Shoulder arthroplasty (SA) has been performed by many years for the treatment of several conditions, including osteoarthritis and proximal humeral fractures following trauma. Surgical site infection (SSI) following Shoulder arthroplasty remains a challenge, contributing to increased morbidity and costs. Identification of risk factors may help implementing adequate strategies to prevent infection. We aimed to identify pre- and intra-operative risk factors associated with deep infections after Shoulder arthroplasty.
MethodsAn unmatched case-control study was conducted to describe the prevalence, clinical and microbiological findings, and to evaluate patient and surgical risk factors for prosthetic shoulder infection (PSI), among 158 patients who underwent SA due to any reason, at a tertiary public university institution. Risk factors for PSI was assessed by uni- and multivariate analyses using multiple logistic regression.
Results168 SA from 158 patients were analyzed, with an overall infection rate of 9.5% (16/168 cases). Subjects undergoing SA with American Society of Anesthesiologists (ASA) grade III or higher (odds ratio [OR]=5.30, 95% confidence interval [CI]=1.58–17.79, p<0.013) and presenting local hematoma after surgery (odds ratio [OR]=7.10, 95% confidence interval [CI]=1.09–46.09, p=0.04) had higher risk for PSI on univariate analysis. However, only ASA score grade III or higher remained significant on multivariate analysis (OR=4.74, 95% CI=1.33–16.92, p=0.016). Gram-positive cocci and Gram-negative bacilli were equally isolated in 50% of cases; however, the most commonly detected bacterium was Pseudomonas aeruginosa (18.7%).
ConclusionThis study provides evidence suggesting that patient-related known factors such as higher ASA score predisposes to shoulder arthroplasty-associated infection. Furthermore, unusual pathogens associated with PSI were identified.
Hemiarthroplasty (HA) and total shoulder arthroplasty (TSA) have been increasingly performed for the treatment of several osteoarticular conditions such as osteoarthritis, humeral head avascular necrosis and proximal humeral fractures following traumas.1,2 Indeed, the annual number of HA and TSA performed in the United States is growing faster, reaching more than 50,000 shoulder replacements per year.3 The incidence of periprosthetic shoulder infections (PSI) appears to be less than that of periprosthetic hip (THA) and knee (TKA) infections, though there have been reports of higher rates in the surgery literature.4,5 Periprosthetic shoulder infections, nonetheless, remain challenging as they increase morbidity as well as raise costs.6 The rate of infectious complication following primary shoulder arthroplasties appears to be as lower as the rates associated with primary hip and knees arthroplasties, while few single-center studies have demonstrated higher rates of PSI.1,4–6
There have been few previous studies analyzing risk factors for PSI.7–9 Patient related-factors and comorbidities such as male gender, younger age, diabetes, morbid obesity, rheumatoid arthritis, and other types of immunosuppression including tumors, have already been implicated.7,10 Surgical-related factors such as peri-operative hematomas and prior surgeries, especially in the trauma setting, increase the incidence of infection after primary shoulder arthroplasty.1,7,11
In addition, the role of biofilm-forming bacteria, such as Propionibacterium acnes, but also Staphylococcus, and Streptococcus in the pathogenesis of orthopedic implant-associated infections, particularly PSI has been widely accepted.12–16 Although uncommonly implicated in PSI, Pseudomonas is an aerobic Gram-negative bacillus expressing the ability to form complex biofilm structures on the surfaces of orthopedic implants.17,18 In one large study addressing Gram-negative prosthetic joint infections, Pseudomonas aeruginosa was by far the most frequently (40%) isolated pathogen.19
We herein sought to identify pre- and intra-operative risk factors predisposing subjects to develop deep infections following HA and TSA, and evaluate causative microorganisms associated with PSI.
MethodsStudy populationWe performed a single-center case-control study with 183 subjects submitted to either HA or TSA that were performed at the Department of Orthopedics and Traumatology of a large urban public teaching hospital, between January 1987 and November 2012. The study included subjects with at least 24 months of follow-up after the surgical implantation of shoulder arthroplasty. Exclusion criteria were age less than 18 years, follow up of less than 24 months, arthroplasties performed for malignant etiologies, prior radiation of the operative site, and patients whose medical records were unavailable. The study was reviewed and approved by the local Institutional Review Board.
