1 to 15 years.
Regarding the progressive phases, 101 (40.9%) were inactive chronic carriers, 82 (33.2%) were HBeAg− CHB, 62 (25.1%) had HBeAg+ CHB, and two (0.8%) were immunotolerant (Fig. 1).
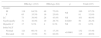
Initial normal ALT values were found in 66.1% of HBeAg− and 17.2% of HBeAg+ patients (p<0.0001). The initial VL was measured in 225 patients and was ≥100,000IU/ml in 28.6% of HBeAg− and in 96.9% of HBeAg+ patients (p<0.0001) (Table 1).
Clinical and laboratory characteristics of the study population.
| HBeAg− (183) | HBeAg+ (64) | p | Total (247) | ||||
|---|---|---|---|---|---|---|---|
| Gender | |||||||
| M | 118 | 64.5% | 48 | 75.0% | NS | 166 | 67.2% |
| F | 65 | 35.5% | 16 | 25.0% | 81 | 32.8% | |
| LC | 73 | 38.9% | 28 | 43.8% | NS | 101 | 40.9% |
| Nephropathy | 31 | 16.9% | 19 | 29.7% | 0.0289 | 50 | 20.2% |
| Hepatitis C | 17 | 9.3% | 4 | 6.3% | NS | 21 | 8.5% |
| Initial ALT | |||||||
| Normal | 121 | 66.1% | 11 | 17.2% | <0.0001 | 132 | 53.4% |
| Elevated | 62 | 33.9% | 53 | 82.8% | 115 | 46.6% | |
| HBeAg− (161) | HBeAg+ (64) | p | Total (225) | ||||
|---|---|---|---|---|---|---|---|
| Initial VL | |||||||
| <100,000IU/mL | 115 | 71.4% | 2 | 3.1% | <0.0001 | 117 | 52.0% |
| ≥100,000IU/mL | 46 | 28.6% | 62 | 96.9% | 108 | 48.0% | |
| HBeAg− (63) | HBeAg+ (23) | p | Total (86) | ||||
|---|---|---|---|---|---|---|---|
| Initial fibrosis | |||||||
| F0 and F1 | 38 | 60.3% | 9 | 39.1% | NS | 47 | 54.7% |
| F2, F3 and F4 | 25 | 39.7% | 14 | 60.9% | 39 | 45.3% | |
LC, liver cirrhosis; ALT, alanine aminotransferase; ULN, upper limit of normal; VL, viral load; F0 to F4, degrees of liver fibrosis by METAVIR classification; NS, not significant.
Liver biopsy was required to complete the evaluation in 86 (34.8%) patients. Fibrosis was ≥2 in 25/63 (39.7%) HBeAg− patients and in 14/23 (60.9%) HBeAg+ patients (Table 1).
A total of 101 (40.9%) patients had LC, 50 (20.2%) had chronic renal failure or transplanted kidney, and 21 (8.5%) were coinfected with HCV, with positive VL (Table 1).
Antiviral treatmentA total of 128 (51.8%) underwent treatment, but only 113 were using any medication at the end of the analysis. Entecavir was the most used drug in both HBeAg− and HBeAg+ groups: about 36% used this medication alone (Table 2). The negative VL rate at one year on lamivudine, entecavir, and tenofovir was 56%, 75%, and 75%, respectively. After two years, these rates were 86%, 90.6%, and 92.9%, respectively.
Treatment of chronic hepatitis B in the study population at the end of analysis.
| Drug | HBeAg− (68/183) | HBeAg+ (45/64) | Total (113/247) | |||
|---|---|---|---|---|---|---|
| Entecavir | 31 | 45.6% | 10 | 22.2% | 41 | 36.3% |
| Lamivudine | 17 | 25.0% | 7 | 15.6% | 24 | 21.2% |
| Lamivudine+tenofovir | 5 | 7.3% | 9 | 20.0% | 14 | 12.4% |
| Tenofovir | 7 | 10.3% | 5 | 11.1% | 12 | 10.6% |
| Lamivudine+adefovir | 5 | 7.3% | 6 | 13.3% | 11 | 9.7% |
| Tenofovir+entecavir | 2 | 3.0% | 7 | 15.6% | 9 | 8.0% |
| Adefovir | 1 | 1.5% | 1 | 2.2% | 2 | 1.8% |
Treatment with conventional or pegylated interferon was administered to 24 patients (9.7%) for 24 or 48 weeks, with a satisfactory response in 10 (41.7%), although only one patient lost HBsAg and there was no positive anti-HBs after interferon use until the end of the study.
