Many interventions demonstrate success in adapting the duration of intravenous antibiotic therapy, but few studies have been conducted in developing countries. The aim of this study was to evaluate the effectiveness of an intervention in the induction of early discontinuation of intravenous antimicrobial therapy and/or its switch to oral therapy. The study employed a before–after intervention design that consisted of displaying a message in the computerized prescription on the third day and suspension of the prescription on the fifth day of intravenous antimicrobial therapy. A total of 465 patients were followed during the control period (CP) and 440 in the intervention period (IP). The intravenous therapy was switched to oral therapy for 11 (2.4%) patients during the CP and 25 (5.7%) in the IP (p=0.011), and was discontinued for 82 (17.6%) patients during the CP and 106 (24.1%) in the IP (p=0.017). During the IP there was a significant increase of patients who had their antimicrobial treatment discontinued before the seventh day of intravenous treatment, 37.40% (49/131) in the IP and 16.13% (15/93) in the CP (p=0.0005). The duration of intravenous antimicrobial therapy decreased by one day, but it was not significant (p=0.136). It is concluded that the proposed intervention is effective in promoting the early discontinuation of antimicrobial treatment and/or switch to oral therapy. As long as a computerized system for prescription already exists, it is easy and inexpensive to be implemented, especially in hospitals in developing countries.
Apart from causing therapeutic injury and unnecessary toxicity to the patient, the frequent use of inappropriate antimicrobials found in hospitals1–5 generates increased costs and has a great impact on bacterial resistance.6 The implementation of programs aiming to improve the use of antibiotics in hospitals is widely recommended, especially in developing countries.7 However, problems such as scarcity of financial resources and poor infrastructure, deficiency of specialized training, lack of control over the supply and quality of antibiotics, poor hygiene, overcrowding, and cultural habits of physicians and patients hinder the implementation of these programs in developing countries.8,9
In Brazil and other developing countries, the availability and use of antimicrobials are poorly controlled, which further aggravates the problem of bacterial resistance.10 On the other hand, because the public Unified Health System (SUS – Sistema Unificado de Saúde) is universal and free, health authorities are concerned with the proper use of antibiotics.11–13
Reassessment of antimicrobial therapy by the third day is a recommended measure in antimicrobial stewardship. At this time, the identification of microorganisms and their susceptibility allow targeted therapy, and clinical evaluation of the patient may lead to discontinuation, change in therapy duration, and/or switch to oral therapy.14–17 Doctors have often ignored this revaluation due to several factors such as time constraint, change of the physician responsible for the patient during the first days of hospitalization, reluctance to change the empirical therapy in a patient who has shown satisfactory improvement, or even due to poor education.18
When correctly recommended, the switch from intravenous to oral therapy reduces the potential for complications due to the use of intravenous devices, the length of hospital stay, and hospital costs with the treatment.19,20Among the criteria for switching to oral therapy are improvement of clinical and hemodynamic status, ability to ingest drugs, and normal gastrointestinal function.21–23
A wide range of interventions with contributions by clinical pharmacists is described in the literature and demonstrating success in improving the prescription of antibiotics in hospitalized patients, especially in inducing the switch to oral therapy and decreased duration of intravenous therapy.24–28 However, few studies have been conducted in developing countries and there is relatively little knowledge on effective strategies to improve antimicrobial use in this context.7 The aim of this study was to evaluate the effectiveness of an easy to implement intervention in the induction of early discontinuation of intravenous antimicrobial therapy and/or its switch to oral therapy.
MethodsThe present study adopted the historically controlled prospective model under the before and after an intervention type. It was conducted at the Clinical Hospital of the Federal University of Uberlândia (HCU, Hospital de Clínicas de Uberlândia), a public tertiary teaching hospital, holding 525 beds and entirely dedicated to SUS. The project for this study was approved by the Research Ethics Committee of the Federal University of Uberlândia (UFU, Universidade Federal de Uberlândia) under process number 379 467.
The HCU has a computerized prescription system that allows the exchange of information between the physician, clinical pharmacies, and the Hospital Infection Control Commission (CCIH, Comissão de Controle de Infecção Hospitalar). Among other functions, the system provides a daily list of patients who are initiating treatment with antimicrobials and only allows the prescription of these drugs when the physician fills in an “antimicrobial request form” in the system, justifying the need for its use.
