Tropical spastic paraparesis or HTLV-associated myelopathy (TSP/HAM) may prevent, limit or restrict the performance of daily living activities, and as a consequence, several aspects of life are affected.
ObjectiveThe aim of this study was to evaluate activity limitations, risk awareness, social participation, quality of life, and pain in individuals infected with HTLV-1.
MethodsThis was an observational, descriptive, analytical, cross-sectional study with a quantitative approach. An interview questionnaire, the Screening of Activity Limitation and Safety Awareness (SALSA) scale, the Participation scale, a quality of life questionnaire (SF-36) and the Brief Pain Inventory were used.
ResultsA total of 55 patients with HTLV-1 were interviewed (62% asymptomatic and 38% symptomatic). In both groups, there was a higher frequency of patients aged 41–50 years old (35.3% asymptomatic and 38.1% symptomatic), with complete secondary education (47.1% asymptomatic and 42.9% symptomatic), and married (64.7% asymptomatic and 52.4% symptomatic). Of the symptomatic patients, 33.3% were retired; among asymptomatic patients, 20.6% performed domestic activities. The majority of patients in both groups had not received blood transfusions. Sexual intercourse was still practiced by patients. After assessment, asymptomatic patients had no activity limitations (64.7%), and symptomatic patients presented limitations (90.5%). None of the groups showed good risk awareness. There was no restriction on social participation in 97.1% of asymptomatic patients and in 52.4% among symptomatics. Both groups complained of pain, being more frequent in the lumbar spine in asymptomatic patients and in the knees in symptomatic patients. Pain was more severe in symptomatic patients and affected aspects of quality of life.
ConclusionThe clinical follow-up instruments must be adopted by healthcare professionals to monitor new symptoms so as to avoid the onset of limitations identified in symptomatic patients, in addition to enabling continuous surveillance of asymptomatic patients.
Human T-lymphotropic virus 1 (HTLV-1) was reported as the first human retrovirus after being isolated in the United States in lymphocytes from a person with T-cell lymphoma.1
It is estimated that approximately 5–10 million people worldwide have HTLV-1 infection, with varying distribution according to ethnic group, individual risk behaviors and geographic area.2,3
In Brazil, HTLV-1 infection is considered endemic, and all Brazilian regions exhibit HTLV-1 and HTLV-2 infections; however, the prevalence rates differ among states and are higher in the states of Bahia, Pernambuco and Pará.4
Many studies point to the spread of the virus through vertical transmission, from mother to child at delivery and during prolonged breastfeeding, as well as through unprotected sex.5,6 In addition, the virus can be transmitted by sharing needles/syringes among persons who inject drugs and through blood transfusions.5
HTLV-1 is associated with multiple diseases, including tropical spastic paraparesis or HTLV-associated myelopathy (TPS/HAM), which is characterized by chronic and progressive inflammatory and neurodegenerative disease.7 This process leads to demyelination of spinal cord neurons and has a higher prevalence in individuals aged 40–50 years.8
In this regard, early diagnosis and timely initiation of treatment are needed for decreasing the progression of TPS/HAM and, consequently, improving the quality of life of patients with HTLV-1.9
The limitations caused by this disease affect various facets of life, including physical, psychological and social aspects; therefore, it is important to perform multidisciplinary monitoring, aiming to “minimize psychological, neurological and cognitive impairment, supporting the adaptation to the changes resulting from the disease”.10
The objective of this study was to analyze activity limitations, risk awareness, social participation, quality of life, and pain in HTLV-1-infected individuals receiving care at a reference unit in the Brazilian Amazon.
Materials and methodsType of studyThis was an observational, descriptive, analytical, cross-sectional study with a quantitative approach. The study was conducted from the second semester of 2016 through the end of the first semester of 2018, in the Laboratório de Clínica e Epidemiologia de Doenças Endêmicas (LCEDE) and in the Laboratório de Estudos em Reabilitação Funcional (LAERF) of the Universidade Federal do Pará (UFPA).
SamplePatients were contacted on the day of the visit or by telephone to inquire about the possibility of participating in the study. Four patients did not agree to participate, one had a stroke and was thus excluded, and contact was attempted by telephone with 19 patients but without response.
