In December 2019, the outbreak of coronavirus disease 2019 (COVID-19) infection, which is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus, was reported in Wuhan, China.1 During COVID-19 pandemic, the type of patients receiving treatment in a head and neck surgery unit differs from it before the pandemic.2 While patients with cleft lip and plate, chronic sinusitis, benign tumors, and so on are recommended to defer the operation, emergent patients with mandibular fracture, malignant tumors, and severe acute infectious diseases such as peritonsillar abscess, acute supraglottitis, and acute deep neck infection must receive emergent conservative or surgical management even during COVID-19 pandemic. By March 18, 2020, we managed emergent patients using the algorithm for the outbreaks as indicated by Yang et al.2 Namely, according to the algorithm, when clinical symptoms or chest computed tomography (CT) as risk assessment is normal, they receive routine treatment, and if clinical manifestations continue to be suspected of COVID-19, they are transferred to designated hospital for infectious diseases in order to receive both reverse transcription-polymerase chain reaction test to detect SARS-CoV-2 infection (the SARS-CoV-2 RT-PCR test) and further management. When clinical symptoms or chest CT is suspected of COVID-19, they are directly transferred to designated hospital. However, even when we follow the above algorithm, we might experience nosocomial infection caused by COVID-19 as indicated by Yang et al.2 Therefore, we needed to re-consider management of emergent patients during COVID-19 pandemic.
Problems for the management of the patients according to the above algorithm by Yang et al. were as follows. At first, we may misdiagnose asymptomatic patients with COVID-19 or patients with COVID-19 whose chest CT is normal. In addition, because of the similarities of clinical symptoms between severe acute infectious diseases with the possibility of upper airway obstruction and COVID-19 regarding fever and dyspnea, it is hard to differentiate whether the patient suffered from only severe acute infectious disease or both severe acute infectious disease and COVID-19 on admission. Thus, we cannot use the algorithm which recommends the SARS-CoV-2 RT-PCR test only for suspected COVID-19 patients on the basis of clinical manifestations of COVID-19 and epidemiological history for patients with severe acute infectious disease, as indicated by Lu et al.3 On the other hand, we can follow the algorithm as indicated by Lu et al. for patients with non-infectious diseases such as mandibular fracture and malignant tumors. Third, some emergent patients must receive emergent operation without knowing the