There are limited data regarding prevalence of Chlamydia trachomatis infection among northern Brazilian pregnant women.
ObjectiveThe purpose of this study was to estimate the prevalence of chlamydial infection among pregnant women in their third trimester and to determine the repercussion of this infection on their offspring.
MethodsIn the first phase of this study 100 pregnant women receiving prenatal care in a local public university hospital were examined to assess the prevalence of genital C. trachomatis infection by polymerase chain reaction technique. In the second phase, 88 pregnant women were prospectively evaluated for premature rupture of membranes, puerperal consequences associated with chlamydial infection, and neonates were checked for low-birth weight.
ResultsThe prevalence rate of chlamydial infection was 11%, and 72.7% of the positive participants were predominantly less than 30 years of age (p=0.1319). A total of 36.4% of the participants had premature rupture of membranes (p=0.9998). Neither low-birth weight infants nor preterm delivery were observed. A cohort of 16 newborn babies were followed-up up to 60 days of life to ascertain outcome: 50% had respiratory symptoms. Neonates born to infected mothers had a higher risk to develop respiratory symptoms in the first 60 days of life.
ConclusionThe scarcity of data about the effects of chlamydial infection on pregnancy and neonatal outcomes justified this study. Diagnosing and treating chlamydial infection during the third trimester of pregnancy may prevent neonate infection. Therefore, preventive screening should be seen as a priority for early detection of asymptomatic C. trachomatis infection as part of local public health strategies.
Chlamydia trachomatis infection is nowadays considered the most frequent sexually transmitted disease (STD) in the developed world. The World Health Organization (WHO) estimate that annually nearly 100 million new cases occur around the world.1 Studies show that chlamydial infections is the commonest transmitted bacterial disease in European countries and in the United States with more than 2.8 million new cases estimated to occur each year.2 During 2009, more than 1.2 million cases of chlamydial infection were reported to Centers for Diseases Control (CDC). Prevalence of chlamydial infection was 6.8% among sexually active females aged 14–19 years.3
According to the CDC, C. trachomatis infection among pregnant women in the United States is the third main cause of STD, with bacterial vaginosis and herpes simplex virus 2 being first and second, respectively.3
In Brazil, according to STDs epidemiologic studies in specific groups of women that attended gynecology, family planning, and prenatal clinics showed a prevalence of 2.1–27.1% for genital infection by C. trachomatis.4 In the Amazon region, there is little data about the actual prevalence of chlamydial infections. Only AIDS, HIV in pregnant women and children, syphilis in pregnant women, and congenital syphilis have compulsory notification.5
In Manaus, the capital city of the state of Amazonas (AM), Brazil, Alencar et al. established a 27.1% prevalence of chlamydial infection by direct immunofluorescence technique.6 On the other hand, Santos et al. and de Lima Freitas found 20.6% and 52.8% of sexually active women and infertile women, respectively, to be positive for Chlamydia using PCR technique.7,8
Many studies have provided estimates of chlamydial infection in pregnant women throughout the world. C. trachomatis disease, considered to be a treatable condition, continues to infect massive populations and the exact magnitude of this is still unknown.9,10 Prevalence rates among pregnant women vary enormously around the world.9,11 Jalil et al. conducted a study to estimate the prevalence of C. trachomatis infection in pregnant women from six Brazilian cities and found 9.4% using hybrid capture technique.12 On the other hand, in Fortaleza, the capital city of Ceará, Brazil, Martins et al. found a prevalence of 11% in pregnant women by PCR technique.13
Uncomplicated C. trachomatis cervicitis in pregnancy may result in sporadic and recurrent miscarriage, preterm labor, premature rupture of membranes, low birth weight and postpartum endometritis.14
Maternal C. trachomatis infections have been associated with increased morbidity in newborns and infants up to three months of age. Approximately two thirds of neonates born vaginally to infected mothers will become infected at birth.15 These infections can result in conjunctivitis, otitis media, pharyngitis and pneumonia in the newborn. Moreover, neonatal infection with C. trachomatis can cause long-term sequelae such as chronic obstructive pulmonary disease.14
The primary aim of this study was to assess the prevalence of C. trachomatis in the final trimester among pregnant women who attended the low-risk prenatal clinic of a public health university hospital in Manaus, Amazonas, Brazil. In Manaus, there are no studies related to vertical transmission of C. trachomatis, so the secondary aim of this study was to ascertain possible neonatal implications associated to maternal C. trachomatis infection. Moreover, the purpose of this study was to evaluate C. trachomatis infection rate associated with socio-economic status of the participants enrolled in the study, adverse pregnancy outcomes associated with miscarriage, preterm labor, premature rupture of membranes and low birth weight.