Thus, a total sample of 55 patients diagnosed with HTLV-1, treated at the aforementioned sites, older than 18 years, and agreeing to participate in the study were included. All patients signed an informed consent form, after being informed about the objective of the study.
The sample was stratified into symptomatic (with TPS/HAM) and asymptomatic (without TPS/HAM) patients, following criteria previously described.11
InstrumentsThe instruments used for data collection were an interview questionnaire created by the authors, the SALSA and Social Participation scales, the Brazilian version of a quality of life questionnaire (SF-36), and the Brief Pain Inventory.
The SALSA Scale was developed through studies of the International Classification of Functionality, Disability and Health (CIF). Therefore, it evaluates the patient’s daily life activities related to the domains “eyes, hands (dexterity and work), feet (mobility), and self-care”.12 It is noteworthy that daily living activities are quotidian practices performed by the individuals enabling their personal independence.12
The SALSA scale assesses the limitations of patients using a score ranging from 10 to 80, where a score close to 10 indicates a person with mild limitations and a score close to 80 indicates a person with very severe limitations. It also assesses risk awareness through a score ranging from 0 to 11, where the closer the score is to 11, the greater the awareness one has of the risk that his/her activities may have.
The Participation scale also uses a score, which ranges from 0 to 90, where zero indicates a person with no restrictions and 90 indicates a person with extreme restrictions.
The SF-36 score (quality of life) is calculated in a two-step process: the first step involves weighting the data, and the second step involves raw scale calculation. In this last step, each domain has a value that ranges from 0 to 100, where the closer the score is 100, the better the quality of life related to that domain.
The Brief Pain Inventory does not generate an overall score; each of its questions are evaluated separately.
Statistical analysisThe obtained data were stored in Microsoft Access 2007 software. Statistical analyses were performed using BioEstat 5.3.13
Sociodemographic and epidemiological characteristics were described using descriptive statistics. Categorical variables are expressed as frequencies and percentages, and numerical variables are presented as medians and quartile deviations.
The Kolmogorov-Smirnov test was used to evaluate normality, and the F test was used to evaluate homogeneity of variances of the numerical variables. Fisher’s exact test was used to test the association of the classification in the SALSA scale and the Participation scale with the presence or absence of symptoms. The Mann–Whitney test was used to identify differences between the symptomatic and asymptomatic groups regarding pain intensity and interference with quality of life. To evaluate the correlation of the quality of life score per domain with pain intensity and interference, Spearman’s correlation coefficient was applied. The level of significance used throughout the study was 5%.
Ethical aspectsThe present study was submitted to and approved by the Research Ethics Committee of the Health Sciences Institute (ICS) of the Universidade Federal do Pará (UFPA) (opinion number 1,592,979).
ResultsFifty-five patients were evaluated and classified as asymptomatic (62%) or symptomatic (38%). In both groups, there was a predominance of patients aged between 41 and 50 years (35.3% asymptomatic and 38.1% symptomatic). In the asymptomatic group and the symptomatic group, 47.1% and 42.9%, respectively, had completed only secondary education. The frequency of individuals with higher education was small in both groups. Regarding marital status, married individuals were more frequent, corresponding to 64.7% of asymptomatic patients and 52.4% of symptomatic patients.
When analyzing the frequency of patient occupations, 20.6% of the asymptomatic patients performed domestic activities, 17.7% were retired, and 17.7% self-employed. While in the symptomatic group, 33.3% were retired.
Regarding family income, 26.5% of asymptomatic patients received up to one salary (minimum wage per month of US$ 249.86), 52.9% from one to less than two salaries, and 20.6% more than two minimum wages. While 11% of symptomatic patients received only the minimum wage, 33.3% received from one to less than two salaries, 9.5% more than two salaries, and 4.8% did not want to inform.
Epidemiological characteristicsRegarding epidemiological characteristics, most patients in both groups had not received blood transfusions; however, those in the asymptomatic group who reported to have received transfusions did so approximately 30–40 years ago (37.5%).
