During the past decade, studies on the composition of human microbiota and its relation to the host became one of the most explored subjects of the medical literature. The development of high-throughput molecular technologies allowed a deeper characterization of human microbiota and a better understanding of its relationship with health and disease. Changes in human habits including wide use of antimicrobials can result in dysregulation of host–microbiome homeostasis, with multiple consequences. The purpose of this review is to highlight the most important evidence in the literature of host–microbiome interactions and illustrate how these intriguing relations may lead to new treatment and prevention strategies.
The term microbiota refers to an abundant and diverse population of microorganisms such as bacteria and fungi that reside on body sites, with the highest concentration of these organisms found in the gastrointestinal tract. Indeed, humans harbor a complex community of microorganisms that outnumbers human cells by tenfold.1
Standard culture techniques are limited to fully characterize microorganisms within the microbiota, but nowadays, modern molecular techniques termed metagenomics are available to allow deep characterization of the microbiota of the nasal mucosa, oropharynx, skin, urogenital sites, and lower intestine. These methods rely on polymerase chain reaction amplification of 16S ribosomal RNA-encoding genes of the microbiota, followed by DNA sequencing.2
Projects such as the Human Microbiome Project3 have already done much to define the variability in the microbiota from different body sites and in the microbiomes both within the same human subject and among different subjects. By applying metagenomics, it is estimated that the human lower intestinal microbiota contains at least 1800 genera and 15,000–36,000 species, most of which have never been successfully cultured and the majority of them are classified within Firmicutes and Bacteroidetes phyla.4
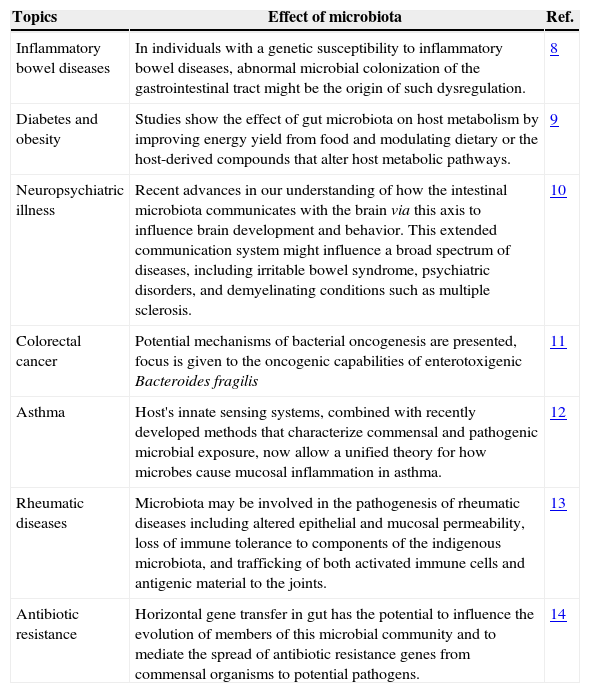
The human intestinal microbiota matures over the first year of life and has substantial and continuous effects on human health and physiological development, including dietary and nutritional processing,5 prevention of pathogen invasion,6 and immune system maturation (Table 1).7
Reviews addressing diseases and biologycal phenomena related to human microbiome.
