HIV/AIDS epidemic is not well controlled, and multiple sexual behavior factors help explain high rates of HIV infection among men who have sex with men (MSM). This article proposes to exam the use of a potential risk behavior score for HIV infection, based on the type and number of sexual partners, and condom use, and their associated factors in a sample of MSM in Brazil. A cross sectional RDS (Respondent Driven Sampling) study was performed among 3738 MSM aged 18+ years old from ten Brazilian cities. The risk behavior score was composed by the number of male partners and anal condom use in the last year with steady, casual, and commercial partners. Most participants were 25+ years old (58.1%), non-white (83.1%), and single (84.9%). Final weighted ordinal logistic model showed that age≤25 years old (p=0.037), homosexual or bisexual identity (p<0.001), sexual initiation before 15-year-old (p<0.001), having sex with men only in the last 12 months (p<0.001), frequent alcohol and illicit drug use (p<0.001), and use of local sites to meet sexual partners in the last month were independently associated with higher scores of risky behavior. Specific strategies should be developed aimed at the MSM population. Additionally, pre-exposed prophylaxis (Prep) should be considered for those at higher score as a strategy for reducing risk for HIV infection in this population.
Recent data from the Joint United Nations Programme on HIV/AIDS (UNAIDS) indicate stable or declining rates of HIV infection worldwide.1 However, the HIV epidemic is not well controlled in many regions, especially among key populations, including young men who have sex with men (MSM), among which HIV prevalence and incidence rates are higher than in the general population irrespective of the world region.2 Although determinants of HIV transmission are multifactorial, sexual behavior factors still play a major role among MSM, including type of sexual practices,3 lack of condom use, number and type of sexual partnerships, concurrency, and age of sexual initiation.4,5 These factors may help explain the high rates of HIV infection among MSM worldwide, especially in countries with concentrated epidemics.
Due to the complexity of the dynamics of HIV transmission, complete assessment of sexual risk behavior may be difficult and, when based solely on only one characteristic (e.g. condom use), estimates may often be imprecise and underestimated.6 In general, number of possible HIV exposures, which reflects risk of infection, depends not only on the number of unprotected sexual acts, but also on the number and characteristics of sex partners. It is not uncommon to find lack of statistical associations of single indicators of risky behavior with HIV infection among key populations.7,8 Although methodological issues are always potential explanations (e.g. lack of statistical power, poor measurements, study design), these components may not sufficiently reflect risk behavior when analyzed separately.9 Moreover, these behaviors are most likely statistically correlated and therefore, it may not be reasonable to analyze them separately as independent variables.6,9
Social networks and pattern of contacts of HIV infected individuals may also play an important role in the transmission chain.10 Frequent unprotected sexual contacts with one partner, who is not infected with HIV, does not confer much risk to the individual. Similarly, a high number of sexual partners potentially increases the chances of someone having sex with recent HIV-infected partners with high infectivity due to high viral load in early infection stage.11 For example,4 assessing the incidence of HIV among MSM by a meta-analysis of 12 studies in China have shown that syphilis infection (relative risk [RR]=3.33), multiple sexual partners (RR=2.81) and unprotected receptive anal sex in the last six months (RR=3.88) were significant risk factors that accounted for HIV seroconversion among MSM.
Thus, it is reasonable to examine sexual risk behavior not only through a single indicator (e.g., condom use), but rather through a combination of variables, including number and type of sexual partnerships, condom use in different types of sexual practices, and some characteristics of sexual partners.12 This would enable a better assessment of an overall sexual risk behavior among key populations, with potential benefits for improved screening for HIV, and prevention and treatment efforts. This article proposes to exam the use of a potential score of sexual risk behavior for HIV infection, based on the type and number of sexual partners, condom use, and their associated factors in a sample of men who have sex with men in ten Brazilian cities.
Material and methodsStudy designThis work is embedded in the project entitled “Behavior, attitudes, practices and prevalence of HIV and syphilis among men who have sex with men (MSM) in 10 Brazilian cities”.13 This is a cross-sectional study whose primary objective was to establish a baseline to be used for monitoring the HIV epidemic, including sexual risk behavior, among a national sample of MSM in the country. The project was approved by the Research Ethical Committee of the Federal University of Ceará, and by The National Council on Ethics in Research (CONEP 14494/2008). Participants were asked to sign a written informed consent and data collection occurred between October 2008 and June 2009.
Population and proceduresParticipants were MSM aged 18 years old or more residing in the following cities: Manaus, Recife, Salvador, Belo Horizonte, Rio de Janeiro, Santos, Curitiba, Itajaí, Brasília, and Campo Grande. The cities were previously chosen by the Department of STD, AIDS and Viral Hepatitis (DSAVH), Ministry of Health, considering regional, socioeconomic, and cultural diversity. Eligible participants should have had at least one sexual relationship with another man in the 12 months preceding the interview.
To obtain the desired sample size at each center, set a priori between 250 and 350 participants per city by the DSAVH, Respondent Driven Sampling (RDS)14,15 was used to recruit participants, previously described.13 The first recruiters, named seeds, were selected during a preliminary formative research (focus groups and semi-structured interviews) according to age and schooling. In each municipality, each initial seed received three non-falsifiable coupons to distribute to their acquaintances within their social network. Individuals who came to the study sites with a valid coupon and who met the inclusion criteria comprised the first wave of the study, each receiving three new coupons. Thereafter, similar subsequent procedures were carried out until the planned sample size was reached in each city.
Data collection was conducted through face-to-face interviews with a structured standardized questionnaire which contained questions on sociodemographic data, sexual behavior and drug use, network and social context, health care, access to condoms and sources of information about sexually transmitted infections. In addition to the interview, participants were also invited to undergo HIV and syphilis testing, using rapid testing standard procedures at the time of data collection, as recommended by the DSAVH.16
Outcome and explanatory variablesFor this analysis, risk behavior for HIV infection was defined as a composite score based on the following variables: (a) number of male sexual partners in the last 12 months; (b) condom use in anal intercourse (receptive or insertive) with men in the past 12 months; and, (c) type of sexual partnership, i.e., stable, casual, or commercial. Stable partner was defined as ‘boyfriend, companion or someone with whom the individual lived and there was no exchange of money for sex’. Casual partner was defined as ‘someone with whom the individual had sex one or more times without any regularity and there was no exchange of money for sex’. Moreover, commercial partner was defined as ‘someone with whom the individual had paid or received money for sex’.
