Hepatitis B virus (HBV) infection is an important worldwide public health problem. In Brazil, the Ministry of Health estimates that 15% of the population has had contact with HBV, and that the mean rate of chronic carriers in Northeastern Brazil is around 0.5%.
ObjectiveThe aim of this study was to assess the prevalence of HBV markers in pregnant women receiving prenatal care at the public maternity hospitals of São Luís.
MethodsDemographical and epidemiological data were collected from 541 pregnant women according to the research protocol. Blood samples were collected, and the anti-HBc test was performed first. If positive, the sample was subsequently tested for HBsAg and anti-HBs. All HBsAg and/or anti-HBc positive samples were additionally tested for HBV-DNA.
Results40 (7.4%) pregnant women turned out positive for anti-HBc. Of those, five (0.9%) were HBsAg positive, four (0.7%) were anti-HBc positive with negative HBsAg and anti-HBs, and 31 (5.7%) were positive for anti-HBc and anti-HBs. Anti-HBc positivity was associated with family history of hepatitis and education level below 11 years of schooling. HBV-DNA was positive in only one HBsAg-positive sample. There was no HBV-DNA positivity among HBsAg negative samples.
ConclusionsThe prevalence of HBsAg in pregnant women in this study confirmed that São Luís is a low endemicity area. Occult hepatitis B was not detected in these samples.
The hepatitis B virus (HBV) is the most common cause of chronic infection worldwide, and can lead to liver cirrhosis and hepatocellular carcinoma (HCC).1 The prevalence of this infection varies widely in different parts of the world, with areas of high (more than 8%), medium (between 8% and 2%), and low endemicity (less than 2%).2 In Brazil, prevalence rates are heterogeneous; the Amazon region and part of some states of South and Southeast Brazil are considered areas of high and medium endemicity, respectively.3
The Brazilian Ministry of Health estimates that 15% of the country population has been exposed to HBV, and that the average rate of chronic carriers in the capital cities of Northeast Brazil is approximately 0.5%, according to a national survey.4 HBV is transmitted by perinatal, parenteral, and sexual exposures.5,6 Perinatal transmission is of great importance in the epidemiology of the disease, since only 5% to 10% of those who acquire the infection in adulthood progress to chronicity. In contrast, children born to HBV infected mothers have a risk of chronicity of up to 90%.1,7
Cross-sectional studies have been performed in order to estimate the prevalence of this chronic infection among pregnant women in Brazil.8–12 Depending on the region studied, results have varied from 0.5% to 8.7%.
Although chronic HBV infection is defined as the presence of HBV surface antigen (HBsAg) for more than six months,1 recently a form of chronic infection has been described in which the HBV-DNA is detected in the serum or liver tissue of patients with negative HBsAg, which is known as occult hepatitis B.13,14 Populations from high endemicity regions appear to have higher prevalence of occult HBV infection; however, it has also been detected in specific populations of Brazil.15,16
In pregnant women, there is little information about occult HBV infection,17,18 and it is still not well established whether prophylactic actions are needed to prevent infection in newborn children.
There are no data about the prevalence of hepatitis B among pregnant women in the state of Maranhão; also, there have been no studies on occult hepatitis B in pregnant women in any state of Brazil. Thus, this study aimed to estimate the prevalence of hepatitis B infection markers among pregnant women assisted at the public hospitals of São Luís, the capital city of Maranhão state, including investigation of HBV occult infection.
Material and methodsThe sample size (n=500) was calculated on the basis of the total number of first visits during antenatal care in four public maternity hospitals of São Luís in 2007, which was 17,296, and the estimated HBsAg prevalence of 0.5% in the general population of Northeast Brazil.4 An absolute precision of 0.05 and a confidence level of 95% were also considered.
Data, as well as by blood collection Data from consecutive pregnant women receiving antenatal care in the selected maternity hospitals, between January and July 2009, were collected by completing a research form (including age, marital status, education level, and risk factors). Additionally, blood was taken for molecular and serological tests.
Serologic tests were performed with the LIAISON kit (DiaSorin), using the chemiluminescence technique and following the procedures established by the manufacturer. First, serologic tests for total anti-HBc (marker of contact with HBV) were performed. If it turned out positive HBsAg and anti-HBs were subsequently performed. Positive HBsAg individuals were retested six months later.