Materials and methodsEndocervical samples were collected from 100 pregnant women receiving care at the low-risk prenatal clinic of Dona Francisca Mendes University Hospital in Manaus, Amazonas, Brazil, between January and June 2005. The first phase of this study was a cross-sectional evaluation of the prevalence of Chlamydia infection in the final trimester of pregnancy (as of 29 weeks of gestation). In the second phase of this study, pregnant women were prospectively followed to evaluate postpartum effects of this infection as well as upon their neonates up to sixty (60) days after birth.
This study was approved by the Human Research Ethics Committee at the Federal University of Amazonas and performed in accordance with the Declaration of Helsinki.
Assessment of patientsPregnant women included in this study answered a standardized questionnaire to collect information on age, marital status and medical history, number of lifetime sexual partners and socio-economic status. Family income and education level were the criteria used to determine socio-economic status. Patients were excluded if the gestational age was less than 28 weeks and six days, had infections requiring antibiotic therapy or a history of antibiotic use in the preceding 30 days. In addition, pregnant women who had sexual intercourse in the past 72h, history of vaginal bleeding or who used vaginal cream, suspected premature rupture of the membranes, and a diagnosis of placenta previa were also excluded.
In the first phase of the study all participants were contacted by telephone so that the researchers could collect information about their maternity admission and start the second phase of the study. During the second phase of the study 88 pregnant women who met the eligibility criteria had their delivery checked and were followed-up for 60 days after giving birth. Of a total of 100 participants in the first phase of the study 12 were excluded from the study: four could not be contacted and eight due to insufficient follow-up time (less than 40 days of postpartum).
A cohort study was carried out in 88 newborns who were evaluated in the first 24h and monitored thereafter every 15 days up to 60 days of life. However, 12 neonates were excluded due to loss of contact (four) and to follow-up time less than 60 days of life (eight). Moreover, one case of stillbirth occurred. Subsequent evaluations were conducted by telephone and if some ocular discharge or respiratory symptoms appeared in the neonate a clinical evaluation was requested. Furthermore, patient's complaints, clinical evaluation and physical exams were registered in the questionnaire and entered in Epi-Info data bank.
Collection of the samplesEndocervical material for smears was collected using a cyto-brush and subsequently re-suspended in 400μL of TE (10mM Tris–HCl pH 8.0 and 1mM EDTA) and stored at −20° C until DNA extraction.
Preparation of the samples for PCREach sample was supplemented with 400μL TPK solution [TE, 20% Tween, 10mg/mL proteinase K], followed by incubation at 56° C for 1h and then boiling for 10min. DNA from samples that contained blood was extracted by phenol/chloroform.
PCR amplification of C. trachomatis DNA plasmidThe KL1 (5′TCCGGAGCGAGTTACGAAGA3′) and KL2 (3′AATCAATGCCCGGGATTGGT5′) primers were used to amplify a 241bp fragment of the C. trachomatis DNA plasmid by PCR. The PCR consisted of 5.0μL of DNA; 5.0μL of 10× PCR buffer; 2.0μL of 50mM MgSO4; 1.0μL of 10.0mM dNTP; 5.0μL of each primer (5pmol/μL); 0.2μL of 5U/μL Taq DNA polymerase; and 26.8μL Milli-Q water to complete the 50μL volume. The amplification was performed in a PXE 0.2 Thermal Cycler (Thermo Electron Corporation), using the following program with 40 amplification cycles: pre-denaturing at 94°C for 30s, denaturation at 94°C for 30s, primer annealing at 64°C for 30s and primer extension at 68°C for 2min, followed by a final extension at 68°C for 5min.
DNA sequencingTo confirm the presence of 241bp PCR products, we sequenced positive samples of C. trachomatis with the MegaBACE 1000 DNA Analysis System. The amplified products were digested with EXO and SAP enzymes, followed by incubation at 37°C and 80°C for 1h and 30min, respectively. The purified products were sequenced using DYEnamic ET DYE Terminator Cycle Sequencing kit for MegaBace from GE Healthcare Lifesciences according to manufacturer's protocol. The sequencing reactions were separated and analyzed on the automatic sequencer.