The following values (scores) were attributed to the number of male sexual partners for each type of sexual partner, e.g., stable (St), casual (Ca) or commercial (Co): none=0, only one=1, two to four=2, five to ten=3, and more than ten partners=4. Similarly, scores for condom use during anal intercourse in the past 12 months were: did not have anal intercourse=0, always used condoms=1, used condoms more than half of the times=2, used condoms less than half of the times=3, and never used condoms during anal intercourse=4. The two scores obtained, number of sexual partners and condom use, were then multiplied, separately, for each type of sexual partnership (stable, casual, or commercial). The final overall score was calculated by the sum of the scores obtained for each type of sexual partnership, ranging from 0-48 points, where higher scores indicate a greater degree of sexual risk behavior. The score calculation is shown in the following formula: Overall Score=(Score #Partners×Score Condom Use)St+(Score #Partners×Score Condom Use)Ca+(Score #Partners×Score Condom Use)Co.
The explanatory variables analyzed were: sociodemographic (age, race, education, marital status [single/living alone, married/living with a female partner, living with a male partner]), and behavioral (age of sexual initiation, alcohol and drug use, looking for places/sites to meet sexual partners, self-reported sexual identity, and history of forced sexual intercourse before 14 years of age). The age of sexual initiation was defined as the age at first sexual intercourse reported by the individual, and it was categorized with a cut-off at 15 years old. Self-reported sexual identity was classified as heterosexual, bisexual, or homosexual (“gay” and “MSM” were included in the latter category). To assess the performance of the risk behavior score we also compared the HIV and syphilis serology results with low, medium, and high score.
Statistical analysisDescriptive analysis was carried out and means and central tendency measures were calculated for continuous variables, and proportions were calculated for categorical variables. Data from the ten cities were combined and weighted by the inverse of each participant's social network size13 and by the estimated proportion of MSM in each city relative to the total sample.17,18
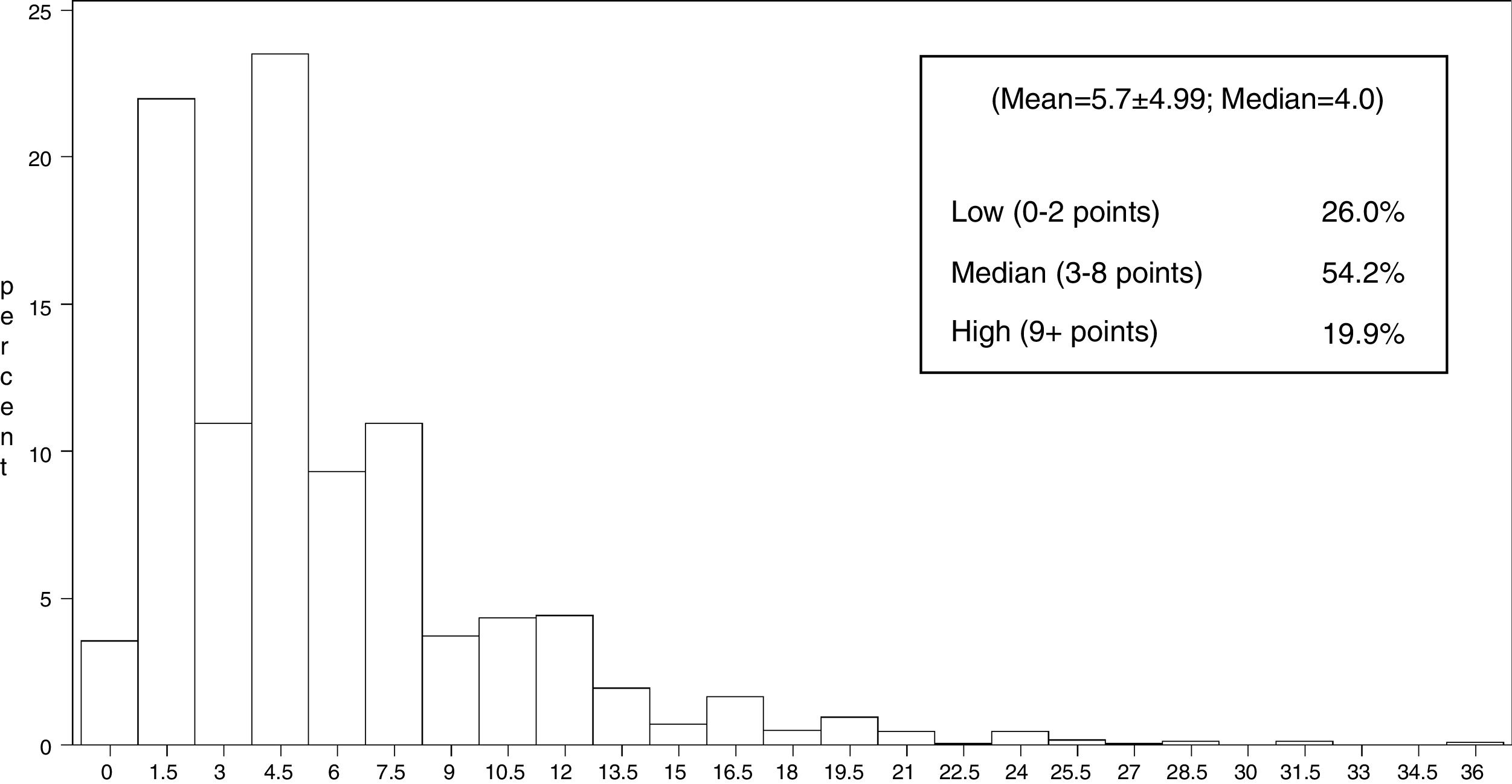
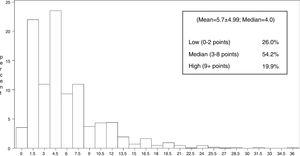
The distribution of the risk score was assessed and categorized (based on its quartile distribution) as: low risk (0–2 points), medium risk (3–8 points) and high risk (9+ points). Individuals without information on the number of sexual partners and/or condom use were excluded from this analysis. The association between explanatory variables and HIV risk behavior score was verified by univariate and multivariate weighted ordinal logistic regression, considering the outcome as an ordinal variable – low, medium, and high risk behavior scores, thus producing a proportional Odds Ratio with 95% confidence interval. Variables with p-values<0.20 in the univariate analysis were selected for initial multivariate modeling. We began with a full model and variables were chosen using a backwards procedure. Only those with p-value<0.05 were retained in the final model. The statistical association of each variable was assessed by means of the Wald test while the final fitness of the model was assessed by Hosmer–Lemeshow test. To assess the performance of the proposed score, the final model obtained was re-run including HIV and syphilis serology in the model in order to verify the association between the risk score and positivity for these infections.
