This was a case–control study to identify prognostic indicators of bacterial meningitis in a reference hospital in Pernambuco/Brazil. The data were collected from charts of 294 patients with bacterial meningitis between January 2000 and December 2004. Variables were grouped in biological, clinical, laboratory and etiologic agent/treatment. Variables selected in each step were grouped and adjusted for age. Two models were created: one containing clinical variables (clinical model) and other containing laboratory variables (laboratory model). In the clinical model the variables associated with death due to bacterial meningitis were dyspnea (p=0.006), evidence of shock (p=0.051), evidence of altered mental state (p=0.000), absence of headache (p=0.008), absence of vomiting (p=0.052), and age ≥40 years old (p=0.013). In the laboratory model, the variables associated with death due to bacterial meningitis were positive blood cultures (p=0.073) and thrombocytopenia (p=0.019). Identification of prognostic indicators soon after admission may allow early specific measures, like admission of patients with higher risk of death to Intensive Care Units.
Bacterial meningitis is a worldwide medical, neurological and, sometimes, neurosurgical emergency.1,2 Most patients with bacterial meningitis present classic signs and symptoms, such as headache, fever, vomiting and neck stiffness. Some patients develop a serious clinical profile, with agitation, torpor, motor disorders, convulsions and even coma.3,4
Studies of prognostic indicators for bacterial meningitis in adults are rare in Brazil. Given the risk of sequelae and death in patients with bacterial meningitis, the identification of prognostic factors on admission to hospital could minimize the occurrence of undesirable events. The aim of this study was to investigate the implications of certain clinical syndromes and laboratory findings at the time of admission to hospital for the prognosis of adult and adolescent patients with bacterial meningitis.
MethodsA case–control study was carried out with all patients aged 13 years and over admitted to a public hospital in Pernambuco/Brazil, Hospital Correia Picanço, between January 2000 and December 2004, with clinical (headache, fever, vomiting, neck stiffness, alterations in consciousness) and laboratory symptoms (liquor cell count>5cells/mm3 and a predominance of polymorphonuclears greater than 50%, irrespective of Gram or culture results) of bacterial meningitis, evolving to death due to the disease or a related cause. The control group consisted of patients aged 13 years and over, with clinical and laboratory diagnosis of bacterial meningitis, who were eventually discharged from the same hospital, during the same time period. The study was approved by the Research Ethics Committee of the Hospital Universitário Oswaldo Cruz (no. 024/2005).
The sample size was calculated on the basis of two previous studies.5,6 The estimated sample was 96 cases and 135 controls.
All patients diagnosed with bacterial meningitis were listed and, once the number of deaths/year (cases) had been identified, the number of controls (patients discharged from hospital) was calculated at a proportion of 1:2. Individuals were selected randomly for the control group stratified by age, proportionate to the number of cases.
Patients were excluded if they had arrived at the Hospital Correia Picanço more than 24h after the commencement of specific treatment (antibiotics); if they had a liquor fistula or one ventricular-peritoneal derivation; or if they had previously undergone neurosurgery.
Patients transferred to other services due to complications whose outcomes (death or discharge from hospital) could not be ascertained, even after active investigation, and those discharged from hospital for non-medical reasons (i.e., those patients who discharged themselves) were considered to be losses.
First, the association of each variable with death from bacterial meningitis was assessed using univariate analysis. The degree of association was expressed as an odds ratio. The sensitivity of the selection of variables for the logistic regression model was established using a cut-off point of p<0.20 in univariate analysis. The statistical significance of the results obtained was assessed using confidence interval of the estimated odds ratios and the chi-squared test, with Yates's correction, where recommended.