All positive total anti-HBc and negative HBsAg sera, irrespective of the presence of anti-HBs, were tested for HBV-DNA by polymerase chain reaction (PCR). Extraction of viral DNA was performed using the QIAamp DNA Kit Qiagen (Germany), according to the manufacturer's instructions. The S gene region of HBV was amplified with previously described primers.19
Chronic HBV carriers were defined as pregnant women with positive total anti-HBc and HBsAg, longer than six months. Those with positive total anti-HBc and anti-HBs were considered as immune to HBV infection, and those with positive anti-HBc, negative HBsAg and positive HBV-DNA were considered as occult HBV infection carriers.
Numeric variables were presented as means and standard deviations, and the categorical variables as n and percentage (%), with 95% confidence intervals. Differences between numerical variables were tested by Student's t-test, and between categorical variables by the Chi-squared test. p-values<0.05 were considered statistically significant.
The study was performed according to ethical guidelines and was approved by the Ethics Committee in Research of the University Hospital of the Universidade Federal do Maranhão. Only pregnant women who signed the informed consent were included in this study.
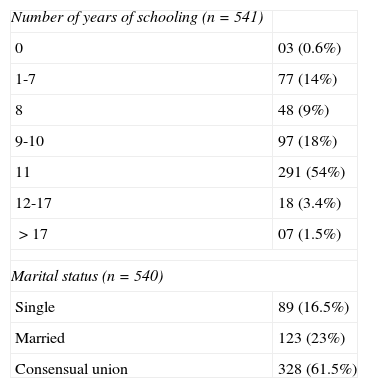
Results541 pregnant women participated in this study. The mean age was 24±5 years. Three hundred and sixteen (59%) reported having 11 or more years of schooling. 327 (61%) lived in a consensual union (Table 1).
Marital status and years of education of study pregnant women assisted in public maternities – São Luís, MA, Brazil, 2009.
| Number of years of schooling (n=541) | |
| 0 | 03 (0.6%) |
| 1-7 | 77 (14%) |
| 8 | 48 (9%) |
| 9-10 | 97 (18%) |
| 11 | 291 (54%) |
| 12-17 | 18 (3.4%) |
| >17 | 07 (1.5%) |
| Marital status (n=540) | |
| Single | 89 (16.5%) |
| Married | 123 (23%) |
| Consensual union | 328 (61.5%) |
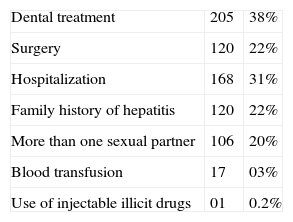
Concerning exposure to potential risk factors for HBV infection, 168 (31%) had been hospitalized at some time during their lives, 17 (3%) had received blood transfusions, 120 (22%) had undergone surgical procedures, and 205 (38%) had had some type of dental treatment. 120 (22%) reported to have a family history of hepatitis. 106 (20%) had had more than two sexual partners. Only one individual reported using injectable illicit drugs (Table 2).
Exposure to potential risk factors for hepatitis B infection, in pregnant women assisted in public maternities – São Luís, MA, Brazil, 2009.
| Dental treatment | 205 | 38% |
| Surgery | 120 | 22% |
| Hospitalization | 168 | 31% |
| Family history of hepatitis | 120 | 22% |
| More than one sexual partner | 106 | 20% |
| Blood transfusion | 17 | 03% |
| Use of injectable illicit drugs | 01 | 0.2% |
40 patients (7.4%, 95% CI, 5.4% to 10%) were positive for anti-HBc total. Five (0.92%, 95% CI, 0.3% to 2.3%) were chronic carriers of the infection (HBsAg positive longer than six months), 31 (5.7%, 95% CI, 4.2% to 8.2%) were immune to HBV infection (positive anti-HBs), and four (0.8%, 95% CI, 0.2% to 2.1%) had isolated total anti-HBc positive.