Data collection and evaluations of the medical prescriptions and “antimicrobial request forms” were carried out by two researchers, a pharmacist and an infectious disease physician at the Hospital Infection Control Service (SCIH, Serviço de Controle de Infecção Hospitalar), in the control period (CP) – October and November 2013 – and in the intervention period (IP) – August and September 2014. The same methodology for data collection was used in both periods. All patients who initiated intravenous antibiotics during hospitalization in the 301 beds of the Medical and Surgical wards, in the adult Intensive Care Unit (ICU), and in the Emergency Room were consecutively followed until discharge, death, or for 60 days.
Patients who were already using intravenous antimicrobial on the first day of the study and those who were discharged or died in the first three days of intravenous antimicrobial therapy were excluded from evaluation. Patients who had their intravenous antimicrobial therapy discontinued or switched to oral before the third day of treatment were also excluded.
InterventionIntervention consisted of messages on the patient's electronic prescription by the third day of intravenous treatment and suspension of antimicrobial prescribing by the fifth day of intravenous treatment. The physicians saw the message only on the fourth day of treatment, upon a new prescription. It pointed to the evaluation of possible appropriateness (targeted therapy), discontinuation of the antimicrobial treatment or switch to oral therapy in case the patient was hemodynamically stable, afebrile, presented clinical and leukocyte count improvement, and was able to ingest and/or absorb the antimicrobial. In case the third day of intravenous antimicrobial therapy occurred over the weekend or holiday, the message was displayed on the following business day.
Suspension of the antimicrobials prescription of by the pharmaceutical researcher was only conducted on the fifth day of treatment with intravenous antimicrobial. The suspension took into account predetermined criteria based on national and international protocols and data available on the local antimicrobial resistance. When necessary, the treating physicians were contacted by telephone for clarification of the patients’ condition. To continue prescribing the suspended intravenous antimicrobial, the physician in charge for the patient had to fill in a computerized form justifying the continuation of the treatment. In case the fifth day of the injectable antimicrobial treatment occurred over the weekend or holiday, suspension of the prescription was made on the following business day.
OutcomesThe frequency of premature discontinuation of intravenous antimicrobial therapy or switch to oral therapy were considered as primary outcome, and the reduction in duration of intravenous therapy and of hospital stay as secondary outcomes. To evaluate safety and efficacy of the antimicrobial treatment the following were considered: need to resume intravenous antimicrobial therapy, mortality, and readmissions over a period of 60 days following patient's hospital discharge.
Statistical analysisStatistical analysis of the data was performed with the help of JMP® software (SAS Institute, 1995). Because the data were not normally distributed, as verified by the Shapiro–Wilk test at 5% significance level, differences between the medians of hospital stay and duration of intravenous therapy in days were evaluated using the non-parametric Mann–Whitney test.
The Pearson's chi-square test was applied to evaluate the potential association between categorical variables assessed in the two study periods (CP and IP). The binomial test for comparing two proportions was applied for non-categorical variables. A level of 5% significance was considered.
The following outcomes were considered in data analysis: switch to oral therapy when it occurred by the fifteenth day of intravenous antimicrobial treatment; discontinuation of intravenous antimicrobial therapy without switching to oral therapy, when all antimicrobials used were discontinued before the fifteenth day of use and the patient remained hospitalized; maintenance of intravenous treatment until discharge, when intravenous antimicrobial therapy was used throughout the hospital stay. The patient's length of hospital stay was considered from the first day intravenous antimicrobial were prescribed until discharge, death, or 60 days of hospitalization.
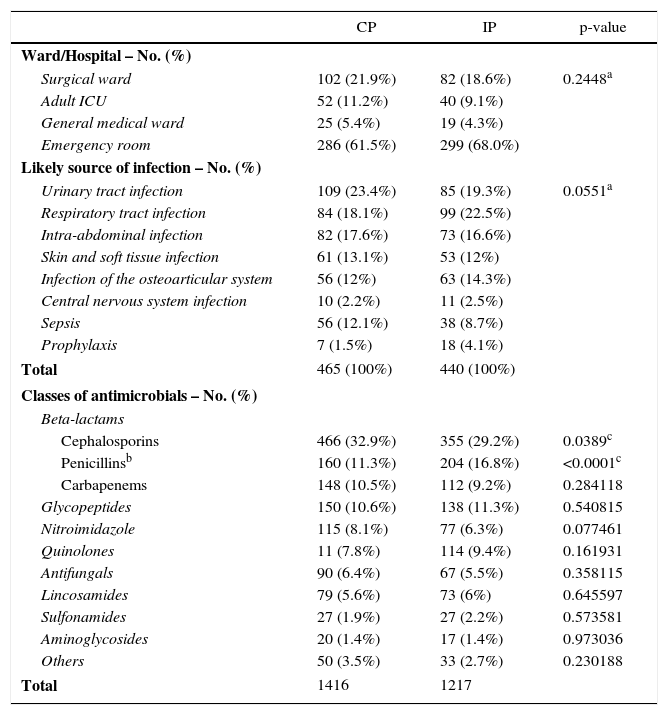
ResultsThe study included 465 patients in the CP and 440 patients in the IP. The patients’ mean age in years was similar in both study periods, 48±23.69 years in the CP and 48±23.74 in the IP (p=0.9253). In the CP, 264 patients were male (56.8%) compared to 282 (64.1%) in the IP (p=0.0271). Clinical features, wards, and the most commonly used classes of antimicrobials in both CP and IP are shown in Table 1.