The variables initially tested using univariate analysis were: age, sex, place of origin, time of development of symptoms, time elapsed until the first dose of antibiotics, signs and symptoms grouped according to organs or systems affected, evidence of shock (circulatory shock, cyanosis, sweating, pallor, alterations in peripheral tissue perfusion), evidence of altered mental state (reduction in level of consciousness, psychomotor agitation, coma, disorientation, listlessness), evidence relating to meningeal signs (neck stiffness; Kernig's, Brudzinski's, and Lasègue's signs), skin and mucusa alterations (petechiae, ecchymoses, vascular lesions), neurological signs (aphasia, motor dysfunction, anisocoria, strabismus, lip pull, dysarthria), and evidence of infection (fever, myalgia, arthralgia, tachypnea, dyspnea, decline in general state of health, chills, asthenia, dizziness). Some clinical signs that have been most commonly identified as factors determining prognosis in previous studies were evaluated in isolation: vomiting, convulsions, dyspnea, fever, headache and coma; initial liquor cell count; initial glycorrhachia; initial proteinorrhachia; identification of etiological agent by Gram or culture; bacterial isolate (etiological agent) from blood, from liquor or both; hemoglobinemia on admission; leucometry of peripheral blood on admission; platelet count in peripheral blood on admission; initial antibiotic regimen and previous use of antibiotics.
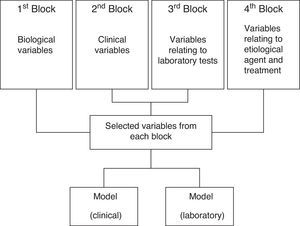
The variables selected were grouped in blocks and introduced into the multiple logistic regression model. Four distinct blocks of variables were created: 1st block: biological variables; 2nd block: clinical variables; 3rd block: variables relating to laboratory tests; 4th block: variables relating to etiological agent and treatment (Fig. 1). At this stage the association was considered statistically significant when p<0.05. The t-test was used for comparison of means. The calculation of the sample and storage and analysis of data were carried out using the EPIINFO 6.04 and SPSS 8.0 for Windows statistics programs. The variables in each block were then adjusted according to others in the bi- or multivariate analysis. The variables with a statistically significant association (p<0.05) identified during each stage were grouped together and then adjusted for the biological variable that was also found to be statistically significant (age group). After multivariate analysis, two distinct final models were created, one containing variables from the 1st and 2nd blocks (the clinical model), and a second containing variables from the 1st and 3rd and 4th blocks (the laboratory model). The association of each variable with the risk of death from bacterial meningitis was measured using the lowest risk group for comparison.
ResultsThe study covered 294 patients at a proportion of one case for two controls (98 cases and 196 controls). Of these, 21 (7.1%) were transferred to other services as a result of complications, and of these, eight (2.7%) died.
Age ranged from 13 to 87 years, with a mean of 30.9 years. In the control group, the mean age was 27.7 years and the median 22, while in the case group age ranged from 14 to 87 years, with a mean age of 37.4 years and a median of 31.5. The risk of death from bacterial meningitis was around three times greater among individuals aged 40 or over (OR 2.78; CI 1.62–4.73; p=0.0002).
Of the 294 patients, 173 were male (58.8%). There was no statistically significant association between sex and death from bacterial meningitis in the sample studied (p>0.05). Neither was there any association between the place of origin of the patient and death from bacterial meningitis, when comparing those from the State capital and the metropolitan region with those from other municipalities in the State.
Bacteria were found in the liquor of 94 patients, with 33.3% (9/27) of cases presenting meningococci compared with 65.7% (44/67) of the control group; with 51.9% (14/27) of the cases presenting pneumococci, compared with 26.9% (18/67) of the control group; staphylococci were isolated in 14.8% (4/27) and 7.5% (5/67) of case and control groups respectively. The proportion of positive hemoculture among the cases was 49.1% (28/57) compared to 19.5% (26/133) in the control group (p<0.0001).
Initial univariate analysis showed no statistically significant association between the variables relating to the time of development of symptoms (time elapsed between the emergence of symptoms and admission to hospital); the type of initial antibiotic regimen employed; previous use of antibiotics; and the time elapsed until the first dose of antibiotics and death due to bacterial meningitis. No statistically significant difference was found between the mean time for the commencement of treatment with antibiotics in case (91.7min) and control groups (98.3min).