| Topics | Effect of microbiota | Ref. |
|---|---|---|
| Inflammatory bowel diseases | In individuals with a genetic susceptibility to inflammatory bowel diseases, abnormal microbial colonization of the gastrointestinal tract might be the origin of such dysregulation. | 8 |
| Diabetes and obesity | Studies show the effect of gut microbiota on host metabolism by improving energy yield from food and modulating dietary or the host-derived compounds that alter host metabolic pathways. | 9 |
| Neuropsychiatric illness | Recent advances in our understanding of how the intestinal microbiota communicates with the brain via this axis to influence brain development and behavior. This extended communication system might influence a broad spectrum of diseases, including irritable bowel syndrome, psychiatric disorders, and demyelinating conditions such as multiple sclerosis. | 10 |
| Colorectal cancer | Potential mechanisms of bacterial oncogenesis are presented, focus is given to the oncogenic capabilities of enterotoxigenic Bacteroides fragilis | 11 |
| Asthma | Host's innate sensing systems, combined with recently developed methods that characterize commensal and pathogenic microbial exposure, now allow a unified theory for how microbes cause mucosal inflammation in asthma. | 12 |
| Rheumatic diseases | Microbiota may be involved in the pathogenesis of rheumatic diseases including altered epithelial and mucosal permeability, loss of immune tolerance to components of the indigenous microbiota, and trafficking of both activated immune cells and antigenic material to the joints. | 13 |
| Antibiotic resistance | Horizontal gene transfer in gut has the potential to influence the evolution of members of this microbial community and to mediate the spread of antibiotic resistance genes from commensal organisms to potential pathogens. | 14 |
Human behavior influences the composition of microbiota and its continuous changes may be responsible for the modification of the ancient microbiota. Some authors believe that diseases succeed and fail in response to mankind's advances. The appearance and disappearance of infectious and chronic diseases might be related to changes in human ecology, resulting in changes in the microbes that populate our bodies.15
Human civilizations experienced many transformations, as improvement in sanitization that was implemented to reduce transmission of infections. In order to provide food for an increasing population, food production incorporated new strategies, such as extensive use of pesticides, antibiotics, and hormones in animals and agriculture.15,16 The increasing antibiotic use in humans and farming is one of the most important fact that leads to a rapid and sometimes irreversible change on human microbiota.17
Helicobacter pylori is an example of an ancient human microbiota member that presented a dramatic change. H. pylori has been extensively investigated by Dr. Blaser et al. who observed that this bacterium was progressively disappearing during the twentieth century, from individuals in developed countries, with secondary alterations in gastric secretory, hormonal and immune physiology.18
This bacterium is thought to be related to peptic ulcer and gastric cancer but the sustained acidity in H. pylori-negative hosts increases the risk of gastroesophageal reflux disease and its consequences, including esophageal and gastric cardia adenocarcinomas.19
The stomach also produces adipokine hormones known as ghrelin and leptin, both with multiple roles in energy homeostasis. Patients under antibiotic treatment that eliminated H. pylori had increased circulating ghrelin levels.20 There is a hypothesis that in recent generations of children growing up in developed countries, there has been little gastric H. pylori-mediated regulation of those adipokines at the developmental stage, when long-term adiposity is being programmed. It is possible that the disappearance of H. pylori might be contributing to the current epidemics of early-life obesity, type 2 diabetes and related metabolic syndromes.
Gordon et al. were also interested in studying the relationship between obesity and microbiome. They analyzed fecal samples of lean and obese twins and observed that obesity was associated with phylum-level changes in the microbiota, reduced bacterial diversity and altered representation of bacterial genes, and metabolic pathways related to glycoside hydrolases.21 Cardiovascular risk also has influence on intestinal microbial metabolism, as shown by Hazen et al., who observed an increase in a proatherosclerotic metabolite, trimethylamine-N-oxide (TMAO), in healthy participants after the suppression of intestinal microbiota with oral broad-spectrum antibiotics.22
Stimulation of the immune system is another important function of the microbiome where the disruption of immune homeostasis may be associated with inflammatory and atopic diseases.23 Epidemiological studies show that H. pylori-positive individuals have lower risk of childhood asthma, allergic rhinitis and skin allergies than those without H. pylori.24H. pylori-positive stomach has a rich population of immune cells which regulates immune functions. Stomachs of H. pylori-negative hosts have much lower number of these cells, which have systemic, as well as local activities.25 The increase in prevalence of immunological disorders (both of autoimmune and of atopic origin) in the developed world has been associated with changes in microbiome, which gave support to the hygiene hypothesis.26
Microbiome and infectious diseasesThe relationship between the microbiome and infectious diseases has yet to be determined. There is a lot of interest regarding the effect of antibiotic therapy, as antibiotic treatment to prevent or eradicate a pathogenic infection also impacts the composition of the commensal microbiota.
Combined antibiotic therapy with clarithromycin and metronidazole reduced bacterial diversity of healthy subjects in short and long terms.27 A decline trend was observed in Actinobacteria in both throat and feces immediately after treatment. The microbiota remained perturbed in some cases for up to four years post treatment.27 The effect of two courses of ciprofloxacin therapy was analyzed by another study. A profound and rapid shift in community composition occurred within three to four days of drug initiation, with a loss of bacterial diversity. One week after the end of each course, communities returned incompletely to their initial state.28
The consequences of antibiotic therapy might be difficult to understand as the microorganisms that are affected may not be those that are directly targeted by the antibiotic. A complex network of co-dependence exists among members of the microbiota, driven by different ways. One intriguing interaction was described by Hogan et al.29 that described a quorum sensing molecule (3-oxo-C12 homoserine lactone), produced by Pseudomonas aeruginosa, that inhibits Candida albicans filamentation and its virulence in vitro.