Sexual intercourse was still reported by 70.6% of asymptomatic patients and by 66.7% of symptomatic patients. Notably, 8.3% of symptomatic patients had more than one partner at the time of the study. When questioned about use of contraceptive methods, 73.5% among asymptomatic and 76.2% among symptomatic responded that they did not use. However, in both groups, use of condoms was referred as the most commonly used method. Regarding the frequency of use, 57.1% of asymptomatic individuals claimed to use it sometimes whereas 75.0% of symptomatic patients claimed to use it always.
Clinical characteristicsRegarding clinical characteristics features, 71.4% of symptomatic patients reported weakness in the legs and 76.2% reported pain in the lumbar spine. Most asymptomatic patients did not report clinical features related to HTLV-1 infection (easy tiredness, frequent falls, skin changes, constipation, leg pain, loss of sensation, altered gait, dry mouth and blurred vision).
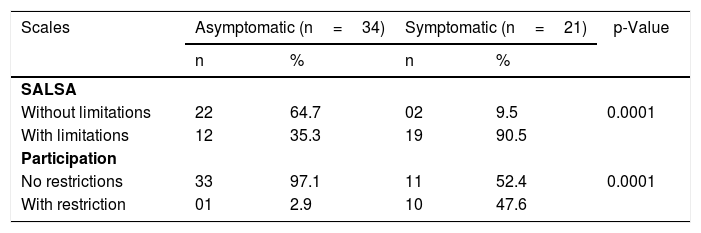
The SALSA scale showed a significant difference regarding patient limitations; 90.5% of symptomatic patients had limitations compared to 35.3% of asymptomatic patients (p=0.0001). Analysis of the risk awareness score, also measured by the SALSA scale, showed variation from 0 to 8 in the asymptomatic group and from 0 to 7 in the symptomatic group. Both groups exhibited a greater frequency of 0.
Regarding the Participation scale, there was also a difference between patients: 47.6% of symptomatic patients exhibited limitations compared to 2.9% of asymptomatic patients (p=0.0001) (Table 1).
Distribution of patients according to SALSA and Participation scale scores in symptomatic and asymptomatic patients.
| Scales | Asymptomatic (n=34) | Symptomatic (n=21) | p-Value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| SALSA | |||||
| Without limitations | 22 | 64.7 | 02 | 9.5 | 0.0001 |
| With limitations | 12 | 35.3 | 19 | 90.5 | |
| Participation | |||||
| No restrictions | 33 | 97.1 | 11 | 52.4 | 0.0001 |
| With restriction | 01 | 2.9 | 10 | 47.6 | |
According to the Brief Pain Inventory, pain was reported by 100% of symptomatic patients, being more frequent in the knees. An expressive percentage (47.1%) of asymptomatic patients reported pain, especially in the lumbar spine. The symptomatic patients reported that they resorted to pain relief medication, but 33% did not remember the name of the medication used, and 19% reported to have used anti-inflammatory medication.
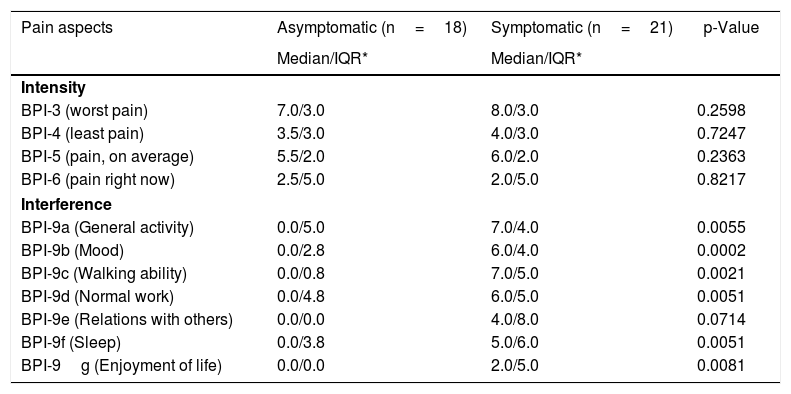
Symptomatic and asymptomatic patients had pain intensity according to the Brief Pain Inventory (Table 2). However, when comparing pain interference, patients with symptoms had a greater degree of pain interference in the aspects of general activity (p=0.0055), mood (p=0.0002), walking ability (p=0.0021), normal work (p=0.0051), sleep (p=0.0051), and enjoyment of life (p=0.0081). It is noteworthy that the aspect 'relationship with other people' was the only one that had no significant difference between symptomatic and asymptomatic patients (Table 2).