The data analysis was conducted using SAS® Software (SAS Institute Inc., Cary, NC, USA) and R Package® (R Foundation for Statistical Computing, Vienna, Austria).
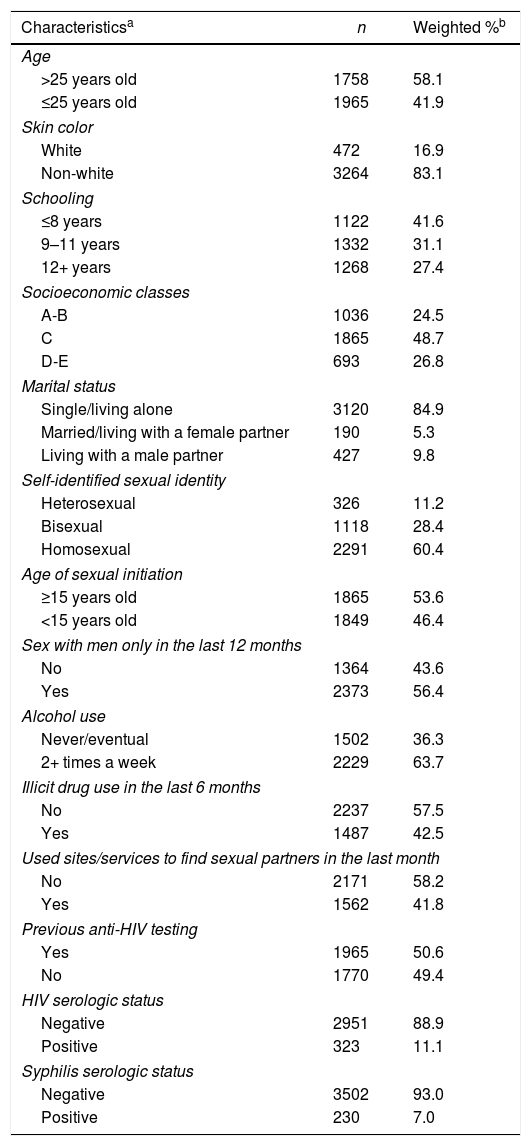
ResultsAmong 4048 recruited MSM, 188 (4.6%) were ineligible and only one refused to participate, resulting in a sample of 3859 participants. Among these, 3738 (96.9%) had complete information on the number of sexual partners and condom use during sexual intercourse in the last 12 months and were included in this analysis. Most MSM in this sample were over 25 years old (58.1%), non-white (83.1%) and single or living alone (84.9%), while 41.6% reported having eight or fewer years of education (Table 1). Almost two thirds of the respondents (63.7%) reported frequent use of alcohol (two or more times per week) and 42.5% reported using illicit drugs in the past six months. Homosexual identity was reported by 60.4%, and 46.4% had their sexual debut before 15 years old. A large proportion had never been tested for HIV before the study (49.4%) while 11.1% were found to be HIV positive during the study – among these, 49.6% were not aware they were positive. Overall, 11.1% and 7.0% of this sample of MSM have positive test for HIV or syphilis, respectively.
Characteristics of the sample of men who have sex with men (n=3738).
| Characteristicsa | n | Weighted %b |
|---|---|---|
| Age | ||
| >25 years old | 1758 | 58.1 |
| ≤25 years old | 1965 | 41.9 |
| Skin color | ||
| White | 472 | 16.9 |
| Non-white | 3264 | 83.1 |
| Schooling | ||
| ≤8 years | 1122 | 41.6 |
| 9–11 years | 1332 | 31.1 |
| 12+ years | 1268 | 27.4 |
| Socioeconomic classes | ||
| A-B | 1036 | 24.5 |
| C | 1865 | 48.7 |
| D-E | 693 | 26.8 |
| Marital status | ||
| Single/living alone | 3120 | 84.9 |
| Married/living with a female partner | 190 | 5.3 |
| Living with a male partner | 427 | 9.8 |
| Self-identified sexual identity | ||
| Heterosexual | 326 | 11.2 |
| Bisexual | 1118 | 28.4 |
| Homosexual | 2291 | 60.4 |
| Age of sexual initiation | ||
| ≥15 years old | 1865 | 53.6 |
| <15 years old | 1849 | 46.4 |
| Sex with men only in the last 12 months | ||
| No | 1364 | 43.6 |
| Yes | 2373 | 56.4 |
| Alcohol use | ||
| Never/eventual | 1502 | 36.3 |
| 2+ times a week | 2229 | 63.7 |
| Illicit drug use in the last 6 months | ||
| No | 2237 | 57.5 |
| Yes | 1487 | 42.5 |
| Used sites/services to find sexual partners in the last month | ||
