This is the case of a young male suffering from Austrian syndrome, which is the triad of endocarditis, meningitis, and pneumonia due to invasive S. pneumoniae infection. He reported recurrent fever for six months without any antibiotic treatment, which may have determined the further course of the syndrome. Echocardiography revealed massive native valve endocarditis, and the patient was considered for ultima-ratio cardiac surgery. Intraoperative aspect presented extensive affection of the aortic root with full destruction of aortic valve, mitral valve, and aortomitral continuity. The myocardium showed a phlegmon-like infiltration. Microbiologic testing of intraoperatively collected specimens identified penicillin-sensitive Streptococcus pneumoniae. S. pneumoniae is a very uncommon cause for infective infiltrative endocarditis and is associated with severe clinical courses. Austrian syndrome is even more rare, with only a few reported cases worldwide. In those patients, only early diagnosis, immediate antibiotic treatment, and emergent cardiac surgery can save lives.
A 41-year-old male presented with severe cardiac failure and ensuing cardiogenic shock. He called an emergency service due to a new onset of severe chest pain and was admitted to this chest pain unit.
The patient reported severe nicotine abuse with a cumulative dose of 24 pack years. Furthermore, he was considered to be an alcoholic in remission for four years. No further comorbidities were reported by the patient or his general practitioner. He referred recurrent episodes of fever in the past six months. Both of his children had suffered from scarlet fever. His wife described progressive physical inactivity, aggravated nicotine abuse, and abnormal fatigue with social marginalization for the past two weeks before admission. One week before admission, he went to his general practitioner, who did not indicate any specific therapy or antibiotic treatment.
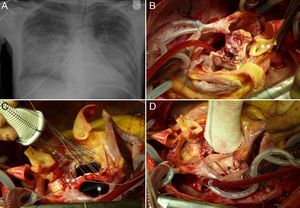
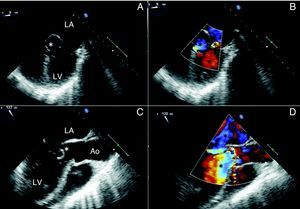
After admission, intubation became urgently necessary due to progressive respiratory failure. Laboratory tests showed significant leucocytosis of 25.6 Gpt/L and concomitant elevated C-reactive protein (CRP) (187 mg/L); creatine kinase (CK) and MB-subtype levels were also high (CK: 5.13 μkat/L and CK-MB 0.94 μkat/L, respectively). Chest X-ray demonstrated extensive bilateral lung infiltrations with concomitant severe cardiac congestion (Fig. 1A) Transthoracic and transesophageal echocardiography revealed fulminant native valve endocarditis with full destruction of the aortic and mitral valves, with a pronounced biphasic flow over both valves. Furthermore, the destruction of the aortomitral continuity led to a relevant shunting from the aortic root to the left atrium. Additionally, the whole aortic root was massively affected by endocarditis and littered with vegetations. (Fig. 2A-D).
(A) Preoperative X-ray of the chest shows severe congestion and concomitant bilateral pneumonic infiltrations. Intraoperative findings are demonstrated in (B-D). (B) Aortic and mitral valve are excised. Remaining are the phlegmone-like alteration to the myocardium(*) and the abscess formation(**) at the former aorto-mitral continuity. The left coronary artery is already isolated (**) (B) Mitral valve prosthesis is already implanted (*). The aortic conduit has to be fixed “valve-to-valve” (**) due to destroyed aorto-mitral continuity. (C, D) Aortic conduit and mitral valve prosthesis are in situ and the left atrium is reconstructed by patch (*).
Preoperative transesophageal echocardiography demonstrating severe damage to the aortic and mitral valve with severe regurgitation (B, D). (A) The extended abscess formation is indexed(*) and (B) duplex shows regurgitation jets(*). (C) The aorto-mitral continuity was totally destroyed(*) and blood was shunting from the aorta to the left atrium (D).
Despite the disastrous cardiac damage and poor clinical condition, the patient was immediately transferred to cardiac surgery for an ultima ratio procedure. Intraoperatively, the previous findings described by the echocardiography were confirmed (Fig. 1B-D). Additionally a massive, phlegmon-like myocardial infiltration was observed. The destroyed aortic valve and severely affected aortic root were replaced by a Bentall procedure. Additionally, the mitral valve was replaced, and the left atrium was reconstructed by patch. During weaning from extracorporal circulation the cardiac skeleton ruptured, originating from the phlegmon-like myocardial infiltration. Thus, the patient died intraoperatively.
Microbiologic testing of the valvar specimens and infected myocardium taken intraoperatively identified penicillin-sensitive S. pneumoniae. The autopsy ruled out any malignant disease. Despite reported alcohol abuse, both liver and spleen presented normal condition. The linings of the brain showed slight hemorraghe and prominent vascular pattern.
DiscussionNative valve endocarditis is still a challenging disease.1–3 In the post-penicillin era, S. pneumoniae causes only 0.9% to 8.0% of all cases of infective endocarditis.4 Thus, S. pneumoniae, causing native valve endocarditis, has become a rarity.5 Worldwide, cases and series are only reported in isolation, with the exception of Denmark, Greenland, and an Inuit population in Alaska, which appear to be associated with a significantly higher incidence.4,6,7 The other cases are usually described in immunocompromised patients, patients suffering from malignancies, or patients who are severely addicted to alcohol.8
Beside this, the clinical rarity of the “Austrian syndrome”, firstly reported by Robert Austrian in 1957, has only been referred in isolated reports.9 It classically describes the triad of meningitis, pneumonia and endocarditis due to invasive pneumococci infection. It is usually associated with males between 40 and 60 years of age, most severely addicted to alcohol, with subsequent splenic dysfunction.
The present case fulfils all criteria for Austrian syndrome: endocarditis, chest X-ray demonstrating preoperative bilateral pneumonic infiltrations, and autopsy revealing prominent vascular patterns and hemorrhage of brain linings. In contrast to the current literature, this patient was considered to be an alcoholic in remission for several years and thus his spleen and liver showed no alterations in autopsy. The infection path might have been the bilateral pneumonia. The question as to why a healthy and immunocompetent young male suffers from a massive pneumococcal pneumonia, must remain unaswered. No factors that could have compromised his immune system were found. Preoperative serologic tests ruled out any hepatitis- or HIV-infection, and the autopsy did not identify any signs of coexisting malignancies. His severe nicotine abuse could be a promoting risk factor; the reported history of scarlet fever of both of his children might only have been a coincidence. Critical to the fatal course was the general practitioner's decision not to initiate antibiotic treatment. One week later, cardiac surgery could only be performed as an ultima ratio procedure. The massive cardiac damage and the phlegmon-like alterations of the myocardium, especially at the aortic root, rendered successful surgery impossible.
Summing up, cases of endocarditis caused by S. pnumoniae are generally associated with severe clinical courses – especially in the presence of late onset of antibiotic treatment or penicillin-resistant pneumococci.9,10 The only chance to survive pneumococcal endocarditis or Austrian syndrome is by early diagnosis and correctly timed antibiotic treatment, as well as early surgery.
Conflict of interestAll authors declare to have no conflict of interest.
Special thanks go to Dr. Stefanie Katzke (Dresden Heart Center, Department for Cardiology, Dresden, Germany) for providing excellent echocardiography and Dr. Uwe Schmidt (Institute for Forensic Medicine at Medical Faculty “Carl Gustav Carus” of Dresden Technical University, Dresden, Germany) for sharing information and giving helpful advice concerning the results of the autopsy.