The variables age and sex were selected for the 1st block, and, following bivariate analysis, only age was retained in the final model (OR 2.78; CI 1.63–4.74; p=0.0002).
Fig. 1 sums up all the steps in the analysis.
Table 1 shows the results of analysis of the variables in the 2nd block (clinical variables) and death due to bacterial meningitis. Presence of dyspnea, evidence of shock, and alterations in mental state were associated with death due to bacterial meningitis. Likewise, the absence of headache and vomiting was associated with a less favorable prognosis.
Adjusted odds ratio, confidence interval and p-value of the association between death due to bacterial meningitis and dyspnea, evidence of shock, meningeal signs, fever, headache, vomiting, alterations in mental state, coma, and skin and mucosa alterations in 294 patients of the Hospital Correia Picanço between January 2000 and December 2004.
| OR | 95% CI | p-Value | |
|---|---|---|---|
| Dyspnea | |||
| Yes | 4.03 | 1.51–10.76 | 0.0054 |
| No | 1.00 | ||
| Evidence of shock | |||
| Yes | 2.73 | 1.02–7.25 | 0.0444 |
| No | 1.00 | ||
| Headache | |||
| Yes | 1.00 | ||
| No | 5.59 | 1.74–17.96 | 0.0038 |
| Vomiting | |||
| Yes | 1.00 | ||
| No | 1.96 | 1.02–3.77 | 0.0446 |
| Alterations in mental state | |||
| Yes | 3.65 | 2.02–6.58 | 0.0000 |
| No | 1.00 | ||
OR, odds ratio; CI, confidence interval.
Table 2 shows the results of analysis of variables in the 3rd block (laboratory variables) and death due to bacterial meningitis. The mean of cells in liquor was significantly higher in the control group (8054.9cells/mm3) than among cases (5734.0cells/mm3), [p=0.02]. The mean glycorrhachia among cases was 36.8mg/dl compared to 34.6mg/dl (p=0.66) in the control group. No statistically significant association was found between the leucometry and risk of death from bacterial meningitis. Regarding the number of platelets in peripheral blood, a mean of 203,343.28cells/mm3 found in the cases was significantly lower than the 227,878.57cells/mm3 in the control group (p=0.04).
Adjusted odds ratio, confidence interval and p-value of the association between death due to bacterial meningitis and liquor cell count, leucometry in peripheral blood, number of platelets in peripheral blood and proteinorrhachia in 136 patients of the Hospital Correia Picanço between January 2000 and December 2004.
| OR | 95% CI | p-Value | |
|---|---|---|---|
| Hemoculture | |||
| Positive | 2.69 | 1.13–6.39 | 0.0253 |
| Negative | 1.00 | ||
| Liquor cell count | |||
| Up to 2000cells/mm3 | 2.72 | 1.16–6.35 | 0.0211 |
| >2000cells/mm3 | 1.00 | ||
| Platelets in peripheral blood | |||
| <150,000cells/mm3 | 3.22 | 1.36–7.63 | 0.0080 |
| ≥150,000cells/mm3 | 1.00 | ||
| Proteinorrhachia | |||
| ≤40cells/mm3 | 1.00 | ||
| >40cells/mm3 | 4.51 | 0.76–26.75 | 0.0972 |
OR, odds ratio; CI, confidence interval.
The 4th block contained the variables: identification of etiological agent using Gram (Gram positive diplococcus) and the initial antibiotic regimen. After adjustment by bivariate analysis, only the identification of Gram positive diplococcus as the etiological agent of bacterial meningitis was associated with a threefold greater risk of death (Table 3).
Adjusted odds ratio, confidence interval and p-value of the association between death due to bacterial meningitis and identification of the etiological agent by Gram stain (Gram positive diplococcus) and the initial antibiotic regimen in 130 patients of the Hospital Correia Picanço between January 2000 and December 2004.
| OR | 95% CI | p-Value | |
|---|---|---|---|
| Diplococcus | |||
| Gram positive | |||
| Yes | 3.20 | 1.47–6.97 | 0.0062 |
| No | 1.00 | ||
OR, odds ratio; CI, confidence interval.
