Coronaviruses are known to be responsible for infections in humans since the 1960s and have accounted for epidemics in recent human history. More recently, in 2019, a disease caused by a new coronavirus appeared in China, in the province of Wuhan, with a characteristic of greater infectivity, called COVID-19, which has caused a new world pandemic. Considering the need to contain the advance in the number of cases, based on the high rate of transmissibility, several countries have adopted extreme social distancing measures, including the so-called ‘lockdown’. Despite the socioeconomic side effects, the aforementioned measure reduced the progression of the pandemic in countries that adopted it. In Brazil, the state of Ceará was one of the first epicenters of the disease in the country and the state capital city of Fortaleza, on May 8, implemented the lockdown measure to contain the increase in the number of cases. It was then observed, in a tertiary hospital, which is a referral for COVID-19 cases, a decrease in the daily occupancy rate of beds reserved for the pandemic after the lockdown onset, evidencing that this measure leads to a sustainable reduction in bed occupation rates, thus preventing the collapse and overload in health services.
Coronaviruses are known to be responsible for infections in humans since the 1960s, and new groups of viruses causing epidemics have been identified in recent human history, such as the one that occurred in the beginning of the 21st century in China, causing acute respiratory distress syndrome (ARDS), and in the Middle East, causing the Middle East Respiratory Syndrome (MERS), creating great concern since then, due to the high potential for dissemination to other countries.1
More recently, in December 2019, a new group of coronaviruses called the Coronavirus Disease 2019, or COVID-19, appeared in the province of Wuhan2, China, having a characteristic of greater infectivity. It caused a great epidemic in this Asian country, which soon spread to Europe and then to the Americas, reaching mainly the United States and Brazil in the beginning of April 2020, characterizing a pandemic of great concern for public health worldwide.3
The consequences of a city being unsuspectingly affected by a disease such as COVID-19 is well known. An unpredictable number of cases and the overload of health systems is observed. However, the city of Wuhan and China, despite the initial delay in establishing infection containment measures, also relentlessly achieved impressive results in controlling the pandemic, by implementing extreme measures of social distancing, including the so-called lockdown.4
Based on the Chinese experience, several countries have adopted the extreme social distancing strategy in an attempt to contain the advance of the pandemic. Countries such as Italy, Germany, India, the United States, and Brazil have adopted measures throughout their national territories, or regionalized the strategy, such as in Brazil. There are several opinions against the lockdown, mainly related to the political-economic scenario, as it negatively impacts economy.5,6
An infected person (even an asymptomatic one) can transmit the virus to at least 400 patients over a period of 30 days. This fast, host-to-host transmission supports the theory that strict social distancing measures implemented during the minimum period of viral incubation, allows the reduction of new infection cases. India is an example of that, having achieved a 50% reduction in the case duplication rate from 3 to 6.2 days in one week, justifying the effectiveness of the lockdown. Many districts in India achieved a zero number of cases after implementation of the measure, claiming that the lockdown would be the only effective measure to halt the number of cases at the peak of the pandemic.7
One of the beneficial effects of significantly reducing the number of cases, especially in the beginning of the epidemic, is the possibility for health services to prepare themselves structurally to receive this new demand. Patients with COVID-19 require specific resources, specially patients with severe disease who require admission at intensive care units (ICUs) and the need mechanical ventilation.
COVID-19 was first detected in Latin America on February 25th 2020, in Brazil, when the first case of the disease was confirmed in a returning traveler from Italy who lived in São Paulo. During the current pandemic, Ceará, northeast Brazil, is one of the three states with the highest number of cases.
The Brazilian scenario in relation to the number of beds and mechanical ventilation support during the pandemic has been of concern as COVID-19 is a disease with a potentially fatal evolution. Therefore, the need for intensive support and invasive ventilation increases the need for hospital beds, in both public and private hospitals, which are traditionally collapsed. In the initial period of the pandemic (January 2020), Brazil had 29,891 ICUs, with 14,094 ICUs directly linked to public system (SUS) and 15,797 with private links, with rates of ICU beds of 13.6 beds/100,000 inhabitants in the public network and 62.6 beds/100,000 in the private network. Out of the 450 Health Regions, 126 did not have an ICU, either from the SUS or from the private sector, with 44.4% of these regions located in the Northeast Region. Regarding mechanical ventilation, SUS claimed to have 40,508 mechanical ventilators, however reliable data on the real supply are scarce due to lack of adequate registration of health equipment in the databases. In studies of situational analysis carried out taking into account the various scenarios of the pandemic, including the most pessimistic scenario (infection rate of 1 per 100,000 inhabitants), practically the entire system would collapse, with 97% of the macro-regions showing impairment of their capacity. In 51 macro-regions, the health system would not be able to serve more than 50% of patients. The Northeast (64%) and the North (57%) regions of the country would present the highest proportion of macro-regions in this most critical situation. However, local public policies, through projection studies, promoted the acquisition of mechanical ventilators to supply the growing demand underway during the pandemic, including expansion of ICU beds and mechanical ventilation equipment both in the capital and in the countryside.