Diagnosis of periprosthetic shoulder infection (PSI)PSI was diagnosed according to IDSA guidelines by the presence of a sinus tract communicating with the prosthesis, histopathological analyses with the presence of inflammatory cells, visible purulence surrounding the prosthesis, and/or identical microorganisms isolated from two or more cultures. PSI was categorized as early when diagnosed before three months after surgery; intermediate when diagnosed between three and 24 months after surgery; and late infection when diagnosed after two years of prosthesis implantation.20 Subjects who fulfilled the diagnostic criteria for PSI were considered cases for this study. Relapses at the same joint prosthesis were not considered for analysis. Controls were subjects who had undergone shoulder arthroplasty due to any indication except joint infection and did not develop PSI during follow-up.
Potential risk factorsTo identify potential risk factors associated with PSI, several variables (patient, microbiological findings, and surgery associated variables) were assessed by reviewing medical, intra-operative, and microbiological records. We searched for demographic variables, comorbidities, American Society of Anesthesiologists (ASA) classification, preoperative diagnosis, primary or revision arthroplasty, previous history of local or systemic infection, use of systemic antibiotic 14 days prior to surgery, or any hospital admission at least three months before surgery. Surgical-related variables including type of implant, need for blood transfusion, duration of surgery, and surgeon's experience level were recorded. The level of experience of the surgeon was categorized as high for senior doctors and head of the group; average for new graduates; and low for medical residents.
Statistical analysisFor statistical analysis qualitative variables were described as mean and percentage, and quantitative variables were described as median and standard deviation. The association between qualitative variables were assessed by chi-square test and Fisher's exact test. For associations between quantitative variables we used univariate logistic regression. Risk estimates were calculated for the variables associated with PSI and reported as odds ratios with 95% confidence interval (CI). Variables that in univariate analysis had a p-value less than 0.20 were included in the multiple logistic regression model to assess their independent association with PSI. Epi-Info® Version 3.22 software was used for data tabulation and SPSS version 20.0 (SPSS, Chicago, IL, USA) for statistical analysis.
ResultsStudy populationDuring the study period of 1987–2012, a total of 183 subjects were included. Twenty-five subjects (13.6%) were excluded from further analysis: 10 due to lack of complete medical information, 12 had less than 24 months of follow up, and three had a diagnosis of shoulder tumor. One-hundred and sixty-eight shoulder implants in 158 subjects (10 subjects had bilateral shoulder prosthesis implanted at different time intervals) were analyzed. Eighty-one percent of these implants were shoulder hemiarthroplasties. After 24 months of follow up, PSI were observed in 9.5% (16/168) of analyzed cases. The clinical characteristics and comorbidities were similar in infected (PSI) and non-infected (NISA) groups (Table 1). Of note, among the 16 subjects presenting PSI, 14 (87.5%) had hemiarthroplasties and two (12.5%) total arthroplasties; in 13 out of the 16 (81.2%) PSI occurred during the first half of the study period while only three (18.8%) occurred in the second half, though this did not reach statistical significance (p=0.103). Table 2 summarizes the 16 clinical cases of PSI concerning demographics, ASA score, diagnosis prior to arthroplasty, type of surgery, presence of hematoma, time elapsed between surgery and PSI, microorganism identified, and the selected medical treatment.
Demographics, comorbidities, and operative characteristics of PSI and NISA study groups. Univariate and multivariate analysis of risk factors associated to develop PSI.