| No | 2171 | 58.2 |
| Yes | 1562 | 41.8 |
| Previous anti-HIV testing | ||
| Yes | 1965 | 50.6 |
| No | 1770 | 49.4 |
| HIV serologic status | ||
| Negative | 2951 | 88.9 |
| Positive | 323 | 11.1 |
| Syphilis serologic status | ||
| Negative | 3502 | 93.0 |
| Positive | 230 | 7.0 |
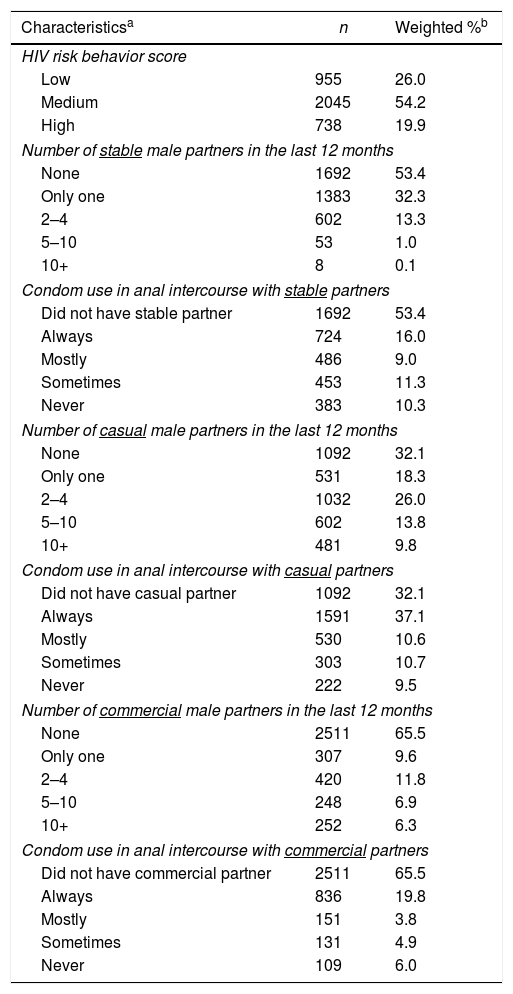
Our results indicate that 46.6%, 67.9%, and 34.5% reported having had at least one stable, one casual, or one commercial male partner in the past 12 months. It should be noted that concomitance between type of partners occurred mostly among stable-casual (27.8%) and stable-casual-commercial (18.1%) partners. In addition, number of male sexual partners varied according to type of partnership. While only 14.4% had two or more stable partners, 25.0% had two or more commercial partners, and 49.6% had two or more casual partners. Also, inconsistent condom use during anal intercourse was common in all types of sexual partnerships (Table 2), but it was higher during anal intercourse with stable partners (64.6%; n=1322/2046) followed by anal intercourse with casual (39.9%; n=1055/2646) or commercial male partners (31.9%; n=391/1227) in the past 12 months. Finally, as a reflection of the combination of these indicators, the HIV risk behavior score varied from 0 to 36 points (mean=5.7±4.99; median=4) (see Histogram – Fig. 1) with 26.0%, 54.2%, and 19.9% classified as low (0–2 points), medium (3–8 points), or high risk (9+ points), respectively (Table 2).
Description of sexual behavior characteristics of the sample of men who have sex with men (n=3738).
| Characteristicsa | n | Weighted %b |
|---|---|---|
| HIV risk behavior score | ||
| Low | 955 | 26.0 |
| Medium | 2045 | 54.2 |
| High | 738 | 19.9 |
| Number of stable male partners in the last 12 months | ||
| None | 1692 | 53.4 |
| Only one | 1383 | 32.3 |
| 2–4 | 602 | 13.3 |
| 5–10 | 53 | 1.0 |
| 10+ | 8 | 0.1 |
| Condom use in anal intercourse with stable partners | ||
| Did not have stable partner | 1692 | 53.4 |
| Always | 724 | 16.0 |
| Mostly | 486 | 9.0 |
| Sometimes | 453 | 11.3 |
| Never | 383 | 10.3 |
| Number of casual male partners in the last 12 months | ||
| None | 1092 | 32.1 |
| Only one | 531 | 18.3 |
| 2–4 | 1032 | 26.0 |
| 5–10 | 602 | 13.8 |
| 10+ | 481 | 9.8 |
| Condom use in anal intercourse with casual partners | ||
| Did not have casual partner | 1092 | 32.1 |
| Always | 1591 | 37.1 |
| Mostly | 530 | 10.6 |
