In the initial phases of the COVID-19 pandemic, strategies adopted to reduce the dissemination of SARS-CoV-2 relied on non-pharmacological interventions, including physical distancing. Mobility restrictions affected the availability and quality of care for many health conditions, including sexually transmitted infections.
ObjectiveTo investigate the impact of the COVID-19 pandemic mobility restriction on syphilis and HIV testing in outpatient settings.
MethodsIn this study, we collected the weekly number of syphilis and HIV tests performed in a referent laboratory in São Paulo, Brazil, as well as the percentage of positive tests between January 2019 and December 2021. We also retrieved data on retail and recreation mobility in São Paulo city using Google COVID-19 Community Mobility Reports. We explored the association between populational mobility and the number of weekly tests and the association between the number of weekly tests and the percentage of positive results during the pandemic period. The analyses were conducted separately for syphilis and HIV tests.
ResultsWe found that mobility restrictions during the COVID-19 pandemic have been associated with a significant decrease in both syphilis and HIV tests performed in outpatient settings. We also observed that the number of tests performed was inversely associated with the percentage of positive results for syphilis; this association was also apparent for HIV tests in the first wave of the pandemic in the graphic analysis.
ConclusionTaken together, our findings suggest an indirect impact of COVID-19 pandemic-related mobility restrictions on the uptake of diagnostic tests for HIV and syphilis and the potential adoption of targeted-testing strategies. Understanding the extent and complexity of COVID-19 aftermaths on specific conditions and communities is essential to build strategies to mitigate the long-term consequences of COVID-19.
Since February 2020, when the first patient with SARS-CoV-2 infection was identified in Brazil, until the end of 2021, more than 22 million cases have been officially reported, with approximately 619 thousand deaths in the country.1 In the city of São Paulo alone, the pandemic was responsible for a peak of 3598 hospitalizations on a single day in March 2021.2 As seen in other parts of the world, this scenario prompted a great mobilization of resources from different areas to essential services implemented to mitigate the consequences of the pandemic. In the healthcare sector, COVID-19 took precedence over almost any other condition, and not only many professionals were displaced from their usual positions, but also a significant reallocation of diagnostic, therapeutic and financial resources was implemented.3,4 Meanwhile, other health issues that commonly affect the population, such as Sexually Transmitted Infections (STI), didn't cease to exist. For instance, syphilis and HIV are persisting threats associated with 158,0005 and 40,0006 yearly new infections in Brazil, respectively. In most cases, patients with syphilis and people living with HIV manifest little or no symptoms during a considerable interval in the natural history of the disease. Therefore, diagnosis relies mostly on the uptake of screening tests.
In the initial phases of the COVID-19 pandemic, when vaccines were still under development or scarcely distributed across different parts of the world, the main strategies adopted to reduce the dissemination of SARS-CoV-2 were non-pharmacological interventions, including physical distancing. It has been reported that mobility restrictions and lockdowns affected the availability and quality of care for many health conditions.7 However, it is plausible to assume that the impact of mobility restrictions was even higher for conditions that produce few or no symptoms since these patients would be even less motivated to visit a health facility. Conversely, as healthcare workers were more focused on the identification and support for COVID-19 patients, it is also likely that provider-initiated STI testing strategies were much less often adopted, resulting in a decrease in syphilis and HIV testing even for the few patients who managed to reach a health facility during the pandemic. Some studies also suggest that, in face of limited resources, strategies for targeted testing of patients at higher risk for STI could have been adopted, resulting in a higher percentage of positive tests concurrently with reductions in the overall number of tests.8 In any case, at a population level, restrictions in the diagnosis and treatment of syphilis and HIV could result in failure to break the chains of transmission, further expanding the dissemination and complications of these infections.
In this study, we investigate the association between COVID-19 pandemic-related mobility restrictions and the number of diagnostic tests for syphilis and HIV performed in a referent health service in the city of São Paulo, Brazil. We also explored correlations between the number of weekly tests and the percentage of positive results according to the magnitude of human mobility reduction.
Material and methodsDesignRepeat cross-sectional analysis.