Distribution of patients according to pain intensity and interference with life in symptomatic and asymptomatic patients.
| Pain aspects | Asymptomatic (n=18) | Symptomatic (n=21) | p-Value |
|---|---|---|---|
| Median/IQR* | Median/IQR* | ||
| Intensity | |||
| BPI-3 (worst pain) | 7.0/3.0 | 8.0/3.0 | 0.2598 |
| BPI-4 (least pain) | 3.5/3.0 | 4.0/3.0 | 0.7247 |
| BPI-5 (pain, on average) | 5.5/2.0 | 6.0/2.0 | 0.2363 |
| BPI-6 (pain right now) | 2.5/5.0 | 2.0/5.0 | 0.8217 |
| Interference | |||
| BPI-9a (General activity) | 0.0/5.0 | 7.0/4.0 | 0.0055 |
| BPI-9b (Mood) | 0.0/2.8 | 6.0/4.0 | 0.0002 |
| BPI-9c (Walking ability) | 0.0/0.8 | 7.0/5.0 | 0.0021 |
| BPI-9d (Normal work) | 0.0/4.8 | 6.0/5.0 | 0.0051 |
| BPI-9e (Relations with others) | 0.0/0.0 | 4.0/8.0 | 0.0714 |
| BPI-9f (Sleep) | 0.0/3.8 | 5.0/6.0 | 0.0051 |
| BPI-9g (Enjoyment of life) | 0.0/0.0 | 2.0/5.0 | 0.0081 |
Patients from each group, using the SF-36, rated their health compared to the same period a year ago. The asymptomatic group responded more frequently ‘about the same’ (47.1%), whereas 29.4% of patients responded ‘slightly worse’, and 2.9% responded ‘much worse’. In the symptomatic group, the most frequent response was ‘slightly worse’ (33.3%), followed by ‘much worse’ (28.6%).
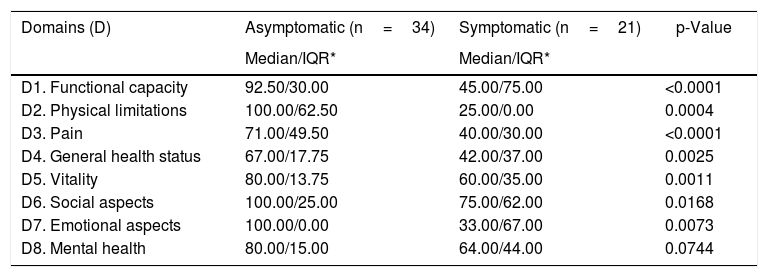
Analysis of SF-36 scale showed that asymptomatic patients have better quality of life than symptomatic patients. The significant results were related to the following domains: functional capacity (p=<0.0001), physical limitations (p=0.0004), pain (p=<0.0001), general health status (p=0.0025), vitality (p=0.0011), social aspects (p=0.0168) and emotional aspects (p=0.0073) (Table 3). It should be pointed out that only the mental health domain had no statistical difference, which demonstrates that there is no relationship between the mental health domain and the classification of patients between symptomatic and asymptomatic.
Distribution of patients according to quality of life (SF-36) score in symptomatic and asymptomatic patients.