Statistical analysisStatistical analyses were performed to calculate the absolute and relative frequency distributions for qualitative variables; as well as median and standard deviation values for quantitative variables. The data were analyzed to evaluate the association between the categorical variables and PCR results using the Pearson χ2 test with the Yates correction or Fisher's exact test. To analyze the risk factors of the neonates relative risks (RR) were calculated. Student's t-test was used to compare means of normally distributed data. To estimate the prevalence of C. trachomatis in pregnant women a 95% confidence interval [CI] was calculated. Throughout this study, p<0.05 was considered significant. Statistical analysis was performed using the Epi-Info version 3.3 software for Windows, developed and distributed by CDC, Atlanta, GA, USA.
ResultsPhase I – studyOut of 100 patients 11 (11.0%) were C. trachomatis-positive by PCR. The mean age of PCR-positive patients was 23.5 years with a standard deviation of ±4.5 years.
Although we assessed associations between C. trachomatis infection with family income (45.5%) and their educational level (45.5%), no statistically significant association could be found.
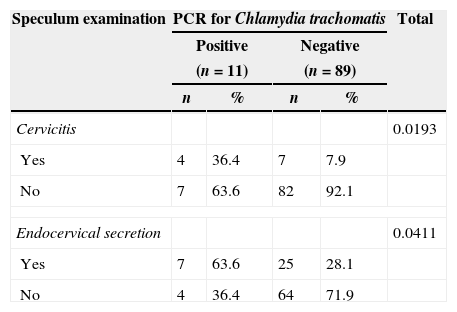
Endocervical secretion and cervicitis were observed in 63.6% and 36.4%, respectively, among those women positive for C. trachomatis infection. Both endocervical secretion and cervicitis were significantly associated with C. trachomatis infection (p=0.0411 and 0.0193, respectively) as shown in Table 1.
Speculum examination according to PCR results for C. trachomatis in pregnant women in Manaus, Amazonas, Brazil.
| Speculum examination | PCR for Chlamydia trachomatis | Total | |||
|---|---|---|---|---|---|
| Positive | Negative | ||||
| (n=11) | (n=89) | ||||
| n | % | n | % | ||
| Cervicitis | 0.0193 | ||||
| Yes | 4 | 36.4 | 7 | 7.9 | |
| No | 7 | 63.6 | 82 | 92.1 | |
| Endocervical secretion | 0.0411 | ||||
| Yes | 7 | 63.6 | 25 | 28.1 | |
| No | 4 | 36.4 | 64 | 71.9 | |
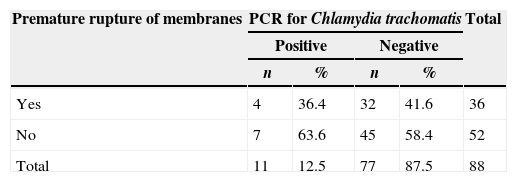
There was no significant association between positivity for C. trachomatis infection and premature rupture of membranes (Table 2). Neither preterm labor (less than 37 weeks gestational age) and nor low-birth weight (weight less than 2500g/5.5 pounds) was observed among the PCR-positive women.
Cesarean delivery was indicated for PCR-positive primiparous pregnant woman. Chronic tubal sequelae were assessed by the surgery description. One week after birth a patient was readmitted to the hospital with diagnosis of postnatal endometritis. Another C. trachomatis positive participant gave birth to a stillborn fetus with 34 weeks gestation. After this episode, this patient developed postnatal endometritis.
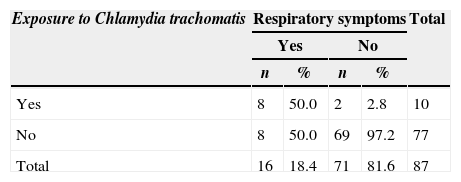
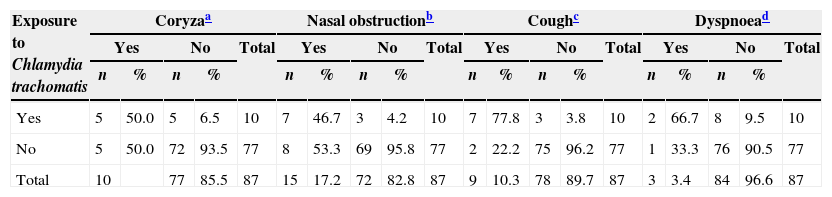
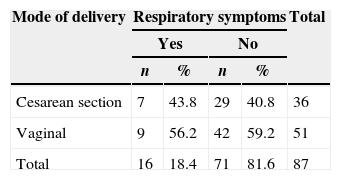
Cohort study of neonatal outcomeOf the 87 newborns, 16 (18.4%) presented respiratory symptoms. Of these newborns, eight (50%) were born to C. trachomatis-positive mothers evidencing a RR of 7.7 (Table 3). Moreover, neonates born to positive mothers were more likely to develop respiratory symptoms such as nasal obstruction (RR=6.7), coryza (RR=7.7), cough (RR=27.0) and dyspnea (RR=15.4) (CI 95%) (Table 4). There was no statistically significant (p=0.8312) association between C. trachomatis infection and type of delivery (cesarean section or vaginal) (Table 5).