Analysis of the variables selected from the 1st block (age) and the 2nd block (clinical variables) showed that being aged 40 years or older, the presence of dyspnea, evidence of shock or altered mental state, and the absence of headaches and vomiting were associated with death due to bacterial meningitis (Table 4).
Adjusted odds ratio, confidence interval and p-value of the association between death due to bacterial meningitis and age, dyspnea, evidence of shock, meningeal signs, fever, headache, vomiting, alterations in mental state, coma and skin and the mucosa alterations in 294 patients of the Hospital Correia Picanço between January 2000 and December 2004.
| OR | 95% CI | p-Value | |
|---|---|---|---|
| Dyspnea | |||
| Yes | 3.99 | 1.49–10.67 | 0.0059 |
| No | 1.00 | ||
| Evidence of shock | |||
| Yes | 2.69 | 0.99–7.27 | 0.0511 |
| No | 1.00 | ||
| Headache | |||
| Yes | 1.00 | ||
| No | 4.79 | 1.51–15.20 | 0.0077 |
| Vomiting | |||
| Yes | 1.00 | ||
| No | 1.93 | 0.99–3.77 | 0.0522 |
| Altered mental state | |||
| Yes | 3.35 | 1.84–6.12 | 0.0001 |
| No | 1.00 | ||
| Age | |||
| <40 years old | 1.00 | ||
| ≥40 years old | 2.14 | 1.17–3.92 | 0.0130 |
OR, odds ratio; CI, confidence interval.
After adjustment of the 3rd block (laboratory) variables for age group in the multiple logistic regression model, the variables remaining in the final model were positive hemoculture, cell count in liquor less than 2000cells/mm3, a platelet count in peripheral blood less than 150,000cells/mm3, and age ≥40 years (Table 5).
Adjusted odds ratio, confidence interval and p-value of the association between death due to bacterial meningitis and age, hemoculture result, liquor cell count, platelet count in peripheral blood, and proteinorrhachia in 137 patients of the Hospital Correia Picanço between January 2000 and December 2004.
| OR | 95% CI | p-Value | |
|---|---|---|---|
| Hemoculture | |||
| Positive | 2.80 | 1.16–6.79 | 0.0223 |
| Negative | 1.00 | ||
| Liquor cell count | |||
| Up to 2000cells/mm3 | 2.55 | 1.08–6.01 | 0.0327 |
| >2000cells/mm3 | 1.00 | ||
| Platelets | |||
| <150,000cells/mm3 | 2.65 | 1.11–6.33 | 0.0238 |
| ≥150,000cells/mm3 | 1.00 | ||
| Age | |||
| <40 years old | 1.00 | ||
| ≥40 years old | 3.67 | 1.47–9.16 | 0.0053 |
OR, odds ratio; CI, confidence interval.
Table 6 shows the results of the adjustment of the variables from the 1st (age group), 3rd (laboratory variables) and 4th (etiological agent) blocks, showing that a positive hemoculture and a platelet count less than 150,000cells/mm3 were associated with death.
Adjusted odds ratio, confidence interval and p-value of the association between death due to bacterial meningitis and age, hemoculture result, liquor cell count, platelet count in peripheral blood, and presence of Gram positive diplococcus in 73 patients of the Hospital Correia Picanço between January 2000 and December 2004.
| OR | 95% CI | p-Value | |
|---|---|---|---|
| Hemoculture | |||
| Positive | 2.69 | 0.91–7.90 | 0.0727 |
| Negative | 1.00 | ||
| Platelets | |||
| <150,000cells/mm3 | 2.62 | 1.23–10.60 | 0.0191 |
| ≥150,000cells/mm3 | 1.00 | ||
OR, odds ratio; CI, confidence interval.
