Despite the known efficacy of the intrapartum antibiotic prophylaxis (IAP),1 no Group B Streptococcus (GBS) prophylaxis program are in place in Brazil,2 and rates of early-onset sepsis (EOS) may be underestimated. We conducted a retrospective analysis on the incidence EOS, IAP use and outcomes of infants born in a Brazilian University Hospital (Hospital de Clínicas de Uberlândia, HC-U). An early-onset GBS sepsis episode was defined based on positive blood cultures in the first 72h of postnatal life. Blood cultures for all newborn infants with suspected sepsis were performed by an automated system (Vitek 2 system BioMerieux, France). Maternal/infant demographic and clinical data were obtained from the medical records. The study was approved by the University Hospital Ethics Committee (protocol 394/09).
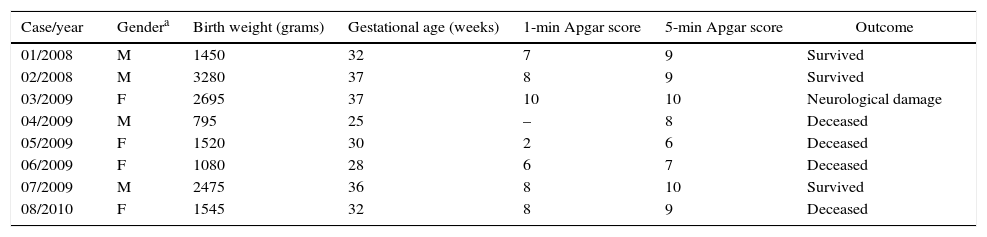
From January 2008 to December 2011, there were 8818 live births. Among them, we identified eight infants with confirmed early-onset GBS sepsis. The overall incidence rate was 0.90 cases per 1000 live births. Infants’ characteristics and clinical outcomes are shown in Table 1. All neonates were born vaginally. The average hospital length of stay was eight days (range: 1–36 days). The case-fatality rate was 50% (4/8), occurring in the first four days of life. Out of four newborns that survived, one had early-onset GBS sepsis associated with meningitis and coursed with neurological damage. We detected one GBS isolate resistant to erythromycin with a minimum inhibitory concentration of 8μg/ml.
Clinical characteristics and outcome of newborns with early-onset GBS sepsis during 2008–2011.
| Case/year | Gendera | Birth weight (grams) | Gestational age (weeks) | 1-min Apgar score | 5-min Apgar score | Outcome |
|---|---|---|---|---|---|---|
| 01/2008 | M | 1450 | 32 | 7 | 9 | Survived |
| 02/2008 | M | 3280 | 37 | 8 | 9 | Survived |
| 03/2009 | F | 2695 | 37 | 10 | 10 | Neurological damage |
| 04/2009 | M | 795 | 25 | – | 8 | Deceased |
| 05/2009 | F | 1520 | 30 | 2 | 6 | Deceased |
| 06/2009 | F | 1080 | 28 | 6 | 7 | Deceased |
| 07/2009 | M | 2475 | 36 | 8 | 10 | Survived |
| 08/2010 | F | 1545 | 32 | 8 | 9 | Deceased |
Half of the mothers were ≤16 years old and 75% were primiparous. Most (75%) had prenatal care. Leukocytosis (>15,000cells/mm3) was identified in two women. One woman had chorioaminiorrexis >24h, untreated urinary tract infection and fever before labor. Another woman had fever (38.6°C) in the first day after delivery and was also diagnosed with urinary tract infection. Although one pregnant woman had been screened for GBS during pregnancy, the positive GBS culture result was not obtained timely. The remaining seven women were not screened for GBS. Consequently, GBS colonization status of all pregnant women was unknown at delivery. None of the mothers received IAP.
Data for newborn infants cared in Brazilian's NICU show a high proportion (39.2%) of maternally acquired bloodstream infections beginning within the first 48h after birth.3 GBS is referred as the leading etiological agent of maternal acquired infections in some Brazilians NICUs.3,4 Our results reinforce these findings and emphasize the importance of early-onset GBS sepsis considering the high incidence (0.9 cases per 1000 live births) and the fatality rate (50%). Similarly, other authors have found an overall incidence rate of early-onset GBS sepsis ranging from 0.39 to 1 per 1000 live births,2,5 with meningitis being detected in a large proportion (26%) of the infected newborns5 who had a high (60%) lethality rate.2,5
We conclude that improvement of prenatal care is recommended in this population to decrease the burden of this maternally acquired infectious disease. Implementation of prophylactic measures should be considered an important public health strategy to avoid early-onset GBS sepsis. The best scenario would be universal culture-based screening of all pregnant women (35–37 weeks) to identify positive GBS women who should receive IAP.1 Furthermore, use of rapid microbiologic tests could be beneficial for intrapartum screening in preterm deliveries.
FundingThis work was supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (grant 474296/2007-5 to P.P.G.F.)
Conflicts of interestThe authors declare no conflicts of interest.
Study conducted at the Universidade Federal de Uberlândia (UFU), Minas Gerais, Brazil.