Data retrievalWe collected data on the weekly number of syphilis and HIV tests performed by the clinical laboratory at Hospital Israelita Albert Einstein in São Paulo, Brazil, as well as the percentage of positive tests between January 2019 and December 2021. After the exclusion of duplicates, invalid results, tests requested in the context of emergency care, and tests performed in hospitalized patients, anonymized data on the age and gender of patients were also extracted from the laboratory database. We retrieved data on retail and recreation mobility in São Paulo city using Google COVID-19 Community Mobility Reports9 between February 2020 and December 2021; this appliance presents the daily percentage of human mobility in different locations taking as the baseline reference the median value observed in the 5-week period between January 3rd to February 6th, 2020.
StatisticsWe categorized the weeks within the pandemic period into 3 subgroups according to the mean observed reduction in population mobility: weeks with less than 25% mobility reduction; weeks with 25% to 50% mobility reduction; and weeks with more than 50% mobility reduction. We used Chi-Squared tests to compare gender distributions and the percentage of positive tests, and Kruskal-Wallis tests to compare age and the number of weekly tests performed in each mobility category. We used Spearman's test and graphic analysis to investigate the correlation between populational mobility and the number of weekly tests and the correlation between the number of weekly tests and the percentage of positive results during the pandemic period. The analyses were conducted separately for syphilis and HIV tests. Finally, we plotted mobility, the weekly number of tests and the weekly percentage of positive results over time between January 2019 and December 2021 for a graphic depiction of these variables before and across the pandemic period. We used Stata 15.1 (StataCorp. College Station, TX: StataCorp LP) for all statistical analyses, with a 0.05 significance level. We used Microsoft Excel for Mac (Version 16.66.1 [22101101]) to design the plots depicting mobility, the weekly number of tests and the weekly percentage of positive results over time.
Laboratory specificationsFor HIV and syphilis immunoassay, we used the ARCHITECT i2000 SR analyzer (iDig) platform and ARCHITECT c8000 analyzer (cDig) platform, according to the protocols recommended by the manufacturer (Abbott Laboratories, Green Oaks, IL).
Study settingAlbert Einstein Hospital is a non-profit, 630-bed academic tertiary hospital, located in São Paulo, Brazil. It excels in implementing state-of-the-art medical technologies in several medical specialties and is ranked as one of the best hospitals in Latin America.
Ethical aspectsThe institutional Ethics Committee reviewed and approved this study with the exemption of informed consent. Our dataset included anonymized patient information only.
ResultsOur search strategy identified 78,552 eligible HIV tests and 41,533 eligible syphilis tests between January 2019 and December 2021. Data on age, gender, number of weekly tests, and percentage of positive results for syphilis and HIV according to the mobility category are presented in Table 1. The median age of patients contributing to the study sample was 37 years old (Interquartile Range [IQR] 45‒30), and 40% were men.
Gender, age, number of weekly tests, and percentage of positive results for syphilis and HIV according to the mobility reduction category.
IQR, Interquartile Range; CI, Confidence Interval.
Populational mobility data comprised 98 weeks between February 2020 and December 2021. Of those, 33 had a mobility reduction < 25%, 44 had a reduction between 25%‒50%, and 21 had a mobility reduction > 50%. Milder mobility reduction corresponded mostly to the second semester of 2021. Greater mobility reductions were observed in two periods: mid-March 2020 to June 2020, and March 2021 to mid-April 2021.
The weeks with > 50% mobility reduction had a lower percentage of men being tested (p < 0.001) and a somewhat younger age distribution compared to weeks with less than 50% mobility reduction. We observed a lower median number of syphilis and HIV tests per week associated with greater mobility reduction (p < 0.001). A higher percentage of positive results for syphilis was also associated with mobility reduction > 50% (p < 0.001). The percentage of positive HIV tests had no statistically significant association with any of the mobility reduction categories (p = 0.209, Table 1).
