The presence of Streptococcus agalactiae (GBS) in the maternal genital tract is known to be responsible for significant neonatal morbidity and mortality rates, but it is usually asymptomatic. Maternal screening during pregnancy through the culture of vaginal and rectal secretions collected between 35 and 37 weeks of gestation allows the introduction of therapeutic interventions in a timely manner, reducing the frequency and severity of early-onset neonatal sepsis.1,2 Many countries have reduced morbidity and mortality rates from S. agalactiae infection by adopting universal screening at 35–37 weeks of gestation, and intrapartum antibiotic prophylaxis.3–5
A cross-sectional study was conducted between August and December 2011 to estimate the prevalence of streptococcal colonization in pregnant women in the third trimester of pregnancy and identify the factors potentially associated with colonization. Participants were recruited among consenting women at 35–37 weeks of gestation, attending antenatal clinics in the city of Tubarão, Brazil. A questionnaire was administered asking about socioeconomic status, and clinical and obstetrical data of current and past pregnancies. It also asked questions related to sexual behavior of pregnant women. Vaginal and anorectal secretion samples were collected, and all culture tests were performed at the same clinical laboratory. A culture method is still considered the gold standard of screening for bacterial colonization, being extremely effective and used by most countries, including the most developed.
The data were entered into Epidata version 3.1 and the SPSS software, version 17.0, was used to perform statistical analysis. The study included 118 pregnant women.
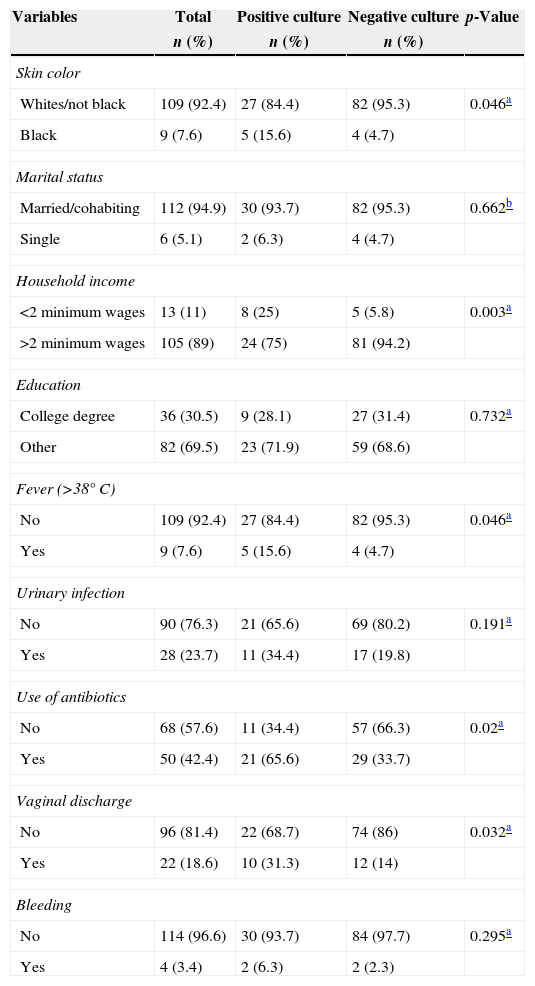
Findings in this study revealed that about one in four women were colonized with GBS, which is considered a high prevalence.2–4 Statistically significant differences were found in this study between colonization with GBS and factors such as black skin color, low household income, fever, antibiotic use and leukorrhea during current pregnancy, prolonged labor in a past pregnancy and multiple sexual partners. Although this was a cross-sectional study, these variables could be considered as risk factors associated with high prevalence of GBS colonization. There was no clear association between marital status, education level, and high rates of streptococcal colonization, even though less educated, unmarried pregnant women had a slightly higher prevalence than their counterparts (Table 1).
Correlation between GBS culture results, demographic and obstetric characteristics of current pregnancy.
| Variables | Total | Positive culture | Negative culture | p-Value |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Skin color | ||||
| Whites/not black | 109 (92.4) | 27 (84.4) | 82 (95.3) | 0.046a |
| Black | 9 (7.6) | 5 (15.6) | 4 (4.7) | |
| Marital status | ||||
| Married/cohabiting | 112 (94.9) | 30 (93.7) | 82 (95.3) | 0.662b |
| Single | 6 (5.1) | 2 (6.3) | 4 (4.7) | |
| Household income | ||||
| <2 minimum wages | 13 (11) | 8 (25) | 5 (5.8) | 0.003a |
| >2 minimum wages | 105 (89) | 24 (75) | 81 (94.2) | |
| Education | ||||
| College degree | 36 (30.5) | 9 (28.1) | 27 (31.4) | 0.732a |
| Other | 82 (69.5) | 23 (71.9) | 59 (68.6) | |
| Fever (>38°C) | ||||
| No | 109 (92.4) | 27 (84.4) | 82 (95.3) | 0.046a |
| Yes | 9 (7.6) | 5 (15.6) | 4 (4.7) | |
| Urinary infection | ||||
| No | 90 (76.3) | 21 (65.6) | 69 (80.2) | 0.191a |
| Yes | 28 (23.7) | 11 (34.4) | 17 (19.8) | |
| Use of antibiotics | ||||
| No | 68 (57.6) | 11 (34.4) | 57 (66.3) | 0.02a |
| Yes | 50 (42.4) | 21 (65.6) | 29 (33.7) | |
| Vaginal discharge | ||||
| No | 96 (81.4) | 22 (68.7) | 74 (86) | 0.032a |
| Yes | 22 (18.6) | 10 (31.3) | 12 (14) | |
| Bleeding | ||||
| No | 114 (96.6) | 30 (93.7) | 84 (97.7) | 0.295a |
| Yes | 4 (3.4) | 2 (6.3) | 2 (2.3) | |
These findings suggest the need for the physicians to adopt a routine prenatal isolation of the micro-organism in culture tests, since knowledge of the prevalence of GBS colonization in pregnant women, and the most significant risk factors, is an important step toward the adoption of intrapartum antibiotic prophylaxis, which can significantly reduce the complications resulting from GBS colonization.
Conflicts of interestThe authors declare no conflicts of interest.