| Sometimes | 303 | 10.7 |
| Never | 222 | 9.5 |
| Number of commercial male partners in the last 12 months | ||
| None | 2511 | 65.5 |
| Only one | 307 | 9.6 |
| 2–4 | 420 | 11.8 |
| 5–10 | 248 | 6.9 |
| 10+ | 252 | 6.3 |
| Condom use in anal intercourse with commercial partners | ||
| Did not have commercial partner | 2511 | 65.5 |
| Always | 836 | 19.8 |
| Mostly | 151 | 3.8 |
| Sometimes | 131 | 4.9 |
| Never | 109 | 6.0 |
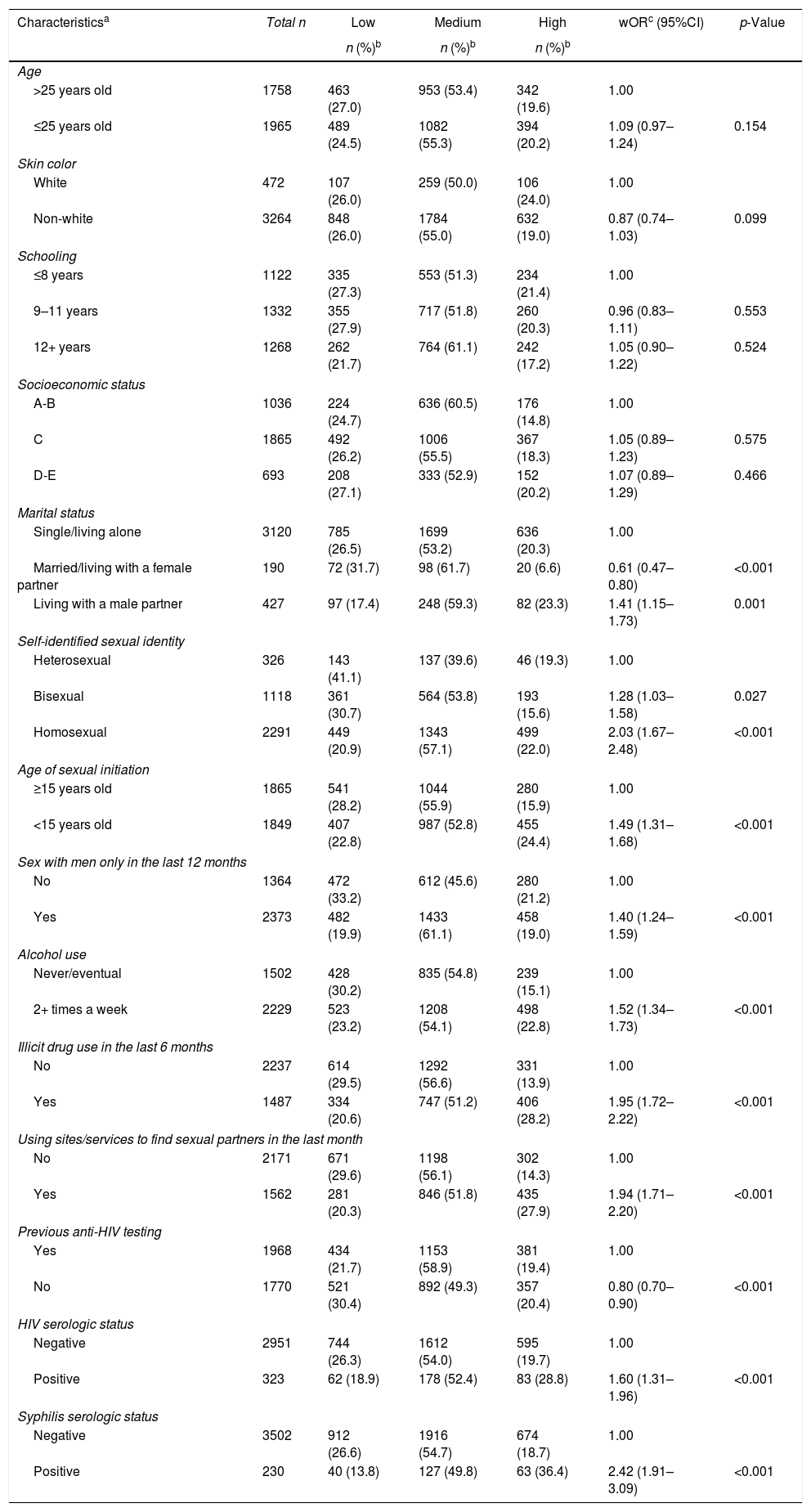
Univariate analysis of the HIV risk behavior score is shown in Table 3. There was a much lower proportion of high risk score (6.6%) among those who lived with a female partner or were married compared with MSM who lived alone (20.3%) or with a male partner (23.3%) (p<0.001). Similarly, individuals who self-identified themselves as homosexual had greater proportions of medium and high risk score (57.1% and 22.0%, respectively) compared with those with heterosexual identity (39.6% and 19.3%) (p<0.001). In the same way, 61.1% and 19.0% of MSM who reported having sex with men only had medium and high risk scores, respectively, compared with 45.6% and 21.2% of those who reported having sex with both men and women. Moreover, among those who initiated sexual activity before 15 years old, 24.4% had high risk score, compared with 15.9% of those who reported sexual initiation with older age (p<0.001). Individuals who consumed alcohol more frequently and who had a history of drug use in the last six months also had a higher proportion of high risk score (22.8 and 28.2%, respectively, p<0.001). Higher proportion of high risk score was also found among those using sites/services to find partners (27.9%, p<0.001), and among those who had ever been tested for HIV, 21.7%, 58.9%, and 19.4% had low, medium and high risk score, respectively, compared to 30.4%, 49.3%, and 20.4% of those who had never been tested for HIV before (p<0.001). Finally, among HIV-negative individuals, 19.7% had high risk score, compared to 28.8% of HIV-positive individuals (p<0.001). Similarly, 18.7% of participants with negative test for syphilis and 36.4% of those with positive test had high risk score (p<0.001). Therefore, the higher the risk score, the higher the proportion of subjects with positive serology for HIV and syphilis.
Univariate weighted ordinal logistic regression model of factors associated with risk behavior score among men who have sex with men, Brazil (n=3738).
