Systemic lupus erythematosus (SLE) is an autoimmune disease resulting in inflammation-mediated multiorgan damage. In SLE patients, bacteria cause a higher rate of infections than viruses and/or fungi. Among SLE patients, bacterial infections is responsible for about 20–55% of death.1,2 Bacteremia frequently occurs in this population due to regular and continued usage of glucocorticoids and immunosuppressive agents for their treatment.3 In this study, we isolated the pathogenic bacteria from blood samples collected from the SLE patients in Southern India and they were analyzed for their resistance profile to standard antibiotics. A total of 100 blood samples were collected from SLE patients. Isolated bacterial cultures were further subjected to antibiotic sensitivity assay or antimicrobial resistance (AMR) profiling using Kirby-Bauer Disk Diffusion method according to CLSI guidelines.4 Ethical approval for this study was obtained from the Institutional Review Board of Madras Medical College, Chennai, India.
Age and sex-wise distribution of SLE patients revealed that about 91% of the infections were among females and only 9% were in males. Among the various age groups, 49% were in the age group of 21–30 years, followed by 22% in 31–40 years, 17% in 10–20 years, 10% in 41–50 years and 2% in 51–60 years. Among SLE patients, butterfly rash were recorded in 26% of the patients followed by a discoid rash in 41%, Reynaud’s phenomenon in 37%, fever in 31%, thick red, scaly red patches in 46%, hemolytic anemia in 18%, thrombocytopenia in 28%, arthritis in 54%, photosensitivity in 49%, oral ulcer in 24%, and alopecia in 16%. The SLE patients were treated with the following immunosuppressive drugs viz. prednisolone, cyclophosphamide, hydroxychloroquine, glococorticoids, and azathioprine. In this study, a total of 50 SLE patients had bloodstream infections and among them 45 patients had bacterial infection and five patients had fungal infection.
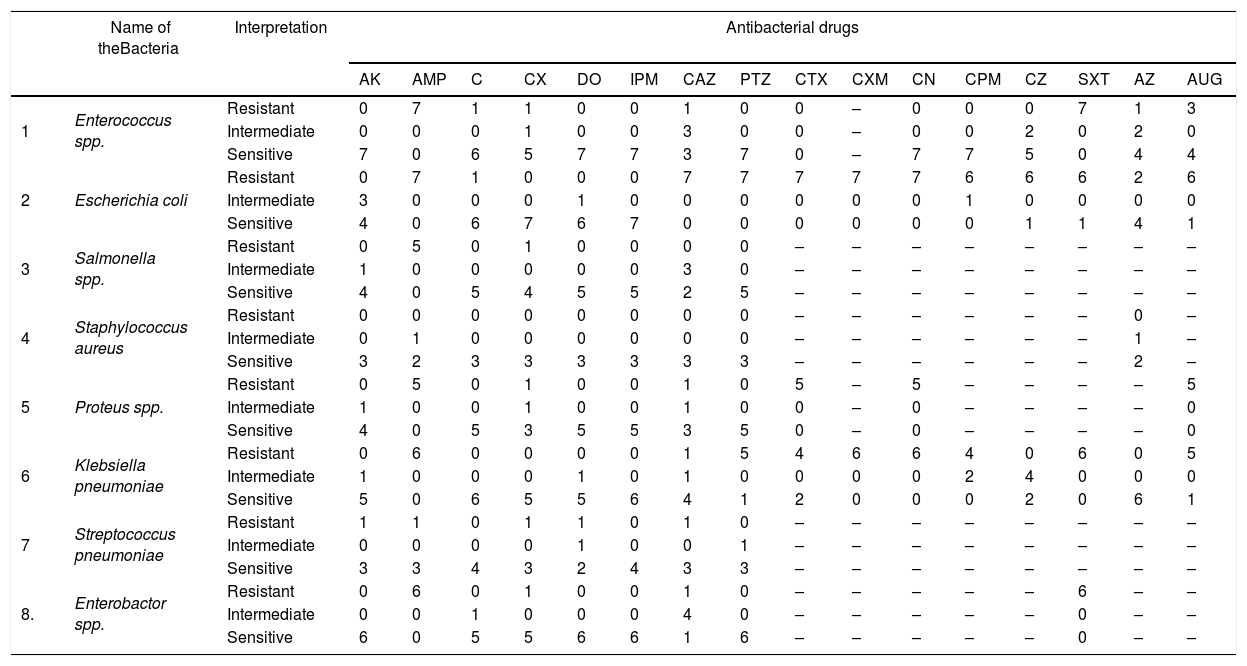
The antibiotic susceptibility profile was carried out only for the bacterial isolates. Escherichia coli isolated from blood specimens showed 100% resistance to ampicillin, ceftazidime, cefotaxime, cefuroxime, piperacillin, gentamicin, followed by 86% to amoxicillin/clavulanic acid, co-trimoxazole, cefepime and cefazolin (Table 1). Klebsiella pneumoniae showed 100% resistance to ampicillin, gentamicin, co-trimoxazole, cefuroxime followed by 83.3% to piperacillin, amoxicillin/clavulanic acid, and 66.7% to cefepime and cefotaxime. Salmonella spp. exhibited 100% resistance to ampicillin, enterobacter showed 100% resistance to ampicillin, co-trimoxazole, and 100% of Proteus mirabilis exhibited resistance to ampicillin, cefotaxime, amoxicillin/clavulanic acid, and gentamicin. Majority of the Staphylococcus aureus isolates showed resistance against penicillin (83.3%) followed by azithromycin (67%) (Table 1). Molecular screening for β-lactamase producing drug resistance genes showed that three isolates of E.coli were positive for blaTEM, two isolates of E.coli for blaCTX_M, and one isolate of K. pneumoniae showed positive for blaTEM, and blaCTX-M, and one isolate of P. mirabilis showed positive for blaTEM.