Virological resistance to lamivudine in five years was detected in 57.5% and to adefovir in 51.8%. The average time for development of resistance to lamivudine and adefovir was 2.97 and 2.34 years, respectively. Resistance to entecavir was detected in one patient (1.9%) in whom resistance mutations L180/181M and rtM204V were observed. There was no resistance to tenofovir.
HBeAg and HBsAg seroconversionLoss of HBeAg occurred in 26/64 (40.6%) patients and 20 (31.2%) became anti-HBe positive. In this group, 10 patients had seroconversion with lamivudine, five with interferon, and other treatments in the remaining subjects.
To describe HBsAg seroconversion, 24 patients who underwent liver transplantation (LT) and used immunoglobulin were excluded. Therefore, in the remaining 223 patients, loss of HBsAg occurred in 29 (13%), and 21 (9.4%) were positive for anti-HBs. This antibody appeared spontaneously in 17 patients (6.9% of the whole population). Lamivudine was responsible for HBsAg seroconversion in three patients and lamivudine plus tenofovir in one; in other words, only 4/128 (3.1%) patients had positive anti-HBs with antiviral treatment. The presence of cirrhosis influenced loss or seroconversion of HBsAg. Cirrhotic patients most commonly lost HBsAg and the rate of non-cirrhotic patients positive for anti-HBs was higher (p=0.0322).
Liver cirrhosis, HCC, and deathInitial increases in ALT and VL were independent risk factors for progression to LC (Table 3). Twenty-four patients developed HCC (9.7%); all of them had cirrhosis, 20 (83.3%) were male, and 20 (83.3%) were HBeAg−. Patients with high VL (≥100,000IU/mL) had more than 7-fold greater risk of developing HCC (Table 3), as was the case in 19 of 24 patients with HCC.
Hazard ratios for LC, HCC and death (Cox Regression).
| Variable | Category | p-value | Hazard ratio | 95% CI |
|---|---|---|---|---|
| Risk for LC | ||||
| ALT | Increased vs. normal | 0.0059 | 1.75 | 1.175–2.608 |
| HBeAg | Positive vs. negative | NS | – | – |
| VL | < vs. ≥100,000IU/mL | <0.0001 | 2.740 | 1.858–4.069 |
| Risk for HCC | ||||
| ALT | Increased vs. normal | NS | – | – |
| HBeAg | Positive vs. negative | NS | – | – |
| VL | < vs. ≥100,000IU/mL | <0.0001 | 7.45 | 2.287–24.270 |
| Risk for death | ||||
| ALT | Increased vs. normal | 0.0039 | 3.826 | 1.537–9.527 |
| HBeAg | Positive vs. negative | NS | – | – |
| VL | < vs. ≥100,000IU/mL | 0.007 | 3.193 | 1.201–8.487 |
| LC | Yes vs. no | <0.0001 | 11.083 | 3.328–39.910 |
| HCC | Yes vs. no | 0.0008 | 4.131 | 1.796–9.499 |
ALT, alanine aminotransferase; ULN, upper limit of normal; VL, viral load; LC, liver cirrhosis; HCC, hepatocellular carcinoma; NS, not significant.
Coinfection with HCV had no significant influence on the occurrence of LC, HCC, or death (p=1.0, p=0.5, and p=0.22, respectively). Of the 21 coinfected patients, eight had LC, two had HCC, and three died. As shown in Table 3, initially elevated ALT, VL, LC, and HCC were independent risk factors for death, which occurred in 26/247 (10.5%) patients. Death was related to the disease in 22/26 (84.6%) patients, and 8/26 (30.8%) had HCC.
Liver transplantationTwenty-four patients underwent LT (9.7%), with a 76.2% survival rate in the first year and 71.4% in the second. Entecavir was used in 89% of transplanted patients. The indication of LT was HCC in 12 patients (50%) and impaired liver function in other 12 (50%).
Table 4 summarizes the clinical and serological outcomes in the study population during the 15-year study period.
DiscussionThis analysis described the course of hepatitis B virus chronic infection in a population over a period of 15 years. The majority of patients with hepatitis B were HBeAg−. In Brazil, it has been reported that nearly 50% of HBsAg positive patients have inactive disease and less than 2% are in the immunotolerant phase. Of patients with active disease, most have chronic HBeAg− hepatitis,10 as verified in our study. In China, where the virus has a high prevalence, a study with 8439 patients showed that 19% were HBeAg+ and 81% HBeAg−, of whom 35% were inactive carriers.11
Coinfection with HCV was found in 8.5% of patients in our analysis. Worldwide, these numbers range from 3 to 18%.12,13 Although coinfected patients are often described as having a more aggressive disease, with higher progression to LC and HCC,14 we did not find this association in our analysis. This could have been due to the growing effort to cure HCV, slowing the progression of liver disease. Half of these patients had negative HCV VL at the end of the study.