| Characteristicsa | Total n | Low | Medium | High | wORc (95%CI) | p-Value |
|---|---|---|---|---|---|---|
| n (%)b | n (%)b | n (%)b | ||||
| Age | ||||||
| >25 years old | 1758 | 463 (27.0) | 953 (53.4) | 342 (19.6) | 1.00 | |
| ≤25 years old | 1965 | 489 (24.5) | 1082 (55.3) | 394 (20.2) | 1.09 (0.97–1.24) | 0.154 |
| Skin color | ||||||
| White | 472 | 107 (26.0) | 259 (50.0) | 106 (24.0) | 1.00 | |
| Non-white | 3264 | 848 (26.0) | 1784 (55.0) | 632 (19.0) | 0.87 (0.74–1.03) | 0.099 |
| Schooling | ||||||
| ≤8 years | 1122 | 335 (27.3) | 553 (51.3) | 234 (21.4) | 1.00 | |
| 9–11 years | 1332 | 355 (27.9) | 717 (51.8) | 260 (20.3) | 0.96 (0.83–1.11) | 0.553 |
| 12+ years | 1268 | 262 (21.7) | 764 (61.1) | 242 (17.2) | 1.05 (0.90–1.22) | 0.524 |
| Socioeconomic status | ||||||
| A-B | 1036 | 224 (24.7) | 636 (60.5) | 176 (14.8) | 1.00 | |
| C | 1865 | 492 (26.2) | 1006 (55.5) | 367 (18.3) | 1.05 (0.89–1.23) | 0.575 |
| D-E | 693 | 208 (27.1) | 333 (52.9) | 152 (20.2) | 1.07 (0.89–1.29) | 0.466 |
| Marital status | ||||||
| Single/living alone | 3120 | 785 (26.5) | 1699 (53.2) | 636 (20.3) | 1.00 | |
| Married/living with a female partner | 190 | 72 (31.7) | 98 (61.7) | 20 (6.6) | 0.61 (0.47–0.80) | <0.001 |
| Living with a male partner | 427 | 97 (17.4) | 248 (59.3) | 82 (23.3) | 1.41 (1.15–1.73) | 0.001 |
| Self-identified sexual identity | ||||||
| Heterosexual | 326 | 143 (41.1) | 137 (39.6) | 46 (19.3) | 1.00 | |
| Bisexual | 1118 | 361 (30.7) | 564 (53.8) | 193 (15.6) | 1.28 (1.03–1.58) | 0.027 |
| Homosexual | 2291 | 449 (20.9) | 1343 (57.1) | 499 (22.0) | 2.03 (1.67–2.48) | <0.001 |
| Age of sexual initiation | ||||||
| ≥15 years old | 1865 | 541 (28.2) | 1044 (55.9) | 280 (15.9) | 1.00 | |
| <15 years old | 1849 | 407 (22.8) | 987 (52.8) | 455 (24.4) | 1.49 (1.31–1.68) | <0.001 |
| Sex with men only in the last 12 months | ||||||
| No | 1364 | 472 (33.2) | 612 (45.6) | 280 (21.2) | 1.00 | |
| Yes | 2373 | 482 (19.9) | 1433 (61.1) | 458 (19.0) | 1.40 (1.24–1.59) | <0.001 |
| Alcohol use | ||||||
| Never/eventual | 1502 | 428 (30.2) | 835 (54.8) | 239 (15.1) | 1.00 | |
| 2+ times a week | 2229 | 523 (23.2) | 1208 (54.1) | 498 (22.8) | 1.52 (1.34–1.73) | <0.001 |
| Illicit drug use in the last 6 months | ||||||
| No | 2237 | 614 (29.5) | 1292 (56.6) | 331 (13.9) | 1.00 | |
| Yes | 1487 | 334 (20.6) | 747 (51.2) | 406 (28.2) | 1.95 (1.72–2.22) | <0.001 |
| Using sites/services to find sexual partners in the last month | ||||||
| No | 2171 | 671 (29.6) | 1198 (56.1) | 302 (14.3) | 1.00 | |
| Yes | 1562 | 281 (20.3) | 846 (51.8) | 435 (27.9) | 1.94 (1.71–2.20) | <0.001 |
| Previous anti-HIV testing | ||||||
| Yes | 1968 | 434 (21.7) | 1153 (58.9) | 381 (19.4) | 1.00 | |
| No | 1770 | 521 (30.4) | 892 (49.3) | 357 (20.4) | 0.80 (0.70–0.90) | <0.001 |
| HIV serologic status | ||||||
| Negative | 2951 | 744 (26.3) | 1612 (54.0) | 595 (19.7) | 1.00 | |
| Positive | 323 | 62 (18.9) | 178 (52.4) | 83 (28.8) | 1.60 (1.31–1.96) | <0.001 |
| Syphilis serologic status | ||||||
| Negative | 3502 | 912 (26.6) | 1916 (54.7) | 674 (18.7) | 1.00 | |
| Positive | 230 | 40 (13.8) | 127 (49.8) | 63 (36.4) | 2.42 (1.91–3.09) | <0.001 |
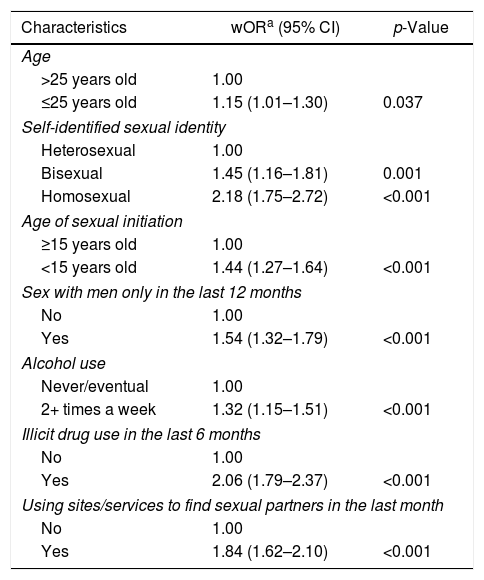
Final ordinal logistic regression model (Table 4) showed that age of 25 years or less (p=0.037), self-reported sexual identity as homosexual (p<0.001) or bisexual (p=0.001), sexual initiation before 15 years old (p<0.001), having had sex with men only in the last 12 months (p<0.001), frequent use of alcohol (p<0.001), illicit drug use in the last 6 months (p<0.001), and using sites/services to meet sexual partners in the last month (p<0.001) were independently associated with higher scores of risky behavior.
Final multivariate weighted ordinal logistic regression model of factors associated with risk behavior score among men who have sex with men, Brazil (n=3738).