Antibacterial susceptibility pattern of bacterial isolates from blood samples of SLE patients.
| Name of theBacteria | Interpretation | Antibacterial drugs | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AK | AMP | C | CX | DO | IPM | CAZ | PTZ | CTX | CXM | CN | CPM | CZ | SXT | AZ | AUG | |||
| 1 | Enterococcus spp. | Resistant | 0 | 7 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | – | 0 | 0 | 0 | 7 | 1 | 3 |
| Intermediate | 0 | 0 | 0 | 1 | 0 | 0 | 3 | 0 | 0 | – | 0 | 0 | 2 | 0 | 2 | 0 | ||
| Sensitive | 7 | 0 | 6 | 5 | 7 | 7 | 3 | 7 | 0 | – | 7 | 7 | 5 | 0 | 4 | 4 | ||
| 2 | Escherichia coli | Resistant | 0 | 7 | 1 | 0 | 0 | 0 | 7 | 7 | 7 | 7 | 7 | 6 | 6 | 6 | 2 | 6 |
| Intermediate | 3 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | ||
| Sensitive | 4 | 0 | 6 | 7 | 6 | 7 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 | 1 | ||
| 3 | Salmonella spp. | Resistant | 0 | 5 | 0 | 1 | 0 | 0 | 0 | 0 | – | – | – | – | – | – | – | – |
| Intermediate | 1 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | – | – | – | – | – | – | – | – | ||
| Sensitive | 4 | 0 | 5 | 4 | 5 | 5 | 2 | 5 | – | – | – | – | – | – | – | – | ||
| 4 | Staphylococcus aureus | Resistant | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | – | – | – | – | – | – | 0 | – |
| Intermediate | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | – | – | – | – | – | – | 1 | – | ||
| Sensitive | 3 | 2 | 3 | 3 | 3 | 3 | 3 | 3 | – | – | – | – | – | – | 2 | – | ||
| 5 | Proteus spp. | Resistant | 0 | 5 | 0 | 1 | 0 | 0 | 1 | 0 | 5 | – | 5 | – | – | – | – | 5 |
| Intermediate | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | – | 0 | – | – | – | – | 0 | ||
| Sensitive | 4 | 0 | 5 | 3 | 5 | 5 | 3 | 5 | 0 | – | 0 | – | – | – | – | 0 | ||
| 6 | Klebsiella pneumoniae | Resistant | 0 | 6 | 0 | 0 | 0 | 0 | 1 | 5 | 4 | 6 | 6 | 4 | 0 | 6 | 0 | 5 |
| Intermediate | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 2 | 4 | 0 | 0 | 0 | ||
| Sensitive | 5 | 0 | 6 | 5 | 5 | 6 | 4 | 1 | 2 | 0 | 0 | 0 | 2 | 0 | 6 | 1 | ||
| 7 | Streptococcus pneumoniae | Resistant | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | – | – | – | – | – | – | – | – |
| Intermediate | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | – | – | – | – | – | – | – | – | ||
| Sensitive | 3 | 3 | 4 | 3 | 2 | 4 | 3 | 3 | – | – | – | – | – | – | – | – | ||
| 8. | Enterobactor spp. | Resistant | 0 | 6 | 0 | 1 | 0 | 0 | 1 | 0 | – | – | – | – | – | 6 | – | – |
| Intermediate | 0 | 0 | 1 | 0 | 0 | 0 | 4 | 0 | – | – | – | – | – | 0 | – | – | ||
| Sensitive | 6 | 0 | 5 | 5 | 6 | 6 | 1 | 6 | – | – | – | – | – | 0 | – | – | ||
AK-Amikacin; AMP-Ampicillin; C-Chloraphenicol; CX-Cefoxitin; DO-Doxycycline; IPM Imipenem; CAZ-Ceftazidime; PTZ-Piperacillin/Azobactam; CTX-Cefotaxime;CXM-Cefuroxime;CN-Gentamicin;CPM-Cefepime;CZ-Cefazolin; SXT-Co-trimaxozole; AZ-Azithromycin; AUG-Amoxicillin/Clavulanic acid.
The bacteria like E. coli, S. aurues and Salmonella spp. causes bloodstream infections in SLE patients and Salmonella spp. was the most common and major etiology among them.3,5Streptococcus pneumoniae caused about 10.3% of the bacteremia in SLE patients and about 54.5% of the infections caused by the microorganisms develop into severe SLE flare.6 In this study, Gram-negative bacteria like E. coli and Salmonella spp. were the major medically important etiology causing the majority of bloodstream infections. In case of Gram-positive bacteria Enterococcus spp. was the major causative agent with very high infection rate followed by S. aureus and S. pneumoniae. Reports of drug resistance among bacteria causing bloodstream infections in SLE patients are scarce. This study highlights drug resistant bacteria causing bloodstream infections among SLE patients which might be a risk factor and complicate the clinical management of these patients with available antibiotics. Bloodstream infections caused by drug resistant bacteria in SLE patients might prolong hospital stay, increase treatment cost, i.e., out-of-pocket expenditure for the treatment/management of secondary infections and may also increase the severity of the disease condition. The need of the hour is to establish rapid diagnosis and continued surveillance system to identify the causative bacterial agent. Adequate antibiogram would be helpful in implementing an appropriate therapeutic option for mitigating the drug resistant bloodstream infections in SLE patients.
Conflict of interestThe author declares no conflicts of interest.