After adjustment by multivariate analysis, the variables that remained associated with greater risk of death in patients with bacterial meningitis were age ≥40 years, absence of headache, absence of vomiting, altered mental state, occurrence of dyspnea, evidence of shock, positive hemoculture, and thrombocytopenia.
Age has been associated with higher mortality in other studies with adults, although this variable is categorized differently in different studies. Duran et al.7 in a review of 493 episodes of bacterial meningitis, found higher mortality among those aged ≥60 years, using univariate analysis. van de Beek et al.8 in a prospective study of 696 episodes of bacterial meningitis in individuals aged over 16, reported an association between age ≥42 years and death from bacterial meningitis. In a case–control study examining prognostic factors for adults with bacterial meningitis admitted to an intensive care unit, it was found that age ≥55 years was associated with the development of sequelae and death.9 Another descriptive study of patients with acute bacterial meningitis admitted to an ICU found an association between age ≥50 years and an unfavorable outcome (death or sequelae), using univariate analysis.10 In another series of cases it was found that patients aged over 60 years had a less favorable prognosis.11,12 However, a retrospective study with a series of 255 patients with acute meningicoccal meningitis did not find any age difference between survivors and those patients who died.13 Pedersen et al.14 examining a series of 96 cases of meningitis caused by Staphylococcus aureus, using univariate analysis, likewise did not find age to be a risk factor for death. The same occurred when assessing 202 patients aged ≥16 years, with no association between age and death due to bacterial meningitis after multivariate analysis.6 The greater risk of death among elderly patients may be related to various factors, such as comorbidity, alterations in the immune response or greater likelihood of developing other complications associated with the disease itself or with hospitalization.14
The association between sex and death due to bacterial meningitis was not statistically significant in the present study, in contrast to the findings of other authors.6,15 This may be due to methodological differences. The present study differed from others in using multivariate analysis, which minimizes the effect of confounding variables.
There was no statistically significant association between the time elapsed until the first dose of antibiotics and death from bacterial meningitis in this sample. However, according to Aronin et al.16, delaying commencement of treatment with antibiotics may result in a bad prognosis, especially in the case of patients who have shown marked clinical deterioration. This conflicting result found in the present study may be due to the initiation of antimicrobial treatment within an adequate time period or even the probable low incidence of infection by resistant bacteria.
Some of the clinical findings strongly suggest a diagnosis of bacterial meningitis and are sometimes considered the only criteria for commencement of treatment. These may be the main features for identification of more serious cases. The clinical indicators most frequently described for diagnosis of bacterial meningitis are fever, headache, vomiting, neck stiffness and an altered mental state. In a series of adult cases, fever, neck stiffness and an altered mental state were considered the classic trio of symptoms and their occurrence in 44% of the cases studied was not associated with prognosis. However, when taken together with headache, it can be seen that two of these four signs/symptoms were present in 95% of patients.8 In a series of children and adolescents which considered the classic trio to be fever, neck stiffness and vomiting, it was found that the absence of these three symptoms was associated with a less favorable prognosis.17 The present study did not consider these clinical data together, but noted that the absence of vomiting and headache was associated with a greater risk of death. It may be that the absence of these warning signs delays diagnosis of meningitis and the timely commencement of appropriate treatment.
The present study identified a strong association between an altered mental state and death. Lindvall et al.18 found a high mortality rate (33%) in patients with bacterial meningitis admitted to ICUs who were comatose on admission. Likewise, Vibha et al.,19 in a study covering 380 cases of bacterial meningitis, have reported that a low score on the Glasgow Coma Scale on admission was an independent risk factor for death. Aronin et al.20 have suggested that patients with bacterial meningitis and an altered mental state and/or hypotension and/or convulsions should be kept under closer observation in intensive care. After multivariate analysis, Lu et al.6 found that the initial level of consciousness, appropriate treatment with antibiotics and septic shock were independently associated with mortality after adjustment for other potentially confounding factors.