The government of the State of Ceará, through a state decree effective as of 03.20.2020,7 determined initial measures that restricted people’s circulation, aiming to contain the spread of COVID-19, which, at that time, had 20 notified cases. On 05.05.2020, Ceará already had 11,381 confirmed cases of COVID-19 and on May 8, 2020, the lockdown was implemented in the city of Fortaleza, the epicenter of cases in the state, as the most extreme measure of social distancing.8,9
Doubts about the real need for social distance measures still guide discussions in political and scientific areas in the country. In Brazil, while the State of Ceará, including the city of Fortaleza, took early objective distance measures (when there was still a small number of confirmed cases), other cities adopted more malleable restrictive measures, for example, the city of Sao Paulo adopted “car rotation” system from the date of May 11, 2020 when it already had 28,089 confirmed cases and 2302 deaths. Likewise, different countries have adopted different distance measures in each territory. However, in general, Latin American countries have tended to implement early restriction measures, including complete border closure, restricted daytime movements, night curfews and interruption of intercity trips, in addition to the suspension of commercial activities, as a way to follow the Chinese experience. Nonetheless, questions about acceptance by the population, mainly due to political distrust on government officials and managers, may justify different rates of population movement restriction, a fact prevalent in Brazil, due to its large territorial extension and political conflicts.
An ecological study was carried out using data from the Hospital Management Statistics Sector of the crisis office directed to the COVID-19 pandemics. Data were analyzed in one of the four largest hospitals in the city of Fortaleza, northeast Brazil, a reference center for care of COVID-19 patients. The “Hospital do Coração de Messejana” is the reference hospital of the State of Ceará for heart and lung diseases, and during the pandemic it had 266 beds for patients with COVID-19. The present study analyzed the occupancy rate based on beds intended solely for the care of patients with COVID-19 (positive RT-PCR or serological positive tests) during the period between 1st May and 31st May 2020. A linearity trend analysis was performed by calculating R2 using the software Numbers (Apple Inc., USA).
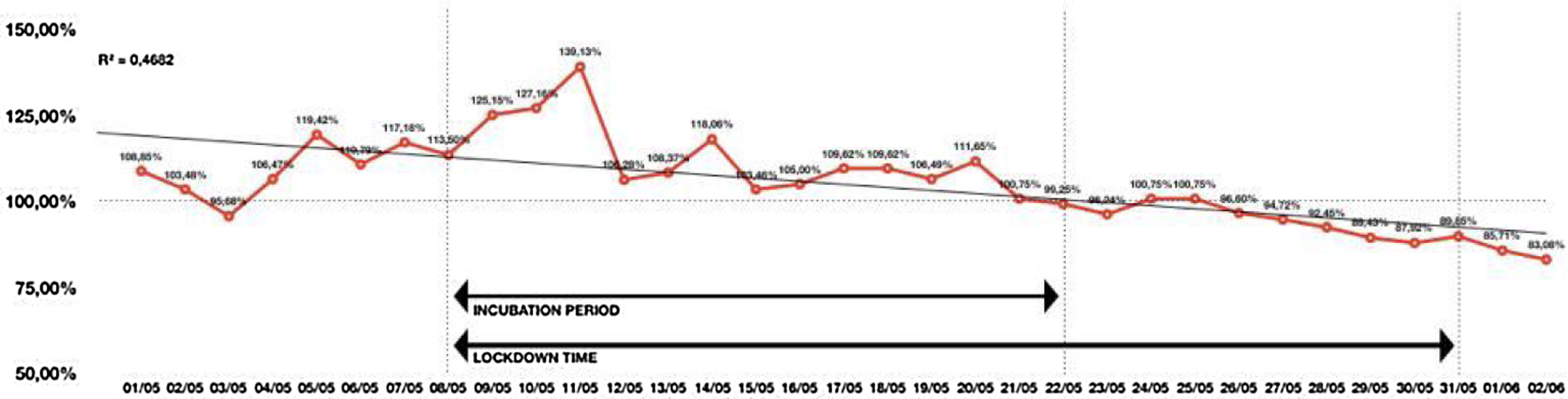
After May 8th, taking into account the 14 days of incubation of the new coronavirus, there was a slow but gradual decrease in the bed occupancy rate observed by the managerial monitoring of beds for patients with COVID-19 (Fig. 1). In the beginning of the month, bed occupancy rates were higher than 100%, reaching an extreme occupancy rate of almost 140% by May 10th (patients occupied spaces in extra beds). The opening of new beds (on May 3rd, a new clinical unit was opened with 24 beds and 33 beds was opened in the Field Hospital between May 11th and 12th) led to a particular improvement in the transitory occupancy rate, albeit still above the total installed capacity (overload). It should be observed that 14 days after the lockdown (viral incubation period), the hospital bed occupancy rate decreases to rates below 100%, a sustainable situation, resulting in available beds and 23 days after the lockdown onset, the occupancy rates were close to 85%, within expected levels as the goal of good bed management.10
Bed Occupancy rate for patients with COVID-19 in a referral tertiary hospital during the pandemic in Fortaleza, Ceará, Brazil.