| Domains (D) | Asymptomatic (n=34) | Symptomatic (n=21) | p-Value |
|---|---|---|---|
| Median/IQR* | Median/IQR* | ||
| D1. Functional capacity | 92.50/30.00 | 45.00/75.00 | <0.0001 |
| D2. Physical limitations | 100.00/62.50 | 25.00/0.00 | 0.0004 |
| D3. Pain | 71.00/49.50 | 40.00/30.00 | <0.0001 |
| D4. General health status | 67.00/17.75 | 42.00/37.00 | 0.0025 |
| D5. Vitality | 80.00/13.75 | 60.00/35.00 | 0.0011 |
| D6. Social aspects | 100.00/25.00 | 75.00/62.00 | 0.0168 |
| D7. Emotional aspects | 100.00/0.00 | 33.00/67.00 | 0.0073 |
| D8. Mental health | 80.00/15.00 | 64.00/44.00 | 0.0744 |
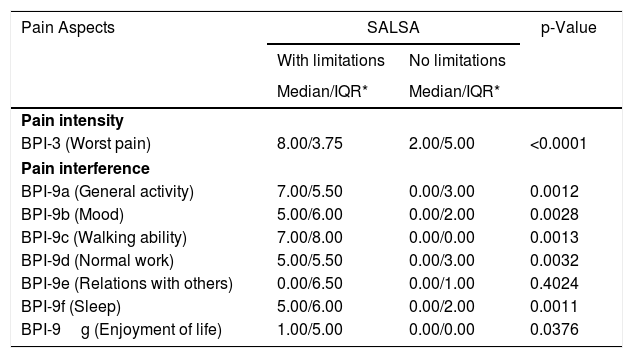
Table 4 shows the relationship between intensity of the worst pain and pain interference on the Brief Pain Inventory and the SALSA scale (with and without limitation) and the Participation scale (with and without restriction).
Relationship between the Brief Pain Inventory and the SALSA and Participation scales.
| Pain Aspects | SALSA | p-Value | |
|---|---|---|---|
| With limitations | No limitations | ||
| Median/IQR* | Median/IQR* | ||
| Pain intensity | |||
| BPI-3 (Worst pain) | 8.00/3.75 | 2.00/5.00 | <0.0001 |
| Pain interference | |||
| BPI-9a (General activity) | 7.00/5.50 | 0.00/3.00 | 0.0012 |
| BPI-9b (Mood) | 5.00/6.00 | 0.00/2.00 | 0.0028 |
| BPI-9c (Walking ability) | 7.00/8.00 | 0.00/0.00 | 0.0013 |
| BPI-9d (Normal work) | 5.00/5.50 | 0.00/3.00 | 0.0032 |
| BPI-9e (Relations with others) | 0.00/6.50 | 0.00/1.00 | 0.4024 |
| BPI-9f (Sleep) | 5.00/6.00 | 0.00/2.00 | 0.0011 |
| BPI-9g (Enjoyment of life) | 1.00/5.00 | 0.00/0.00 | 0.0376 |
| Participation | |||
|---|---|---|---|
| With restrictions | Without restrictions | ||
| Median/IQR | Median/IQR | ||
| Pain intensity | |||
| BPI-3 (Worst pain) | 8.00/2.50 | 5.00/8.00 | 0.1681 |
| Pain interference | |||
| BPI-9a (General activity) | 7.50/4.25 | 3.50/6.50 | 0.0162 |
| BPI-9b (Mood) | 7.00/5.25 | 1.50/5.00 | 0.0069 |
| BPI-9c (Walking ability) | 7.50/3.75 | 0.00/7.00 | 0.0100 |
| BPI-9d (Normal work) | 6.50/4.50 | 3.50/6.50 | 0.0255 |
| BPI-9e (Relations with others) | 4.50/4.75 | 0.00/0.00 | 0.0037 |
| BPI-9f (Sleep) | 5.00/5.25 | 2.00/5.75 | 0.0299 |
| BPI-9g (Enjoyment of life) | 5.00/3.50 | 0.00/0.00 | 0.0004 |
In patients with activity limitation, the relationship between pain intensity and interference were more pronounced than for patients without activity limitation, in all aspects evaluated, except for pain interference related to the aspect 'relationships with other people’ (p=0.0714). Thus, one could suggest that pain causes changes in several aspects in patients who have physical activity limitations.
Regarding the relationship between pain and the Participation scale, pain interference was higher among patients with restricted social participation, in all aspects evaluated (Table 4). Thus, pain is an interference factor in social life, restricting or even preventing patients from maintaining an active social life.