| Variables | Prosthetic shoulder surgeries | Univariate analysis | Multivariate analysis | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| NISA (n=152) | PSI (n=16) | OR | IC (95%) | p-value | OR | IC (95%) | p-value | |||
| Lower | Upper | Lower | Upper | |||||||
| Demographic data | ||||||||||
| Male | 37 (24.3) | 7 (43.7) | 2.42 | 0.84 | 6.94 | 0.131a | 0.68 | 0.84 | 50.7 | 0.174 |
| Age | ||||||||||
| Average | 58.4 (14.1) | 55.8 (15.7) | 0.99 | 0.95 | 1.02 | 0.486c | 1.01 | 0.96 | 1.06 | 0.693 |
| Median (range min- max) | 60.5 (22–80) | 55 (22–77) | ||||||||
| Comorbidities | ||||||||||
| Hypertension | 58 (38.1) | 8 (50) | 1.62 | 0.58 | 4.55 | 0.356 | ||||
| DM | 18 (11.8) | 2 (12.5) | 1.06 | 0.22 | 5.07 | >0.999 | ||||
| Rheumatoid arthritis | 7 (21.7) | 1 (6.3) | 1.38 | 0.16 | 11.99 | 0.559 | ||||
| Pulmonary comorbidity | 1 (0.6) | 0 (0) | a | >0.999 | ||||||
| HIV | 2 (1.3) | 0 (0) | a | >0.999 | ||||||
| Smoker | 30 (19.7) | 4 (25) | 1.36 | 0.41 | 4.50 | 0.743 | ||||
| Alcohol dependency | 12 (7.9) | 3 (18.7) | 2.69 | 0.67 | 10.78 | 0.158 | ||||
| Sickle cell disease | 3 (2) | 0 (0) | a | >0.999 | ||||||
| Hypothyroidism | 8 (5.2) | 0 (0) | a | >0.999 | ||||||
| Hepatitis | 3 (2) | 1 (6.3) | 3.31 | 0.32 | 33.85 | 0.332 | ||||
| Epilepsy | 11 (7.2) | 1 (6.3) | 0.86 | 0.10 | 7.09 | >0.999 | ||||
| Corticoid use | 1 (0.6) | 0 (0) | a | >0.999 | ||||||
| Chemotherapy | 2 (1.3) | 0 (0) | a | >0.999 | ||||||
| Preoperative characteristics | ||||||||||
| Diagnosis | 0.148b | |||||||||
| Acute fracture PH | 59 (38.8) | 10 (62.5) | 1.00 | |||||||
| LPTN | 48 (31.5) | 4 (25) | 0.49 | 0.15 | 1.67 | |||||
| AAHN | 45 (29.6) | 2 (12.5) | 0.26 | 0.06 | 1.26 | |||||
| Reoperation | 22 (14.5) | 2 (12.5) | 0.84 | 0.18 | 3.97 | >0.999 | ||||
| Previous Antibiotic UseA | 13 (8.6) | 1 (6.3) | 0.71 | 0.09 | 5.84 | >0.999 | ||||
| Previous InfectionA | 6 (3.9) | 0 (0) | a | >0.999 | ||||||
| HospitalizationA | 8 (5.3) | 2 (12.5) | 2.57 | 0.50 | 13.31 | 0.244 | ||||
| Preoperative hospitalization | ||||||||||
| >7 days | 51 (33.6) | 6 (37.5) | 1.17 | 0.40 | 3.39 | 0.779 | ||||
| Intraoperative characteristics | ||||||||||
| ASA class | ||||||||||
| I/II | 140 (92.1) | 11 (68.8) | 1.00 | 1.00 | ||||||
| III | 12 (7.9) | 5 (31.2) | 5.3 | 1.58 | 17.79 | 0.013 | 4.74 | 1.33 | 16.92 | 0.016 |
| Surgery | 0.739 | |||||||||
| Hemiarthroplasty | 30 (19.7) | 2 (12.5) | 1.00 | |||||||
| TSA | 122 (80.3) | 14 (87.5) | 1.72 | 0.37 | 7.99 | |||||
| Intraoperative BT | 2 (1.3) | 0 (0) | a | >0.999 | ||||||
| Operative length of time | ||||||||||
| >2h | 135 (88.9) | 16 (100) | A | 0.369 | ||||||
| Antibiotic prophylaxis | 0.523 | |||||||||
| Cefazoline | 142 (93.4) | 15 (93.8) | 0.53 | 0.06 | 4.82 | |||||
| Surgeon experience | 0.393 | |||||||||
| High | 135 (88.8) | 15 (93.8) | 1.00 | |||||||
| Median | 9 (5.9) | 0 (0) | a | |||||||
| Low | 8 (5.3) | 1 (6.3) | 1.13 | 0.13 | 9.62 | |||||
| Postoperative characteristics | ||||||||||
| Hematoma requiring drainage | 3 (2) | 2 (12.5) | 7.10 | 1.09 | 46.09 | 0.04c | 6.51 | 0.84 | 50.70 | 0.074 |
| Postoperative BT | 2 (1.3) | 0 (0) | a | >0.999 | ||||||
Chi-square test; a, OR, odds ratio; IC (95%), 95% of confidence interval; DM, diabetes mellitus; HIV, human immunodeficiency virus; min, minimum; max, maximum; PSI, periprosthetic shoulder infection; NISA, non infected shoulder arthroplasty; Acute fracture PH, acute fracture of the proximal humerus; TSA, total shoulder arthroplasty; A, last three months; AANU, arthritis, arthropathy and humeral necrosis; LPTN, luxations and post-traumatic humeral necrosis; BT, blood transfusion.