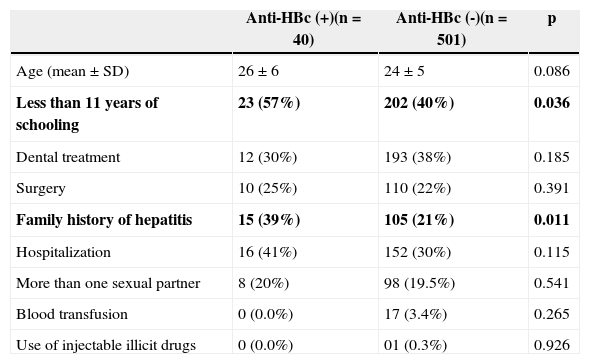
Comparing the differences between the characteristics of groups with positive or negative anti-HBc it was observed that only the level of education and the presence of family history of hepatitis were statistically associated with the presence of a positive marker (Table 3).
Comparison between pregnant women with and without positive serological markers of hepatitis B in public maternities of São Luís, MA, Brazil, 2009.
| Anti-HBc (+)(n=40) | Anti-HBc (-)(n=501) | p | |
|---|---|---|---|
| Age (mean±SD) | 26±6 | 24±5 | 0.086 |
| Less than 11 years of schooling | 23 (57%) | 202 (40%) | 0.036 |
| Dental treatment | 12 (30%) | 193 (38%) | 0.185 |
| Surgery | 10 (25%) | 110 (22%) | 0.391 |
| Family history of hepatitis | 15 (39%) | 105 (21%) | 0.011 |
| Hospitalization | 16 (41%) | 152 (30%) | 0.115 |
| More than one sexual partner | 8 (20%) | 98 (19.5%) | 0.541 |
| Blood transfusion | 0 (0.0%) | 17 (3.4%) | 0.265 |
| Use of injectable illicit drugs | 0 (0.0%) | 01 (0.3%) | 0.926 |
Despite the presence of anti-HBs marker, all anti-HBc positive and HBsAg negative samples (n=35) tested for HBV-DNA were negative. Thus, occult hepatitis B infection was not observed.
DiscussionHepatitis B is a disease of significant public health impact. Prevention strategies are important for the effective control of this infection, including universal vaccination and the use of immunoglobulin in certain situations. For this purpose, data about prevalence rates are needed, especially in populations at risk for disease transmission, such as pregnant women.
No studies in the state of Maranhão on the prevalence of serological markers of HBV in any population could be retrieved. In this representative sample of pregnant women attending public services of São Luís, five patients had the marker of current HBV infection (HBsAg) and thus, a prevalence rate of 0.94% (95% CI, 0.3% to 2.3%), which is not different from most of the results found in studies conducted in other Brazilian states (ranging from 0.5% to 1.7%),8–11 and far below the prevalence found in a study in the state of Amazonas, which was as high as 8.7%.12 The prevalence found in the present study confirms the expectation that the state of Maranhão is a region of low HBV endemicity.
When comparing the characteristics of the groups with and without positive markers for HBV, it was observed that only family history of hepatitis and low level of education were positively associated. Family history could be explained by the possibility that some patients have family members with HBV infection, who could have transmitted the disease to them and then cleared the virus (remaining the markers of contact). Such occurrence is frequent after five years of age, which is already clearly shown in some regions of the world, including Brazil.20 Another explanation could be the possibility of episodes of acute infection in sexual partners, who may have transmitted the disease, with subsequent progression to cure. The level of education, probably a surrogate of low socioeconomic status, reflects poor knowledge about prevention as well as poor access to health services, which lead to greater susceptibility to infection.
Cases of occult hepatitis B among HBsAg negative and anti-HBc positive individuals were not identified, even among those who had isolated anti-HBc, without anti-HBs marker. This result was consistent with the expectation that this event is uncommon in areas of low endemicity, although this has already been described in the general population in Brazil.15
This study demonstrated the low prevalence of chronic HBV infection in pregnant women assisted in public maternity hospitals of São Luís. The presence of serological markers for HBV infection was associated with lower educational levels and family history of hepatitis. These results confirm that investments in education are important for the prevention of most diseases. The absence of cases of occult HBV is consistent with the area of low HBV prevalence expected for São Luis.
Conflict of interestAll authors declare to have no conflict of interest.
We thank the National Council of Technological and Scientific Development (CNPq) for the financial support. We also thank Prof. Dr. Natalino Salgado Filho and Bezelga Ana Luiza Rodrigues for their indispensable contributions to the implementation of this study. They also thank the professionals of all hospitals in which data collection was performed for having promptly and openly received the researchers.