The microbiota has also protective functions. A mouse model for S. typhimurium diarrhea was used to study the role of microbiota and secretory antibodies (sIgA). When exposed o infection, mice that harbor a low complexity gut flora, lack S. typhimurium colonization resistance and develop a normal sIgA response, but fail to clear it from the gut lumen. In these mice, pathogen clearance was achieved by transferring a normal complex microbiota. This study was able to determinate the capacity of microbiota to confer colonization resistance and to mediate pathogen clearance in primary infections, despite sIgA.30
Clostridium difficile-associated diarrhea (CDAD) is possibly one of the most important examples in vivo on how antibiotics affect the resident microbial ecosystem patient health. Endogenous microbial inhabitants provide colonization resistance to infection by other microbes, most notably C. difficile. Until now the therapeutic option for CDAD relies on antibiotic treatment with vancomycin or metronidazole, but this approach was associated with depletion of host microbiota and recurrence of symptoms in 35% of patients.31 Transplantation of indigenous microbiota was tested as an alternative treatment to restore the microbiota of a patient with CDAD. Not surprising, the intestinal microbiota transplantation approach resulted in resolution rate of 94%, statistically superior to vancomycin-containing regimens (p<0.01).32
Use of probiotic is an intervention that seeks the restoration of the beneficial microbiota. Strategies are being implemented following antibiotic therapy in infants with necrotizing enterocolitis (NEC),33 as well as in individuals being treated for antibiotic associated diarrhea,34 and bacterial vaginosis.35
Understanding the importance of microbiome is also critical given the huge number of microorganisms in this ecosystem, and the possibility of gene transfer between species. Transfer of resistance genes may occur through horizontal gene transfer (HGT) from commensal bacteria to opportunistic pathogens, as previously described CTX-M extended-spectrum beta-lactamase (ESBL) resistance genes, which originate from Kluyvera sp.36 Using functional metagenomic methods, Sommer et al.37 studied individuals after antibiotic treatment and found clones conferring resistance to 13 different antibiotics and enabled the discovery of 95 unique inserts containing functional antibiotic resistance genes. The majority of these genes were evolutionarily distant from known resistance genes, including 10 previously unidentified beta-lactamase gene families.
Because of the harmful effects of antibiotics on the commensal microbiota, alternative therapies are under investigation, as antimicrobial peptides that have potential antibiotic adjunctive action. For instance, a reduced production of the antimicrobial peptide REG3γ was related to an increased colonization by vancomycin-resistant Enterococcus (VRE) in mice. This was a consequence of depleted microbial signals38 in activating Toll-Like Receptors (TLR). This mechanism seems to be involved in bacterial-mediated protection from diseases, including VRE, suggesting that TLR agonists could be administered during antibiotic therapy to help restore immune homeostasis, specifically REG3γ expression, drastically reducing colonization by VRE.39
The challenge of efficient control strategies for multidrug resistant organisms (MDROs) brought the attention for the hypothesis that restoring and maintaining the commensal microbiome may be a key to prevent MDRO colonization and infection.40 Conversely, a comprehensive antimicrobial stewardship program focusing the prevention of MDRO emergence is needed. In an attempt to identify antibiotics that promote KPC colonization, Perez et al.41 evaluated whether antibiotics promote colonization by KPC-producing Klebsiella pneumonia (KPC-Kp). They found that those antibiotics that fully suppress anaerobes and bacteroides (i.e. tigecycline, clindamycin and piperacillin-tazobactam) promoted significant colonization by KPC-Kp, whereas agents that did not suppress total anaerobes or bacteroides (i.e., ertapenem, ciprofloxacin and cefepime) did not.41
With an increasing number of studies demonstrating that antibiotics have detrimental effects on the host health and on host colonization there is urgent need to develop treatments targeting specific pathogens without changing the indigenous microbiota. For this, a better understanding on microbial cross-talking is essential. Most of the studies are still experimental and remain to be validated, but they hold substantial promise as adjunct therapies to antibiotics in a promising future.
Conflicts of interestThe authors declare no conflicts of interest.