Antiviral treatment, resistance and seroconversionThe majority of our patients used entecavir. Our center is a reference for liver transplantation in the region, and therefore provides care for many cirrhotic patients (about 41%), which likely influenced the choice of this drug. Moreover, many of our patients have kidney disease, for which entecavir is more used.4,5
A total of 75% of our patients on entecavir or tenofovir had a negative VL at one year. Rates of 76–95% with tenofovir15 and 76.1–90% with entecavir15,16 have been reported. At two years, the rates increased. Using lamivudine, a negative VL was observed in 56% at one year; however, globally, this rate was around 70%.17,18 We could not assess patients’ adherence to treatment, and poor adhrence may have been responsible for lower therapeutic success.
There was a 42% response rate to treatment with interferon. In the 16 HBeAg+ patients who underwent this treatment, five (31.2%) had HBeAg seroconversion. In other studies, this rate varied from 19 to 33%,16,19,20 and up to 30% maintained VL suppression after ending treatment.21 Despite reports of the possibility of seroconversion of HBsAg due to interferon,22 there was no patient who turned anti-HBs positive after interferon use until the end of the study. This response associated with interferon tends to be late4 and it is not known if a longer observation after medication use could change these results.
Eight percent of our patients received entecavir plus tenofovir, but only 1.9% had resistance to entecavir. The medical team observed fluctuations in VL of some patients taking entecavir prompting to adding tenofovir. At the time of tenofovir addition resistance was thought to exist but these fluctuations may have occurred due to irregular delivery of entecavir by the pharmacy or to lack of patient adherence to treatment.
HBeAg seroconversion varies from 20 to 40% in the literature,3,16 which is consistent with our results. Seroconversion of HBsAg remains low globally.4,18 About 10% of our patients had HBsAg seroconversion in this analysis, although only 3.1% did so with antiviral treatment.
Factors associated with poor prognosisIn our analysis, initial elevated VL and ALT were independent risk factors for progression to LC; this has been previously demonstrated in other studies.23,24 Approximately 15–40% of patients with CHB progress to LC, increasing the risk of HCC.7 In an epidemiological survey published in Brazil, LC was present in 18.5% of 3913 patients with hepatitis B.10
All of our patients with HCC had LC, the majority were male, and our study demonstrated that LC and HCC are independent risk factors for death. HCC is a leading cause of death among patients with CHB. The incidence of HCC remains high, even in large centers, and cirrhotic patients are at greater risk.18 Male gender, viral coinfection, alcohol use, and high VL are also risk factors,3 as well as HBeAg positive status.19,25
However, in our analysis, HBeAg was not associated with LC, HCC, or death. Antiviral treatment may have influenced this finding, since only 9/64 (14.1%) patients in the HBeAg+ group had never been treated. It has been shown that effective antiviral treatment appears to reduce the risk of HCC, especially when patients maintain viral suppression for prolonged periods of time.26–29 It is important to identify patients in need for treatment to prevent this outcome.
Elevated VL was a risk factor for development of cirrhosis, HCC, and death, as shown by other studies.24 We found that initially elevated ALT level was significantly associated with LC and death, but not with HCC. Other aspects may have influenced the incidence of HCC, as alcohol consumption. Here we analyzed only ALT, not AST. It may have been a confounding factor.
The survival of our patients with CHB in the first and second years after LT was lower than that reported in other countries,16 but it is not different from the overall LT survival in Brazil including all etiologies. According to data from the Brazilian Association of Organ Transplantation, the overall survival after transplantation is 74% in the first, and 72% in the second year.30
Our study has some limitations. Since it was retrospective, we could neither evaluate the influence of alcohol abuse or viral genotype in this population, nor the age at first infection. Additionally, we were unable to consider the role of quantification of HBsAg and HBeAg in the prediction of seroconversion.
ConclusionsWe demonstrated that the presence of HBeAg was not associated with a worse prognosis, but we should value the first determinations of ALT and VL because if high, they can select patients at higher risk for worse outcomes. Further efforts must be made to prevent progression to LC and HCC, as these were the main factors associated with death in our patients with CHB.
Conflicts of interestThe authors declare no conflicts of interest.
Medical writing support was provided by Editage (www.editage.com.br).