Incidence of respiratory symptoms in a cohort of 87 neonates exposed according to maternal Chlamydia trachomatis infection in Manaus, Amazonas, Brazil.
| Exposure to Chlamydia trachomatis | Respiratory symptoms | Total | |||
|---|---|---|---|---|---|
| Yes | No | ||||
| n | % | n | % | ||
| Yes | 8 | 50.0 | 2 | 2.8 | 10 |
| No | 8 | 50.0 | 69 | 97.2 | 77 |
| Total | 16 | 18.4 | 71 | 81.6 | 87 |
RR=7.7; 95% CI (3.7–15.9).
Incidence of nasal obstruction, coryza, cough and dyspnea in a cohort of neonates according to maternal Chlamydia trachomatis infection up to 60 days after birth in Manaus, Amazonas, Brazil.
| Exposure to Chlamydia trachomatis | Coryzaa | Nasal obstructionb | Coughc | Dyspnoead | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Total | Yes | No | Total | Yes | No | Total | Yes | No | Total | |||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |||||
| Yes | 5 | 50.0 | 5 | 6.5 | 10 | 7 | 46.7 | 3 | 4.2 | 10 | 7 | 77.8 | 3 | 3.8 | 10 | 2 | 66.7 | 8 | 9.5 | 10 |
| No | 5 | 50.0 | 72 | 93.5 | 77 | 8 | 53.3 | 69 | 95.8 | 77 | 2 | 22.2 | 75 | 96.2 | 77 | 1 | 33.3 | 76 | 90.5 | 77 |
| Total | 10 | 77 | 85.5 | 87 | 15 | 17.2 | 72 | 82.8 | 87 | 9 | 10.3 | 78 | 89.7 | 87 | 3 | 3.4 | 84 | 96.6 | 87 | |
Studies show that C. trachomatis infection during pregnancy may lead to serious complications. Epidemiological data suggest that pregnant women may be a specific target group for C. trachomatis screening. Antenatal screening, as recommended by the CDC,3 would be beneficial to decrease morbidity amongst women themselves, but also to prevent vertical (infant) and horizontal (partner) transmission.
Although studies have demonstrated prevalence of C. trachomatis in pregnant women using hybrid capture technique in Brazilian cities,12 we decided to undertake this study using the conventional PCR technique. However, although hybrid capture technique is widely used for the detection of pathogens, it may lack sensitivity in comparison with PCR techniques.16 PCR was the first technique to be developed and because of its ability to amplify specific targets and due to superior sensitivity it remains the most widely used molecular technique.17
The prevalence of C. trachomatis infection in this study was 11.0%. Although Jalil et al.12 found a prevalence of 9.4% among Brazilian pregnant women, the rate identified in this study is in agreement with the findings of Martins et al.13 (11.0%). However, as mentioned above there were no data on C. trachomatis infection among pregnant women in the city of Manaus before this study. The main goal of this study was to better understand the epidemiology of Chlamydia infection in this Brazilian city. As compared to other C. trachomatis infection prevalence studies conducted in Brazil, it is possible that the prevalence rate identified in this study is associated with the population characteristic. Although we found that the majority (45.5%) of the participants with PCR-positive results had a low family income, in addition to low educational level (45.5%), and had no knowledge of the existence of C. trachomatis and its effects on women's reproductive health. A total of 81.8% of PCR-positive C. trachomatis women in this study were married or were living a cohabitating situation. Only one lifetime sexual partner was reported by 90.9% of the women; 72.7% of the PCR-positive patients were under 25 years old. The risk of presenting chlamydial infection is two times higher in under 25 years old women.18 In most of the studies the majority of positive participants were under 25 years old, which is could possibly be explained by the unhealthy lifestyle behavior of this age group, such as unprotected sex.19 These factors may be due to high number of unrecognized infected men which provides a reservoir for spreading the infection to women via sexual contact.20 These findings indicate the need for disseminating information about the risk factors for Chlamydia infection. The following factors may be responsible for the inadequate incorporation of preventive measures by women: low educational level of the population; and lack of screening for Chlamydia infection in the public health system.21 Also, it is possible that the prevalence rate identified in this study is associated with low socio-economic status and low family income of the participants enrolled in this study. Women of low-income groups or of low educational level have no access to screening tests.