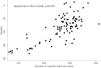
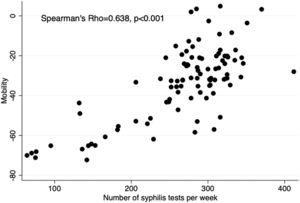
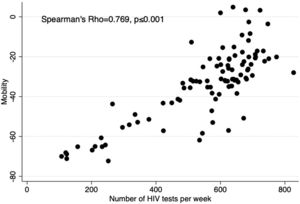
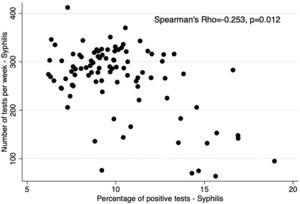
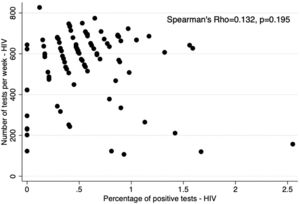
Figs. 1 and 2 present scatter plots depicting the correlation between population mobility and the number of tests. Figs. 3 and 4 present scatter plots depicting the correlation between the number of tests and the percentage of positive results. We found a statistically significant correlation between population mobility and the number of weekly syphilis tests (Spearman's Rho = 0.638, p < 0.001) and between populational mobility and the number of weekly HIV tests (Spearman's Rho = 0.769, p < 0.001). We also found an inverse correlation between the number of weekly syphilis tests and the percentage of positive results (Spearman's Rho = −0.253, p = 0.012). We failed to find a statistically significant correlation between the number of HIV tests and the percentage of positive results (Spearman's Rho = 0.132, p = 0.195).
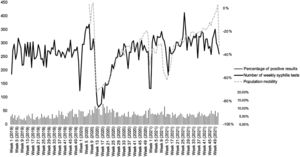
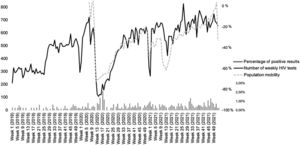
Figs. 5 and 6 present trends over time for the number of tests performed per week, population mobility, and percentage of positive results for syphilis (Fig. 5) and HIV (Fig. 6) between January 2019 and December 2021. The number of weekly tests for both infections closely follows population mobility tendencies. Three striking reductions in testing and mobility were noticeable. The first two correspond to the first and second waves of COVID-19 in the city of São Paulo.2 The third one was likely related to major end-of-year holidays and vacations. For syphilis, apart from the two periods with a significant reduction in tests, the number of tests remained similar to the pre-pandemic period. For HIV, a progressive recovery in the number of tests occurred after the first and second waves; interestingly, the overall number of weekly tests was even higher after the second wave compared to the pre-pandemic period. We observed a rise in the percentage of positive results for both syphilis and HIV during the first COVID-19 wave, suggesting that strategies of targeted testing of patients at higher risk may have been adopted.
In this repeat cross-sectional study, we showed that mobility restrictions during the COVID-19 pandemic have been associated with a significant decrease in both syphilis and HIV tests performed in outpatient settings served by our institution's clinical laboratory. We observed that the number of tests performed was inversely associated with the percentage of positive results for syphilis; we failed to find this association for HIV when comparing mobility reduction categories or in the correlation analysis, although this association was apparent in the first wave of the pandemic in the graphic analysis.
Our findings are aligned with previous studies conducted in other settings. In a study that analyzed data from four continents, despite regional differences, authors observed an overall reduction in HIV testing and a reduction in the number of new enrollments in HIV care facilities during the COVID-19 pandemic period.8 Studies from Africa and USA used predictive models to assess the impact of COVID-19 on HIV testing and concluded that, in Africa, mortality rates will increase significantly in the next 5-years, while in the USA, a 50% reduction in testing would result in a 9% increase of incident HIV cases between 2020 and 2025.10,11 Studies conducted in Belgium, Australia and Panama also showed reductions in HIV testing during the COVID-19 pandemic.12-14 Another study including data from the World Health Organization Europe region observed important reductions in tests for HIV, syphilis and other sexually transmitted infections.15 Although these studies collectively gather a large amount of data from several countries, only one included data from South America. In the course of disruptive events such as the COVID-19 pandemic, the observed impact on medical care (including access to diagnostic tests) can vary greatly in different contexts. Thus, data reflecting the reality of specific regions are important to guide tailored health policies aiming to reduce the mid and long-term detrimental effects of the COVID-19 pandemic. Our study also assessed the patterns of outpatient HIV and syphilis testing according to mobility reductions, providing important insights for the development of mitigation strategies in future events that result in reduced access to facility-based testing. Of note, resources such as telemedicine, self-collection kits, and home-based self-test devices could facilitate the uptake of diagnostic tests for sexually transmitted infections not only in settings with reduced mobility but also among hard-to-reach populations.16
The inverse association between the number of tests and the percentage of positive results, observed for syphilis in all analyses, and for HIV in the graphical analysis for the 1st COVID-19 wave, suggests that tests may have been more frequently performed for patients at higher risk for a positive result during the periods of higher mobility reduction, as suggested in a previous study.8 This targeted testing could have been observed because patients who had suggestive symptoms or those who were asymptomatic but at higher risk were more likely to seek care despite mobility restrictions. Alternatively, this could also result from provider-initiated testing prioritizing patients at higher perceived risk. While resources should be allocated to those most in need, in the case of sexually transmitted infections it is also necessary that appropriate screening tests are available to all individuals to avoid secondary transmission and other complications of untreated infections.