Source: Hospital de Messejana, Fortaleza, Ceará, Brazil.
*100% means the total hospital capacity (beds), which was increased due to COVID-19 pandemics; it reached a peak of 130% on 11th May, and a tendency to decrease was detected after the lockdown period, mainly from 21st May on, when the bed occupancy is near 100% of the hospital capacity.
During the studied period, the state of Ceara government implemented public policies regarding therapy and patient management. It was advocated that this combination of non-pharmacological measures (lockdown) together with population-based therapeutic measures (use of medications and guidelines for seeking hospital services in case of symptoms) could control the further advancement of the epidemic. During the months of April and May, most of the technical norms standardizing the use of the main medications for patient management (hydroxychloroquine/chloroquine, azithromycin, corticosteroids and anticoagulants) and supports (mechanical ventilation protocols) had already been released, these being the basis of the guidelines followed by the clinical staff of this hospital as it belongs to the state public network.
The onset and duration of social distancing measures will influence its impact. It is a great challenge to determine the best time to implement such interventions, since their early implementation can result in economic and social difficulties with no benefit to public health and, over time, result in “intervention fatigue” and loss of adherence by part of the population. On the other hand, implementation after extensive spread of the disease may limit the public health benefits. It must occur early enough to prevent the initial steep rise in the number of cases and last long enough to cover the peak of the predicted epidemic curve.11
Currently, the city of Fortaleza has a tendency to stabilize the number of deaths, consolidated in the second week of June (25th Epidemiological week), reflecting a reduction in the fatal events recorded daily. The epidemic curve of confirmed (accumulated) cases shows a sublinear growth, with a daily increase in a slower pace. The “flattening” trend of the confirmed case curve was consolidated and monitored daily. Fortaleza is in the current phase of allowing population circulation and economic re-opening. However, the cities of the state countryside are at the peak of the epidemic, where the same measures of social distance implemented in the capital city are now adopted. The second “wave”, predicted after this re-opening of social movement in the capital, is being speculated, although unknown factors at the moment (collective immunization at high rates, previous crossed immunity, early pharmacological interventions, educational attitude related to protective measures – use of face masks, voluntary distancing) may justify, up to the present moment, the non-occurrence of an exaggerated and collapsing demand from the health units, keeping the bed occupancy rate reduced.
The use of lockdown within the context of a new pandemic becomes a challenge from the point of view of public health management. It will be necessary to record and study the experiences regarding the use of this strategy in the different scenarios, time of use, time of onset and end of the measure in comparison to the case curves, so that at the end of this pandemic we can have better knowledge and applicability of this non-pharmacological tool to fight the progression of transmissibility of diseases with the characteristics of COVID-19.
LimitationsWe recognize that this study has important limitations, since it is based on a single center in Brazil and it represents a limited period of time. However, since we face an emergency situation of pandemics, including the fact that Brazil is currently the second country in the world with the highest number of cases, we believe it is important to present these results, as they represent a significant evidence of the lockdown effect on reducing hospital beds requirement. The analyzed hospital is the main specialized hospital in heart and lung diseases of Fortaleza city, State of Ceará, which is the third epicenter of the epidemics in Brazil (first and second are São Paulo and Rio de Janeiro), and it might reflect what occur in other reference hospitals in our region after adoption of lockdown measures. Since many people, including some authorities and opinion leaders, question whether it is worth adopting lockdown, it is important to present its effects on healthcare, once the main reason for adopting such an extreme measure is to decrease the requirements for healthcare support, mainly hospital beds. This is a model of analysis of hospital beds occupancy, and by analyzing its number before and after the adopted measures is a simple way of measuring its effects. Further studies are required to analyze the broader impact of the COVID-19 pandemics on healthcare systems.
Conflict of interestThe author declares no conflicts of interest.
We would like to thank for all the health care team from the Hospital de Messejana for the exceptional assistance provided for the patients and for all the technical support provided for this study. Our study group have financial support from the Brazilian Research Council - CNPq (grant number 301174/2017-2), Fundação Cearense de Apoio ao Desenvolvimento Científico e Tecnológico - FUNCAP, and Fundação Edson Queiroz/Universidade de Fortaleza.