| Characteristics | wORa (95% CI) | p-Value |
|---|---|---|
| Age | ||
| >25 years old | 1.00 | |
| ≤25 years old | 1.15 (1.01–1.30) | 0.037 |
| Self-identified sexual identity | ||
| Heterosexual | 1.00 | |
| Bisexual | 1.45 (1.16–1.81) | 0.001 |
| Homosexual | 2.18 (1.75–2.72) | <0.001 |
| Age of sexual initiation | ||
| ≥15 years old | 1.00 | |
| <15 years old | 1.44 (1.27–1.64) | <0.001 |
| Sex with men only in the last 12 months | ||
| No | 1.00 | |
| Yes | 1.54 (1.32–1.79) | <0.001 |
| Alcohol use | ||
| Never/eventual | 1.00 | |
| 2+ times a week | 1.32 (1.15–1.51) | <0.001 |
| Illicit drug use in the last 6 months | ||
| No | 1.00 | |
| Yes | 2.06 (1.79–2.37) | <0.001 |
| Using sites/services to find sexual partners in the last month | ||
| No | 1.00 | |
| Yes | 1.84 (1.62–2.10) | <0.001 |
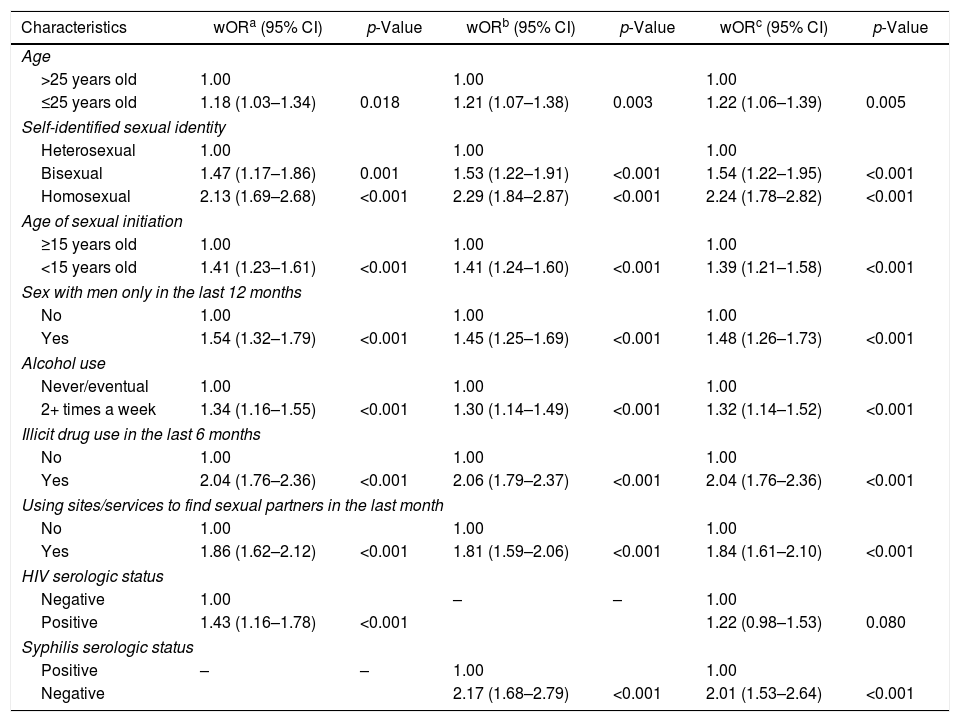
In the present analysis, the HIV risk behavior score showed adequate performance for capturing the associations with prevalent HIV and syphilis infections (Table 5). As shown, there was an independent association between HIV (p<0.001) or syphilis (p<0.001) with the risk score while all the remaining variables showing similar wOR (magnitude and direction) as compared with the final model without either HIV or syphilis. However, when modeling together, HIV infection showed a borderline association (p=0.08), most likely due to power considerations.
Final multivariate weighted ordinal logistic regression models of factors associated (including HIV and/or syphilis serologic status) with risk behavior score among men who have sex with men, Brazil (n=3738).
| Characteristics | wORa (95% CI) | p-Value | wORb (95% CI) | p-Value | wORc (95% CI) | p-Value |
|---|---|---|---|---|---|---|
| Age | ||||||
| >25 years old | 1.00 | 1.00 | 1.00 | |||
| ≤25 years old | 1.18 (1.03–1.34) | 0.018 | 1.21 (1.07–1.38) | 0.003 | 1.22 (1.06–1.39) | 0.005 |
| Self-identified sexual identity | ||||||
| Heterosexual | 1.00 | 1.00 | 1.00 | |||
| Bisexual | 1.47 (1.17–1.86) | 0.001 | 1.53 (1.22–1.91) | <0.001 | 1.54 (1.22–1.95) | <0.001 |
| Homosexual | 2.13 (1.69–2.68) | <0.001 | 2.29 (1.84–2.87) | <0.001 | 2.24 (1.78–2.82) | <0.001 |
| Age of sexual initiation | ||||||
| ≥15 years old | 1.00 | 1.00 | 1.00 | |||
| <15 years old | 1.41 (1.23–1.61) | <0.001 | 1.41 (1.24–1.60) | <0.001 | 1.39 (1.21–1.58) | <0.001 |
| Sex with men only in the last 12 months | ||||||
| No | 1.00 | 1.00 | 1.00 | |||
| Yes | 1.54 (1.32–1.79) | <0.001 | 1.45 (1.25–1.69) | <0.001 | 1.48 (1.26–1.73) | <0.001 |
| Alcohol use | ||||||
| Never/eventual | 1.00 | 1.00 | 1.00 | |||
| 2+ times a week | 1.34 (1.16–1.55) | <0.001 | 1.30 (1.14–1.49) | <0.001 | 1.32 (1.14–1.52) | <0.001 |
| Illicit drug use in the last 6 months | ||||||
| No | 1.00 | 1.00 | 1.00 | |||
| Yes | 2.04 (1.76–2.36) | <0.001 | 2.06 (1.79–2.37) | <0.001 | 2.04 (1.76–2.36) | <0.001 |
| Using sites/services to find sexual partners in the last month | ||||||
| No | 1.00 | 1.00 | 1.00 | |||
| Yes | 1.86 (1.62–2.12) | <0.001 | 1.81 (1.59–2.06) | <0.001 | 1.84 (1.61–2.10) | <0.001 |
| HIV serologic status | ||||||
| Negative | 1.00 | – | – | 1.00 | ||
| Positive | 1.43 (1.16–1.78) | <0.001 | 1.22 (0.98–1.53) | 0.080 | ||
| Syphilis serologic status | ||||||
| Positive | – | – | 1.00 | 1.00 | ||
| Negative | 2.17 (1.68–2.79) | <0.001 | 2.01 (1.53–2.64) | <0.001 | ||
Our analyses indicate that the proposed score is a reasonable way of capturing risk behavior in this national sample of Brazilian MSM. The results demonstrate that only 26.0% were at a lower risk with 54.2% at medium risk, and a worrisome 20.0% at a very high risk for HIV infection. As expected, this is reflecting the combination of number of stable, casual, and commercial sexual partners with a high proportion of inconsistent condom use in anal intercourse by these partners in the last 12 months. Similarly to the score presented, several other studies have assessed the sexual behavior through a combination of multiple variables, although there are methodological differences that may affect direct comparisons.,12 analyzing data from a randomized trial of circumcision in Kenya, proposed a scale of sexual risk propensity, which contained 18 items related to condom use, number and type of sexual partners, concurrency, and perception about behavior of partners. These authors demonstrated a significant association between the risk scale and the incidence of STI and HIV. Darke et al.19 developed a questionnaire to measure primary risk behavior among injecting drug users. The HIV Risk-taking Behavior Scale (HRBS) is composed of two sections, one for drugs and one for sexual activity. Issues related to sexual behavior include number of sexual partners, condom use with regular, casual, and commercial partners, and history of anal intercourse. Similarly, Menza et al.20 proposed a predictive model that included recent use of methamphetamine or inhaled nitrites, unprotected anal sex with a partner with positive or unknown HIV status, history of 10 or more male sexual partners in the previous year, and history of STI as predictors for HIV acquisition.