We also observed a small reduction in median age and a reduction in the overall percentage of male patients undertaking HIV and/or syphilis tests in periods with higher mobility restrictions. While the change in median age is unlikely to be clinically meaningful, reductions in the percentage of male patients suggest a differential impact of pandemic-related mobility restriction by gender. Gender-based differences in healthcare-seeking behaviors have been described in multiple studies, usually suggesting that men are less likely to access healthcare when compared to women;17-19 it is unknown whether this discrepancy would increase, decrease, or remain stable in the context of restricted mobility. On the other hand, the overall prevalence of HIV and syphilis in Brazil is higher among men when compared to women;5,6 consequently, targeted testing would be expected to prioritize men over women during the most critical moments of the pandemic.
Another interesting finding from our study was the pattern of weekly tests performed after periods of higher mobility restriction. For syphilis, the number of tests returned to baseline pre-pandemic patterns after May 2021. The number of HIV tests showed a different tendency, achieving even higher values than those seen in the pre-pandemic period. It is unclear if this post-pandemic increase in HIV testing represents a latent demand from patients postponing tests during the pandemic. However, since a progressive increase in the weekly number of HIV tests was already noticeable even before the pandemic, additional mechanisms likely contributed to the rising number of tests performed in our institution.
Our study had a few limitations. We used a repeat cross-sectional design to depict trends over time. Because the same patient could have been enrolled more than once in the weeks represented in the study, tests and results across the study window could be non-independent, potentially influencing the percentage of positive results; however, assuming that this would be a rare event, it is unlikely that estimates would be heavily affected. We were unable to obtain data from other laboratories that could represent the experience of other outpatient communities, including those serving as referent facilities for key vulnerable populations, such as sex clinics; or those attending patients with a presumed lower risk for sexually transmitted infections, such as antenatal care clinics. We opted for using mobility information derived from retail and recreation in Google COVID-19 Community Mobility Reports; other modalities of mobility ascertainment could also have been adopted. Finally, we used screening HIV and syphilis tests to define study endpoints, ignoring confirmatory tests.
Despite these limitations, our findings are relevant to demonstrate the indirect impact of COVID-19 pandemic-related mobility restrictions on the uptake of screening tests for HIV and syphilis. Understanding the extent and complexity of COVID-19 aftermaths on specific conditions and communities is essential to build strategies to mitigate the long-term consequences of COVID-19.
Authors' contributionsGJSM, FFE, BFP and VAS conceived the study. GJSM and VAS performed data analysis and drafted the first version of the manuscript. VAS prepared Table 1 and Figs. 1, 2, 3 and 4. GJSM prepared Figs. 5 and 6. AMD contributed with manuscript writing. GJSM, AMD and EARW contributed with data acquisition and database organization. All authors revised and approved the final version of the manuscript.
FundingGJSM is supported by a research grant from Sociedade Beneficente Israelita Brasileira Albert Einstein through the contract with the Associação Brasileira de Gestão em Projetos.
Ethics approval and consent to participateThe institutional Ethics Committee reviewed and approved this study with exemption of informed consent. Our dataset included anonymized patient information only.
Consent for publicationNot applicable.
Permission to reproduce materials from other sourcesNot applicable.
Availability of data and materialsCurrently, the datasets used and/or analyzed during in this study are restricted to institutional investigators. Data may be available through reasonable request and approval by the institutional Ethics Committee.
We thank Denise Laurentis dos Anjos de Sousa, member of the Big Data division at Hospital Israelita Albert Einstein, for supporting data acquisition.