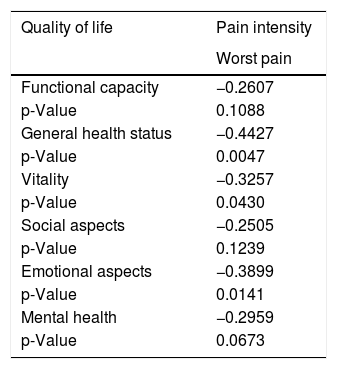
Table 5 shows the correlation between the SF-36 scale and the worst pain identified by the Brief Pain Inventory. Pain influenced patients’ quality of life. Notably, the worst pain intensity was significantly correlated with general health status (r=-0.4427; p=0.0047), vitality (r=-0.3257; p=0.0430) and emotional aspects (r=−0.3899; p=0.0141). It is suggested that, whenever the patient is in a lot of pain (worse referred pain), the quality of life related to general health status, vitality and emotional aspects decrease, that is, the greater the intensity of pain, the lower the quality level of life of patients.
Correlation of pain intensity evaluated by the Brief Pain Inventory with quality of life (SF-36).
| Quality of life | Pain intensity |
|---|---|
| Worst pain | |
| Functional capacity | −0.2607 |
| p-Value | 0.1088 |
| General health status | −0.4427 |
| p-Value | 0.0047 |
| Vitality | −0.3257 |
| p-Value | 0.0430 |
| Social aspects | −0.2505 |
| p-Value | 0.1239 |
| Emotional aspects | −0.3899 |
| p-Value | 0.0141 |
| Mental health | −0.2959 |
| p-Value | 0.0673 |
In the present study, there was a higher prevalence of asymptomatic HTLV-1 patients, corroborating other studies.14,15 Most people with HTLV-1 infection remain asymptomatic14; however, it is important to be highly vigilant so as to notice mild signs and/or symptoms.16
Both symptomatic and asymptomatic patients had only 11 years of formal education, corroborating the findings of other studies.14,16 Notably, this is a relevant factor because patients with low education level may have difficulty understanding the recommentations conveyed by healthcare professionals. That may negatively affect counseling, clinical follow-up, and adherence to prevention activities.17
With regard to marital status, there was a higher frequency of married patients in both groups, corroborating another study that found a greater prevalence of patients with partners.14
Occupations are of great importance in society, and in this study, symptomatic patients were more frequently retired, which has also been described in the HTLV Reference Center in the city of Salvador.18 Such a situation may be explained by the advanced age of most symptomatic patients, as well as motor limitations for performing some work activities, leading to retirement to preserve the family income.
The types of occupations observed in our study allow us to understand the family income, which was reported by symptomatic patients to be up to one minimum wage, corroborating another study.19 It is noteworthy that the family's financial income is of paramount importance for maintaining needs at home, in addition to assisting in the treatment of symptomatic patients.
The majority of the participants reported not having received blood transfusions. However, 37.5% of asymptomatic and 30% of asymptomatic patients had received blood transfusions between 30 and 40 years ago, a practice that is associated with high rates of transmission due to the infusion of infected lymphocytes. This mode of transmission may be associated with the abrupt onset of TSP/HAM. Because of such issues, screening for antibodies against HTLV is necessary to prevent transmission, besides allowing to estimate the prevalence of infection.20
Sexual intercourse was still practiced by most patients, emphasizing the importance of sex education actions and/or sexual counseling17 because infection can spread, thus perpetuating the transmission chain. The use of condoms however, was still unfrequently used by patients in this study.
A retrospective study conducted in the same place (LCEDE) in 2015 identified that patients had risky behaviors, since they had extramarital sex without using condoms.21 It is known that such an attitude can help explain the dynamics of virus transmission, with different prevalence rates between locations.22 In addition, health education practices are important as a way of educating and answering patients' doubts.
Some characteristics are commonly seen in symptomatic patients and follow a specific order of manifestation: mild sensory and motor signs, as well as urinary disorders, and subsequently the presence of leg weakness and a positive Babinski sign.23
Our study found that most patients reported leg weakness, which demonstrates advanced progression of the symptoms. Within this context, the use of physical therapy is relevant because as leg weakness causes significant functional impairment in patients.24
HTLV infection leads to numerous limitations in activities of daily living in addition to changes in daily life.25 According to the SALSA scores, there was a prevalence of asymptomatic patients without limitations in activities of daily living.