Summary of 16 cases of infection after shoulder arthroplasty.
| Case | Gender | Age | ASA | Reoperation | Diagnosis | Surgery | Hematoma | Period of infection | Etiological agent |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 69 | I | No | Glenohumeral arthrosis | H | No | Early | Enterococcus sp |
| 2 | M | 75 | III | No | Posterior shoulder dislocation | H | No | Late | S. aureus |
| 3 | F | 72 | I | No | PHF | H | No | Delayed | P. aeruginosa |
| 4 | F | 80 | III | No | PHF | H | No | Early | Enterobacter sp |
| 5 | M | 78 | II | No | PHF | H | No | Delayed | S. epidermidis |
| 6 | F | 60 | I | No | Glenohumeral arthrosis | TSA | No | Late | Unidentified |
| 7 | M | 65 | III | No | PHF | H | No | Late | P. aeruginosa |
| 8 | M | 48 | II | No | PHF | H | No | Early | Enterococcus sp |
| 9 | F | 77 | II | No | PHF | H | Yes | Early | Unidentified |
| 10 | F | 98 | III | No | PHF | H | No | Delayed | Unidentified |
| 11 | M | 62 | III | Yes | PHF | H | Yes | Early | S. epidermidis, M. morganii |
| 12 | F | 86 | II | No | PHF | H | No | Early | Unidentified |
| 13 | M | 86 | II | No | Post-traumatic humeral necrosis | H | No | Delayed | Unidentified |
| 14 | F | 81 | II | No | PHF | H | No | Early | P. mirabilis, S. aureus, P. aeruginosa |
| 15 | M | 59 | I | No | PHF | H | No | Late | Unidentified |
| 16 | F | 80 | II | Yes | Post-traumatic humeral necrosis | TSA | No | Early | Unidentified |
Source: Medical files from DOTSCMSP.
S. aureus, Staphylococcus aureus; S. epidermidis, Staphylococcus epidermidis; M. morganii, Morganela morganii; P. mirabilis, Proteus mirabilis; P. aeruginosa, Pseudomonas aeruginosa; F, female; M, male; PHF, proximal humeral fracture; H, hemiarthroplasty; TSA, total shoulder arthroplasty; ASA, American Society of
Anesthesiologists.
The results of the uni- and multivariate analysis of risk factors for PSI are presented in Table 1. Demographic variables, comorbidities, underlying diagnosis, and all other pre-operative characteristics were not significantly associated with PSI. On the other hand, subjects undergoing shoulder arthroplasty with ASA grade III or higher (odds ratio [OR]=5.30, 95% confidence interval [CI]=1.58–17.79, p<0.013) and presenting local hematoma after surgery (odds ratio [OR]=7.10, 95% confidence interval [CI]=1.09–46.09, p=0.04) had higher risk for PSI on univariate analysis. Intra-operative aspects such as HA or TSA, blood transfusion (yes/no), duration of surgery longer than 2h, antibiotic prophylaxis, and surgeon's experience were not significantly associated with PSI. On multivariable analysis, only ASA score III or higher remained statistically associated with PSI (odds ratio [OR]=4.74, 95% confidence interval [CI]=1.33–16.92, p=0.016), though hematoma formation showed a trend toward significance (odds ratio [OR]=6.51, 95% confidence interval [CI]=0.84–50.70, p=0.074).