status of SARS-CoV-2 infection. Therefore, head and neck surgeons must perform the emergent operation wearing high level of personal protective equipment (PPE) in a negative pressure operation room. Moreover, health care workers (HCWs) must manage the patients with unknown status of SARS-CoV-2 infection wearing high level of PPE in the isolation ward after emergent operation, while the shortage of PPE is remarkable around the world.4 Fourth, it is unclear whether patients with unknown status of COVID-19 with severe acute infectious disease also complicated with upper airway stenosis owing to laryngeal edema can be given systematic steroid, because they might be immunocompromised when they are given systematic steroid.
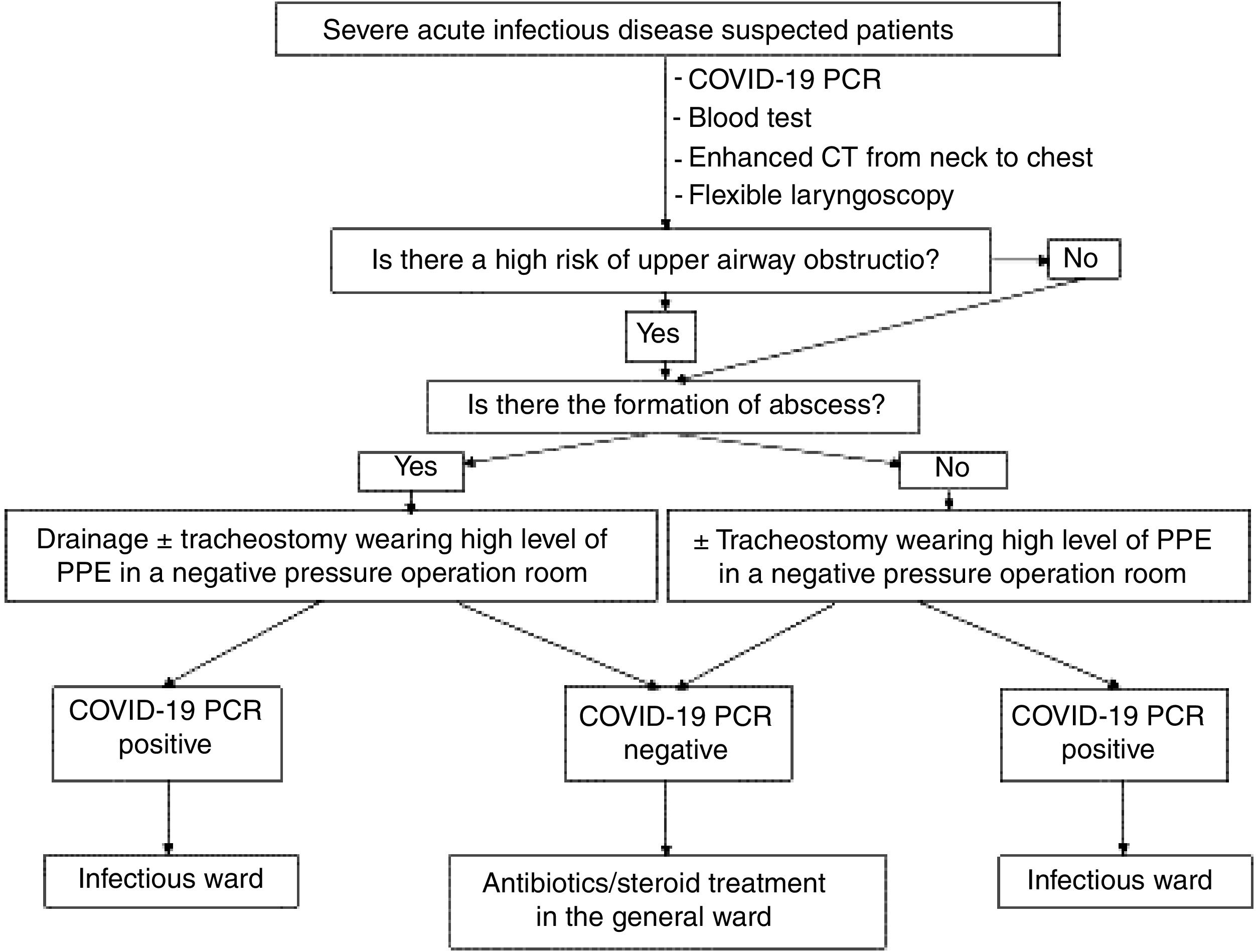
In order to overcome the above problems, we manage the patients with emergent infectious diseases using new algorithm since March 19, 2020 as indicated in Fig. 1. Namely, on emergent admission, patients suspected of severe acute infectious disease perform SARS-CoV-2 RT-PCR test in addition to routine blood test, enhanced CT from neck to chest, and flexible laryngoscopy. Using this strategy, there is less possibility that the patients with severe acute infectious disease might also involve patients with SARS-CoV-2 infection. Patients with severe acute infectious disease and COVID-19 whose chest CT is normal can be differentiated from emergent patients suffering from severe acute infectious disease other than COVID-19. Furthermore, shortage of PPE may be overcome to a certain degree. In the SARS-CoV-2 RT-PCR negative case, HCWs do not need to wear high level of PPE after RT-PCR result. Furthermore, COVID-19 negative patients also with laryngeal edema can be given systemic steroid.
In conclusion, we insist that RT-PCR test for SARS-CoV-2 on admission is essential for emergent patients with severe acute infectious disease in order to prevent nosocomial infection and collapse of the medical care system during COVID-19 pandemic. Different management between emergent infectious disease and emergent non-infectious disease is important while the SARS-CoV-2 RT-PCR test does not become widely available. Up to June 29, 2020, no nosocomial infection had occurred at our hospital under this management. Thus, we are convinced that our algorithm will be useful for the prevention of nosocomial infection also in Brazil which is one of the most seriously affected countries by COVID-19 in the world.5 Of course, ideally all patients admitted to hospital should have a SARS-CoV-2 RT-PCR test performed to prevent overlooking asymptomatic patients with COVID-19 as it becomes more widely available.
Conflict of interestThe authors declare no conflicts of interest.