Importantly, this scale can be used as an instrument for clinical follow-up. As the score increases, follow-up should be intensified to avoid activity limitations as a consequence of HTLV-1 symptoms.25
Among symptomatic patients, activity limitations were reported possibly because patients with TPS/HAM have functional problems that limit the performance of daily life activities.26–28
In this study, most patients had a score of 0 on the assessment of risk awareness measured by the SALSA scale, i.e., such patients do not consider the risks involved in their activities. This is a worrisome factor because these patients can suffer consequences due to the activities they perform routinely.
Most participants in this study, from both groups, were classified as having no social participation restrictions; i.e., they did not experience difficulties in social life due to HTLV infection. However, some of the symptomatic patients exhibited some level of restriction, as TPS/HAM caused not only functional but also social and emotional consequences.26,29
Physical limitations interfere with the performance of daily activities as well as the autonomy and privacy of patients.25 Thus, the infection causes changes that also affect social life, as the relationship between people is affected, as well as the relationship within the work environment and/or with the work itself.
In this study pain was more frequently reported by symptomatic patients, corroborating another study.30 Symptomatic individuals were 1.21 times more likely than asymptomatic individuals to present with pain.14 However, a significant fraction of asymptomatic patients complained of pain in the lumbar spine, underscoring the need for continuous clinical monitoring of these patients.
Sociodemographic factors, as well as the means of transportation used, and environmental issues can contribute to the onset of pain in people without symptoms.30,31 Those factors may also explain the presence of pain in asymptomatic patients in this study, in particular regarding occupations – domestic services – that require physical exertion and fitness.
The location of pain in the lower limbs and in the spine corroborates previous findings.30,32 The presence of constant pain is a factor that predisposes patients to indiscriminately use anti-inflammatory medication, characterized as a regular behavior among patients with some symptomatology.14,33 Although this condition is common, such a situation should be monitored more diligently to avoid consequences of the constant use of these drugs, which are often not prescribed by a doctor.
In the present study, asymptomatic patients had higher quality of life than did symptomatic patients, corroborating results from another study that reported low quality of life in patients with TPS/HAM.34 These results may be explained because patients with TPS/HAM have greater impairment of quality of life domains than do asymptomatic patients.
After evaluating quality of life among symptomatic patients in this study, the domains most affected were emotional aspects, pain and limitations in physical activities. These findings corroborate the results from studies by Martins et al.32 and Caifa et al.26 who identified “pain (D3)” and “physical limitations (D2)”, respectively, as greatly affecting the quality of life of patients with TPS/HAM.
ConclusionThis study used scales to evaluate HTLV-1 infected patients. The SALSA and Participation scales were relevant for clinical evaluation of limitation of activities and social participation. These patients need continued assessment of their physical, emotional and social aspects for better assistance.
The Brief Pain Inventory and SF-36 scales were essential for tracking pain, its intensity and interference in activities, as well as with quality of life. Pain causes several discomforts, which can ultimately affect patient's quality of life.
Therefore, clinical follow-up instruments such as those used in the present study must be adopted by different healthcare professionals to monitor new symptoms so as to avoid the onset of limitations identified in symptomatic patients.
It is relevant to emphasize that asymptomatic patients should be evaluated and assisted routinely, since TSP/HAM can evolve to more complex conditions.
This study also points to the need to support symptomatic HTLV-1 infected patients through therapeutic interventions, such as physical therapy (Pilates), to address leg weakness, as well as social and emotional support therapies because the infection causes changes that affect social life.35 Although the groups in the present study did not have restrictions related to social participation, such changes impact relationships between people, the work environment, and work itself.
Notably, pain should be better evaluated, and professionals should employ various therapeutic resources to relieve pain, thus preventing self-medication by patients, as observed in this study. Furthermore, pain interferes in the lives of patients and impairs quality of life.
Thus, further research and improved care from healthcare professionals are needed so that these patients can be supported and assisted as their clinical condition evolves.
FundingThis study was supported by the National Council for Scientific and Technological Development (CNPq; # 301869/2017-0) and the Dean of Research and Graduate Studies (PROPESP/UFPA – Public Notice PAPQ 2020).
Conflicts of interestThe authors declare no conflicts of interest.
We thank all patients who agreed to participate in the study.