Our results are consistent with other risk behavior studies worldwide. There was a statistical significant association between sexual initiation before 15 years old and increased sexual risk behavior in the sample of MSM evaluated, indicating that the earlier the onset of sexual activity, the greater the chance of keeping risky behavior for HIV infection in adulthood. Similarly, a study conducted in Australia21 showed higher prevalence of STI and increased likelihood of practicing sexual risk behaviors among MSM who had earlier anal sex initiation, being the age of anal sex initiation a strong marker of HIV infection. Murphy et al.22 longitudinally examined the sexual behavior of a cohort of 8208 adolescents in the U.S. by means of a variable consisted of five categories, combining condom use and number of sexual partners, with higher scores reflecting greater risk. These authors reported that a high proportion of young people established an initial pattern of risky behavior that continued into adulthood. Moreover, it was observed that young people with a history of higher risk behavior initiated sexual life at a younger age than those with a history of lower risk behavior (14.6 and 17.0 years, respectively).
Almost half (47.0%) of the sample of MSM studied initiated sexual activity before 15 years old, a proportion significantly higher than the Brazilian adult general population (37% and 17% for men and women, respectively).18 The association between early sexual initiation and patterns of sexual risk behavior throughout life may be partially explained by the presence of selected personality traits, such as working memory ability (which expresses the cognitive ability to incorporate and manipulate relevant information and ignore deviant stimuli), impulsivity, sexual adventurism, and sensation seeking (characterized by the need for new and complex experiences, taking physical and social risks to experience them).23,24 Also, there is scientific evidence that early sexual debut in the general population is associated with a lack of information and proper sex education,25 drug abuse and emotional problems in adolescence,22 in addition to sociodemographic characteristics, including male sex, skin color, and low schooling.26 Intervention strategies should focus on young people even before the onset of sexual activity, including guidance on the importance of sexual behavior in HIV transmission, as well as the number of sexual partners and consistent and proper use of condoms, as part of school-based prevention programs.
In this analysis, HIV risk behavior score was higher among those who self-identified as homosexual, and this association could be explained by the fact that men who maintain bisexual relationships but identify themselves as heterosexuals practice safe sex more frequently to conceal their homosexual relations.27 The association of high risk behavior with having sex with men only and with searching sites to find sexual partners reinforces this hypothesis. However, information bias may have occurred, if men who had sex with men but identified themselves as heterosexual have reported safer sexual practices considering this answer to be more socially acceptable.
Alcohol and illicit drugs were also important markers of sexual risk behavior in this sample. Similarly, Reisner et al.28 found a negative association between alcohol use and the adoption of safer sexual practices. Another study demonstrated a greater chance of an individual not to use condoms during the last anal sex if he was under the effect of alcohol or cocaine.29 Frequently, a combination of drug use and sexual activity can be a way for the individual to justify their sexual risk behavior.30
The HIV risk behavior score proposed was built considering risky behavior as a complex construct, which is better assessed through a combination of indicators rather than the analysis of each variable separately.31 As shown, the proposed HIV risk behavior score was able to capture the association with HIV and syphilis infections, and it seems an adequate indicator for measuring HIV sexual risk behavior in this population. Moreover, the definition of the score as a continuous variable, with subsequent categorization makes the construct more informative and it can be used in sequential surveys to assess behavioral trends and effects of interventions applied in public health and health services.
Some limitations of the study should be mentioned. This is a sample of the adult Brazilian population of MSM obtained in 10 different cities, and differences in socio-cultural, geographical, and epidemiological settings are potential limiting factors to the representativeness of the general population of MSM in the country. Furthermore, RDS technique is potentially subject to selection bias, as sample characteristics can be influenced by seed selection, and individuals with certain characteristics tend to recruit peers with similar characteristics.32 However, estimates obtained by RDS are theoretically robust and tend to remove bias when the sample reaches the steady state after successive waves of recruiting.14,15 In addition, the data was properly weighted for the potential bias from the recruitment chains and the unequal probabilities of selection resulting from the different sizes of networks of each participant. Furthermore, behavioral variables were obtained by self-reporting, considering a period of up to 12 months, which may theoretically result in information/recall bias, despite the large sample size and the consistency of the results. Finally, because our data is based on a cross-sectional design we are only able to detect associations rather than direct causal effect. More studies are needed to validate our findings, specially incidence studies of HIV infection in key populations.
Nevertheless, the use of a summary score may be of practical use in various contexts, including health services. As new biomedical interventions proposed for key populations, including pre-exposure prophylaxis (PrEP), are proved effective,33,34 economic issues may be a barrier for their unrestricted use in many poor-resource countries. Currently, PrEP is not implemented in Brazil, as in many other countries and the use of a risk score for screening high risk key populations for PrEP use could be a cost-effective prevention strategy.
Informed consentInformed consent was obtained from all individual participants included in the study.
Financial supportThis research was supported by the Brazilian Ministry of Health/Secretariat of Health Surveillance/Department of STD, Aids and Viral Hepatitis through the Project of International Technical Cooperation AD/BRA/03/H34 between the Brazilian Government and the United Nations Office on Drugs and Crime – UNODC.
Ethical approvalAll procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflicts of interestThe authors declare no conflicts of interest.