Lamivudine (LAM), a nucleoside analog, was the first anti-HBV drug approved for antiviral therapy in China. Long-term antiviral therapy with LAM may lead to drug resistance, which is associated with a mutation in tyrosine-methionine-aspartic acid-aspartic acid (YMDD) motif of the reverse transcriptase in HBV-DNA genome. Several previous studies showed that YMDD mutations were also present in treatment-naive chronic hepatitis B (CHB) patients, but the prevalence rates of natural YMDD motif mutations in some reports were quite different (from 0% to 26.9%).1–4 However, the relationship between natural YMDD motif mutations and virus-related characteristics in CHB patients is also not quite clear. The aim of present study was to assess the prevalence rate of natural YMDD motif mutations and to investigate the associations between natural YMDD mutations and clinical factors among LAM-untreated CHB patients in Huzhou city, eastern China.
A total of 202 CHB patients who had never received antiviral treatment were recruited from department of infectious diseases in Huzhou central hospital for this study. CHB was diagnosed according to the Chinese consensus criteria. This study was approved by the Ethics Committee of Huzhou central hospital. All patients provided written informed consent. Serum HBV DNA levels were quantified using a real-time PCR kit. HBV genotypes were analyzed by genotype-specific Taqman probes using a real-time fluorescence PCR. YMDD mutations were detected using specific primers for real-time PCR.
Natural YMDD mutations were found in 20 (9.9%) treatment naive CHB patients. Among these patients, YVDD variants were detected in 13 cases, YIDD variants in 5 cases, and YVDD+YIDD variants in 2 cases. In this study, the rate of natural YMDD motif mutation was not consistent with previous studies.1–4 The reason for the discrepancy might be due to different demographic characteristics, geographical diversion, other characteristics of study groups, and sample sizes, as well as sensitivity of different detection methods.2–4
The mean age of patients were 37.8±10.8 and 36.7±13.2 years for patients with and without natural YMDD motif, respectively (p>0.05); 70% of patients with natural YMDD motif were male compared to 68.7% of patients without natural YMDD motif (p>0.05). Some previous studies showed that natural YMDD motif mutation was not associated with age and gender of patients,3–5 which is consistent with the results of this study.
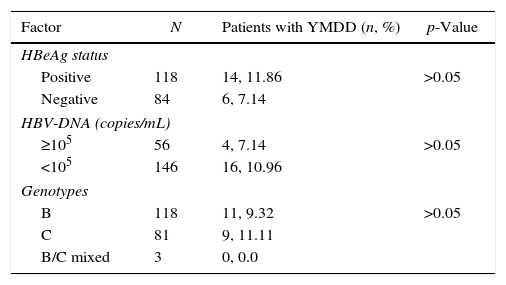
In present study, the prevalence rate of natural YMDD mutations among HBeAg positive and HBeAg negative patients were not significantly different (p>0.05) (Table 1). This finding is contrast with some previous reports,3,4 but in line with other reports.2 The relationship between the HBV genotype and natural YMDD mutations is not clearly identified. Some previous researchers reported that most natural YMDD motif mutations occurred in patients infected with genotype C and its mixed forms.2,4 In contrast, our results showed no association between natural YMDD motif mutations and HBV genotype (p>0.05) (Table 1).
Relationship between natural YMDD motif mutation and clinical feature.
| Factor | N | Patients with YMDD (n, %) | p-Value |
|---|---|---|---|
| HBeAg status | |||
| Positive | 118 | 14, 11.86 | >0.05 |
| Negative | 84 | 6, 7.14 | |
| HBV-DNA (copies/mL) | |||
| ≥105 | 56 | 4, 7.14 | >0.05 |
| <105 | 146 | 16, 10.96 | |
| Genotypes | |||
| B | 118 | 11, 9.32 | >0.05 |
| C | 81 | 9, 11.11 | |
| B/C mixed | 3 | 0, 0.0 | |
In addition, the prevalence rate of YMDD in patients with high HBV-DNA level (≥105copies/mL) was higher than those with low HBV-DNA level (<105copies/mL), but the difference was not significantly different (p>0.05) (Table 1). This result is not consistent with previous studies, which suggested an association between higher HBV-DNA level and increased prevalence of natural YMDD mutations.4,5 Whether the HBV-DNA level is indeed associated with higher prevalence of YMDD mutations warrants more studies.
This study shows that the natural YMDD motif mutations do exist in a proportion of treatment-naive CHB patients in eastern China. These findings suggest that it is necessary to screen for YMDD resistance mutations before LAM therapy. Further large-scale, multi-center and follow-up studies are needed to elucidate the mechanism and clinical significance of natural YMDD motif mutations in HBV chronically infected patients.
Conflicts of interestThe authors declare no conflicts of interest.
This work was supported by a grant from the Foundation Project for Science and Technology of Huzhou City (No. 2014GY12).