Considering that 36.4% of the PCR-positive patients had cervicitis identified at gynecological examination, this is an important clinical finding for women's reproductive health because in certain situations, cervicitis may ensue infection in pregnancy, which may result in preterm labor and neonatal infections. This clinical finding is in agreement with the syndromic approach protocol for vaginal discharge and cervicitis established by CDC.22 Considering that chlamydial infections are usually asymptomatic and therefore difficult to screen, women without such marker would be considered to be at high risk of ascending infection, which may lead to severe complications resulting in tubal damage.23
In this study, we verified a high rate of abortion. In contrast to most studies on the subject, 30 (90.9%) of these participants were negative for C. trachomatis infection. Although various studies state that C. trachomatis may cause abortion in several animal species, endocervical Chlamydia infections may or may not be associated with spontaneous abortion.24,25 This diagnostic accuracy is important because it has the potential to help identifying cases at higher risk for spontaneous abortion.
In this study, we verified a case of a pregnant woman diagnosed with Chlamydia infection developed a stillborn fetus. The putative association with the infection could not be confirm because the fetus was investigated. Andrews et al.26 related a study where chlamydial infection detected at 24-week gestation could be associated with double risk of preterm birth. Yet, infection that was detected at 28-week gestation had no significant effect of preterm birth.
Also, some studies indicate that C. trachomatis is an important etiological agent of endometritis in women with concomitant signs of salpingitis.27 It is possible that cases of postpartum endometritis in this study were due to C. trachomatis infection. Ascending infections of the female genital tract with sexually transmitted agents of the lower genital tract may occur during the postpartum period.28
In this study, 50% of positive C. trachomatis newborns presented respiratory problems. Various studies state that transmission of C. trachomatis from mothers to their newborns usually occurs at the time of delivery with passage of the newborn through the infected endocervix. According to Numazaki et al. and Schaad et al. the possibility of intrauterine infection at late pregnancy has also been reported.29 Our finding showed a relation between C. trachomatis infection and respiratory symptoms. Cough symptoms showed to have an increased risk (RR 27.0) when neonates are born to infected mothers, followed by dyspnea (RR 15.4), coryza (RR 7.7) and nasal obstruction (RR 6.7). Respiratory symptoms were more frequent in neonates born to Chlamydia infected mothers. In addition, in this study, respiratory symptoms such as cough, was the most important symptom found in infants. Therefore, it is clear that clinical findings in this study in neonates born to Chlamydia infected mothers were associated with antenatal chlamydial infection in their mothers. Bébéar and Barbeyrac have also described that untreated infection acquired at birth can persist for months or years.30 Moreover, the role of chlamydial infection resulting in neonatal pneumonia has also been considered. Although mortality associated to neonatal pneumonia caused by chlamydial infection is low, sequelae such as impairment in lung function may be evidenced.14 These findings indicate the great importance of a systematic investigation for this curable STD in pregnant women. This points to the necessity of an important clinical measure to reduce vertical transmission and complications of C. trachomatis infection and other causes of curable STD.
ConclusionOur results demonstrate a true local reality, where women lack information about Chlamydia infection and an awareness of the possibility of gestational, perinatal and neonatal complications. Most of the time, pregnant women who are less privileged in socioeconomic and educational terms are left without any or insufficient medical assistance. It is important to emphasize the need for an equitable distribution of resources in health services. Therefore, it is essential to implement antenatal screening programs in public health service laboratories using the PCR method for detecting Chlamydia infection in this high risk population during the last month of pregnancy.
Conflict of interestThe authors declare no conflict of interest.
The authors like to thank the Federal University of Amazonas and Dona Francisca Mendes University Hospital for all the help received during the development of this work. We are also thankful for Fundação de Amparo à Pesquisa do Estado do Amazonas (FAPEAM), who funded this research.