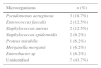
Microbiological findingsPeriprosthetic tissue and synovial fluid cultures identified no pathogens in 43.7% (7/16) of PSI subjects, all of which were using systemic empirical antibiotics prior to surgery. Sonication of retrieved shoulder arthroplasty was performed in only one infected shoulder implant, yielding P. aeruginosa, Staphylococcus aureus, and Proteus mirabilis (patient number 14). The infection was polymicrobial in two cases (12.5%). Gram-negative bacilli (GNB) were detected on 50% of cultures, mostly P. aeruginosa (18.7%). Interestingly, P. acnes was not found in this case series. Table 3 shows the microbiological findings of the 16 patients with PSI.
Microbiological findings of 16 patients with periprosthetic shoulder-associated infection.
| Microorganisms | n (%) |
|---|---|
| Pseudomonas aeruginosa | 3 (18.7%) |
| Enterococcus faecalis | 2 (12.5%) |
| Staphylococcus aureus | 2 (12.5%) |
| Staphylococcus epidermidis | 2 (6.2%) |
| Proteus mirabilis | 1 (6.2%) |
| Morganella morganii | 1 (6.2%) |
| Enterobacter sp | 1 (6.2%) |
| Unidentified | 7 (43.7%) |
Source: Department of Orthopedics e Traumatology of Santa Casa de São Paulo School of Medical sciences medical files.
There have been few studies describing the epidemiology of periprosthetic joint infection (PJI) after shoulder arthroplasty, including microbial etiology, incidence, and predisposing factors. We aimed to investigate the risks of PJI as well as to understand the underlying microbiological aspects in a cohort of subjects who underwent HA and PSA over 25-year period, 1987–2012. While the rates of PJI following TKA and THA seems to be increasing,10 PSI remains relatively stable according to a large US database survey.6 Interestingly, in our study the rate of PSI reached 12.4% during the first 12-year period of 1987–1999, but dropped to 4.8% in the subsequent 13-year period of 2000–2012, although this difference was not statistically significant. Many reasons may have been associated with the reduction of PSI rate over time, but we argue that an improvement in the pre- and intra-operative management of trauma patients in our urban tertiary teaching center may have played a role.
We sought to identify potential risk factors for PSI, and when examining specifically pre-operative variables, such as demographic data and underlying medical comorbidities, no significant association with PSI was found. Conversely, previous studies have associated younger male patients and PSI, possibly due to local trauma and surgical procedures performed for fractures,6,7 while others studies showed PSI to be significantly associated with chronic diseases, including diabetes and rheumatoid arthritis.1 We identified higher rates of proximal humeral acute fractures as the main reason for shoulder arthroplasty; however, we could not find an association with infection.
Compared to HA, TSA is associated with increased difficulty, increased need for blood transfusions, and longer operative times, though recently published studies show superior outcomes with equivalent postoperative complications, including PSI.1,2,7 In the present study, 6.2% of TSA became infected, even though TSA was not statistically associated with PSI. In contrast, we identified a statistically significant association between PSI and patients presenting ASA grade III or higher, which was confirmed on multivariate analysis. In fact, patients presenting ASA grade three or higher had 4.74-fold higher risk of PSI. To the best of our knowledge, no previous studies have identified significant association of ASA grade particularly with shoulder arthroplasty infection. A retrospective cohort study of patients undergoing TSA or reverse TSA with an ASA score grade III or higher found greater risk of surgical complications, including nerve damage and perioperative fracture, but not higher incidence of surgical site infections.21 Composite risk scores aggregate different factors into one and ASA is a six-point scale frequently applied pre-operatively to assess patient's global health and risks for postoperative complications.22 Furthermore, an elevated ASA grade has been shown to increase the rate of infectious complications after orthopedic surgeries, including PJI following THA and TKA and spinal surgeries.10,22 Additionally, in the current study the presence of hematoma formation soon after shoulder arthroplasty was found to be a potential risk of PSI, showing a 7.10-fold higher risk of PSI on univariate analysis, though it did not reach statistical significance likely secondary to the low incidence of PSI in our study. Cheung et al.23 have previously showed an association of postoperative large hematoma formation requiring reoperation and PJI after primary or revision shoulder arthroplasty, in which hematoma formation after PSA was frequently associated with positive intraoperative cultures.
The presence of hair follicles and sebaceous glands do not increase the adherence of bacteria; this is an inherent property of the bacterium. Rather, they likely harbor bacteria that cannot be adequately sterilized with routine peri-operative sterilization procedures.
