Progressive multifocal leukoencephalopathy (PML) is a brain devastating demyelinating disease caused by the John Cunningham polyomavirus (JCV), that occurs almost exclusively in immunocompromised patients. Nonetheless, PML is a rare complication after solid organ transplantation, with an incidence of 1.24 per 1000 person years,1 and is mostly considered to be a consequence of viral reactivation.
Patient-to-patient transmission of JCV-associated PML was suspected in natalizumab treated patients.2,3 However, this was not reported after solid organ transplantation so far. Between July 2017 and April 2018, three kidney-transplant recipients followed in our center (81, 77, and 67 years-old, respectively) presented a definite PML (as defined by the American Academy of Neurology) at 5, 2 and 11 years post-transplantation, respectively. Two patients were receiving tacrolimus, mycophenolic acid and steroids, and the third patient was treated with belatacept, mycophenolic acid and steroids. As previously reported,4 despite discontinuation of immunosuppressants and use of immune checkpoint inhibitor therapy, all three patients died.
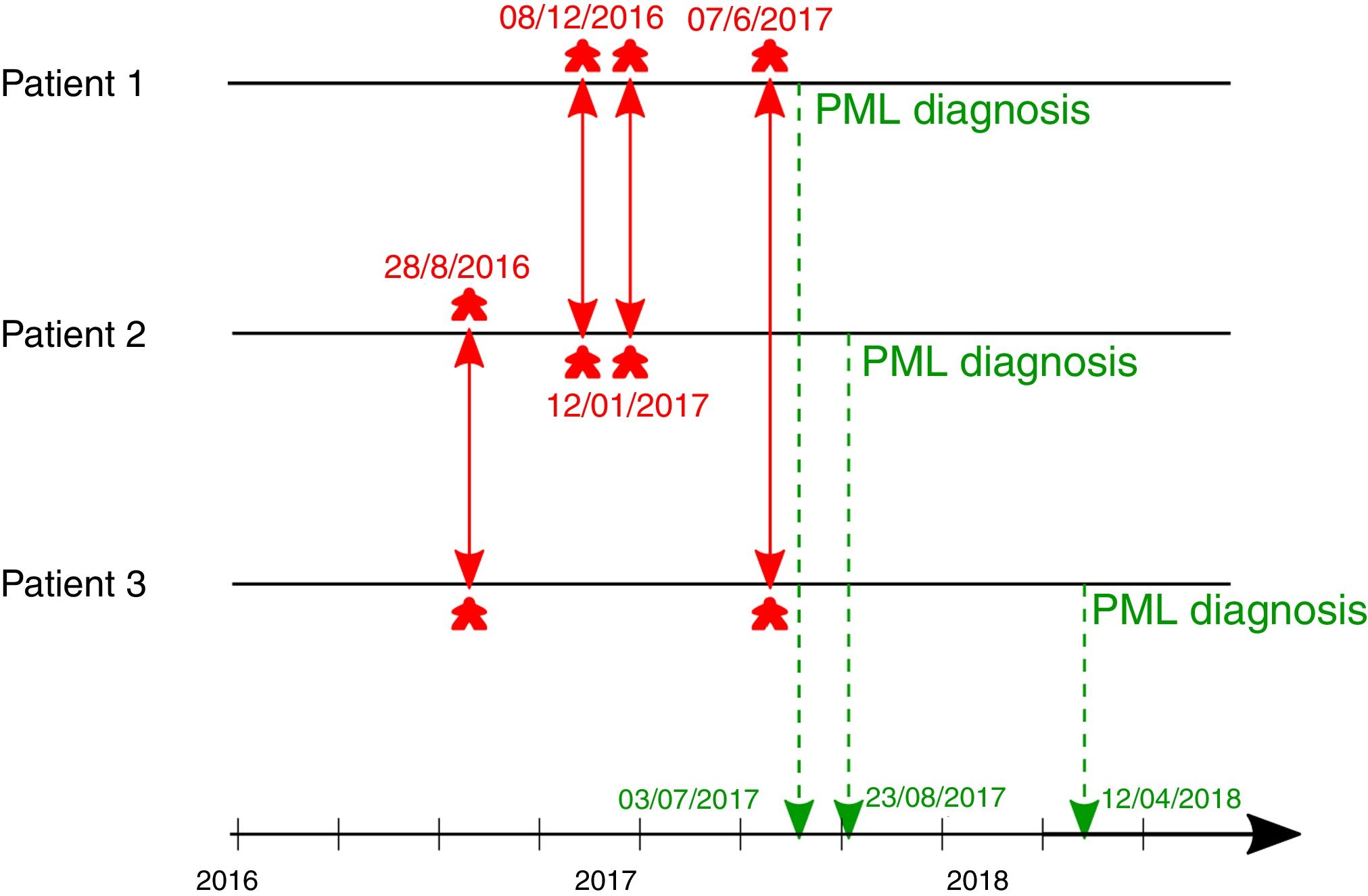
The diagnosis of three cases of PML within a short period, led us to analyze the incidence of PML in solid organ transplant recipients in our center. Between January 2007 and June 2017, as well as between May 2018 and May 2020 (i.e. a total of 150 months) no case of PML occurred in our center, while three cases were diagnosed in less than nine months, between July 2017 to April 2018. This prompted us to investigate a potential close contact between these patients and a possible nosocomial transmission. Indeed, as presented in Fig. 1, we found that the three patients attended the clinic at the same time at least once within the few months before diagnosis, i.e. two times for patients 1 and 2, once for patients 1 and 3, and once for patients 2 and 3.
JCV could be detected in several biological fluids, such as saliva, oropharyngeal fluids, blood or urine. Although the mode of transmission is not well known, initial infection by JCV is considered to be caused by ingestion or inhalation of virion particles leading to subacute infections, mainly during the childhood.5 Unfortunately, we were not able to perform the sequencing of JCV that caused PML in our patients to confirm viral transmission. Nevertheless, the diagnosis of three cases within a short period of time among patients who attended the clinic at the same time, is suggestive of a patient-to-patient transmission.
Hence, our data suggest that patient to patient transmission could occur in a transplant-unit, even if we cannot exclude another source of transmission. We suggest isolation and barrier measures for patients with suspected or confirmed PML.
Conflicts of interestThe authors declare no conflicts of interest.