In the present study, no statistically significant association was found between focal neurological signs and death due to bacterial meningitis, as in some previous studies.7,15 Likewise, in a series of patients with pneumococcal meningitis, no association was found between the presence of focal signs and an adverse outcome.21
One peculiarity of the present study was the fact that dyspnea, taken in isolation, was associated with a less favorable prognosis, since it was found in the most serious cases. This association has not been previously reported in studies involving adults. The occurrence of dyspnea in these patients might be a result of the infection or severe systemic inflammatory response, metabolic acidosis, or even pulmonary injury by the same agent involved in meningitis. All these situations are present in critical patients.
The present study identified evidence of shock as another factor of poor prognosis in bacterial meningitis. Other studies have also reported this finding.12,22–24 Evidence of shock could be a result of sepsis and severe systemic inflammatory response or infection.
As for laboratory findings as prognostic indicators, van de Beek et al.8 have reported a six-fold greater risk of death when the organism causing bacterial meningitis had been identified. The probability of an unfavorable outcome was highest among patients infected with Streptococcus pneumoniae than among those with meningococcal meningitis. In this study, presence of Gram-positive diplococcus was also found to be significantly associated with death, although after adjustments for other laboratory variables, this association was removed from the final model.
Low glycorrhachia on admission has been described by various researchers as a factor associated with a less favorable prognosis, be it death or the development of complications of bacterial meningitis. Curiously, the present study did not find this association as McMillan et al.15 did, This may have been because the sample was too small for investigating this particular variable.
In a retrospective analysis using the 3:1 case–control methodology (n=192), Eisenhut et al.25 observed that in types of bacterial meningitis other than those caused by Neisseria meningitidis and regardless of the duration of symptoms up to diagnosis, glycorrhachia was lower in patients who experienced a reduction in auditory and sensory-neural capacity compared to the controls, the difference being statistically significant.
McMillan et al.15 found a lower liquor cell count and a greater proportion of positive hemocultures among patients who died. A liquor cell count lower than 1000cells/mm3, a positive culture, and a reduction in the number of platelets were associated with death due to bacterial meningitis.8 Tsai et al.22 described thrombocytopenia as a poor prognostic factor in young adults. In our study thrombocytopenia was also associated with higher mortality. In serious infectious diseases, like meningococcal disease and sepsis, thrombocytopenia itself is already a sign of poor prognosis, and may be a reflection of disseminated intravascular coagulation.26
In a prospective series of cases with individuals aged over 16 years diagnosed with pneumococcal meningitis, the diagnostic factors identified were paralysis of cranial nerves, lower leukocyte count in liquor, hyperproteinorrhachia, and an elevated erythrosedimentation rate on multivariate analysis. Glycorrhachia was likewise not associated with death due to bacterial meningitis,27 as in the present study. Many patients in this series did not use corticoids, again as in the present study.
A number of factors differentiate the present study from others that have preceded it like use of a randomly selected control group, as it has not been the case in previous studies with adults. The random selection of controls minimizes selection bias. As this was a retrospective study, some information may have been lost due to incomplete filling of admission forms, even though these were standardized for all the cases admitted, or by the absence of records of baseline laboratory tests results. It may not be possible to completely avoid information bias, but, should this occur, it is probable that it follows the same pattern in both groups, since, at the time of admission to hospital, it is not known which patients will eventually die, making this an non-systematic error.
ConclusionThe prognostic indicators identified in the present study may serve as a tool for clinicians providing initial care for patients with bacterial meningitis. In this way, special attention should be given to patients aged over 40 years, presenting with altered mental state, dyspnea, evidence of shock, and thrombocytopenia. Clinicians should be careful for not delaying the diagnosis of bacterial meningitis in patients with other clinical signs, even in the absence of headache and vomiting, which could result in an unfavorable prognosis, since mortality among adults with bacterial meningitis and the frequency of neurological damage among survivors is still high.
Conflict of interestThe authors declare no conflict of interest.