Studies have associated PSI with higher frequency of chest bacterial colonization, especially the adherence of anaerobic-aerotolerant Gram-positive bacilli such as P. acnes and other colonizers of human skin like Staphylococcus, Streptococcus, and Pseudomonas spp.12–14 Indeed, an increasingly amount of recent data have demonstrated the predominance of P. acnes in PSI.7,10,12–16 Importantly, our microbiological findings added new information to the epidemiology of PSI as GNB were identified in half of periprosthetic cultures. Notwithstanding, because no P. acnes was recovered from our PSI cases, we have modified the microbiological protocol for the diagnosis of PJI in our Institution. Since 2009 we included sonication technique of the retrieved implants, tissue, and synovial fluid culture incubation on thioglycolate broth for up to 14 days. These findings may reflect the fact that in the majority of our PSI cases presented as early-onset, and local trauma had been the main reason for primary shoulder arthroplasty. Hsieh et al., identified 15% of GNB-PJI after THA and TKA, occurring mainly in the early postoperative period, in which P. aeruginosa was the principal pathogen.19 Reasons for the high frequency of GNB-PSI in our study may include: (1) previous use of broad-spectrum systemic antibiotics such as cephalosporin in trauma patients may have selected more naturally resistant pathogens; (2) since 2011 we started applying sonication culture method for the microbial diagnosis of PJI, thus increasing microbial identification of biofilm-forming sessile pathogens. The presence of S. aureus and S. epidermidis in a quarter of our PSI patients was not surprising, in contrast to the 12.5% detection of Enterococcus faecalis. Much like GNB, enterococci are more commonly associated with early postoperative PJI and as part of polymicrobial infection.10 Since previous studies have associated the P. acnes with PSI,13,24 we have then applied sonication cultures for the microbial diagnosis of different orthopedic implant-associated infections, and prolonged the culture incubation period to 14 days. So far, we have isolated many fastidious and difficult-to-grow bacteria, but not P. acnes.25 Unfortunately, we have been unable to understand why P. acnes shows no growth after plating sonication fluid and tissue samples onto solid culture media and liquid broth under anaerobic condition, and incubating for at least 14 days. Perhaps, its growth may be hampered by the concomitant presence of others pathogens on polymicrobial infections.12 As previously speculated by Singh et al., we also believe that many of the culture-negative results on clinically diagnosed PSI cases would have been caused by P. acnes.7
We are aware that our study has several important limitations, of course due to its retrospective design and a small number of PSI cases (type II error), thus limiting the performance of multivariate analysis to many important associations with PSI such as presence of hematoma and type of fracture. Interpretation by readers of odds ratio calculation using only binominal logistic regression should be made with caution, because it may overestimate the true effect if the variables analyzed are common. The study was carried out in a large urban public teaching center located in a developing country crowded mega-city which offers a specialized orthopedic care for the local population. Studies addressing PSI risk factors among different populations may not reproduce these results, thus the generalizability of our conclusions should be seen with caution. On the other hand, one important strength of our study is that we performed an active surveillance among all subjects submitted to HA and TSA for at least two years after surgery. Another strength was the large number of trauma patients included in the analysis, thus generating a good epidemiological data among this frequent reason for shoulder arthroplasty.
Despite these limitations, our study revealed higher rates of PSI after HA and TSA, estimated at 9.5% over a 25-year period. PSI was mainly associated with an underlying diagnosis of local trauma, and on multivariate analysis, only ASA grade three or higher was associated with increased risk of PSI. Conversely, controlling for individual patient comorbidity, we found no increased association with PSI. Gram-negative bacilli, especially P. aeruginosa was an important cause of infection and P. acnes was neither detected in periprosthetic tissues nor on sonication fluid cultures. Since 2013, PSI rates after shoulder arthroplasty have reduced dramatically in our center, by applying infection control measures especially on trauma patients requiring HA or PSA, which improved the quality of care. Prospective studies including larger number of patients are needed to examine potential risk factor for PSI after HA and TSA.
Conflicts of interestThe authors declare no conflicts of interest.
We thank Rogério Ruscitto do Prado for his support in statistical analysis.