Characteristics of the assessed patients and classes of commonly used antimicrobials in the control period (CP) and intervention period (IP).
| CP | IP | p-value | |
|---|---|---|---|
| Ward/Hospital – No. (%) | |||
| Surgical ward | 102 (21.9%) | 82 (18.6%) | 0.2448a |
| Adult ICU | 52 (11.2%) | 40 (9.1%) | |
| General medical ward | 25 (5.4%) | 19 (4.3%) | |
| Emergency room | 286 (61.5%) | 299 (68.0%) | |
| Likely source of infection – No. (%) | |||
| Urinary tract infection | 109 (23.4%) | 85 (19.3%) | 0.0551a |
| Respiratory tract infection | 84 (18.1%) | 99 (22.5%) | |
| Intra-abdominal infection | 82 (17.6%) | 73 (16.6%) | |
| Skin and soft tissue infection | 61 (13.1%) | 53 (12%) | |
| Infection of the osteoarticular system | 56 (12%) | 63 (14.3%) | |
| Central nervous system infection | 10 (2.2%) | 11 (2.5%) | |
| Sepsis | 56 (12.1%) | 38 (8.7%) | |
| Prophylaxis | 7 (1.5%) | 18 (4.1%) | |
| Total | 465 (100%) | 440 (100%) | |
| Classes of antimicrobials – No. (%) | |||
| Beta-lactams | |||
| Cephalosporins | 466 (32.9%) | 355 (29.2%) | 0.0389c |
| Penicillinsb | 160 (11.3%) | 204 (16.8%) | <0.0001c |
| Carbapenems | 148 (10.5%) | 112 (9.2%) | 0.284118 |
| Glycopeptides | 150 (10.6%) | 138 (11.3%) | 0.540815 |
| Nitroimidazole | 115 (8.1%) | 77 (6.3%) | 0.077461 |
| Quinolones | 11 (7.8%) | 114 (9.4%) | 0.161931 |
| Antifungals | 90 (6.4%) | 67 (5.5%) | 0.358115 |
| Lincosamides | 79 (5.6%) | 73 (6%) | 0.645597 |
| Sulfonamides | 27 (1.9%) | 27 (2.2%) | 0.573581 |
| Aminoglycosides | 20 (1.4%) | 17 (1.4%) | 0.973036 |
| Others | 50 (3.5%) | 33 (2.7%) | 0.230188 |
| Total | 1416 | 1217 | |
The median patients’ length of hospital stay was 11 days in the CP (interquartile range 6 and 21.5 days) similar to the IP (11; 7 and 21 days) [p=0.8853]. The duration of intravenous therapy was one day lower in the IP (median: 9; interquartile range 6 and 17 days) compared to the CP (median: 10; interquartile range 6 and 18 days), a non significant difference (p=0.1360). The proportion of readmitted patients was significantly higher in the IP (11.6%) compared to the CP (7.1%) [p=0.0199]. However, there was no significant difference in patients who switched to oral therapy, 9.1% (1/11) in the CP and 8% (2/25) in the IP (p=0.9131). The same occurred in patients who had their intravenous antimicrobial treatment discontinued, 10.98% (9/82) in the CP and 10.38% (11/106) in the IP [p=0.8950]. A total of 19.51% (16/82) of the patients had to resume intravenous antibiotics in CP and 22.64% (24/106) in the IP [p=0.6031]. Twenty-seven percent (3/11) of the patients resumed intravenous antibiotics after switching to oral therapy in the CP and 20% (5/25) in the IP [p=0.6287].
There was no difference in the percentage of patients who used other oral medications concomitantly with intravenous antimicrobials in both periods, 361 patients (77.6%) in the CP and 325 (73.9%) in the IP (p=0.1856).
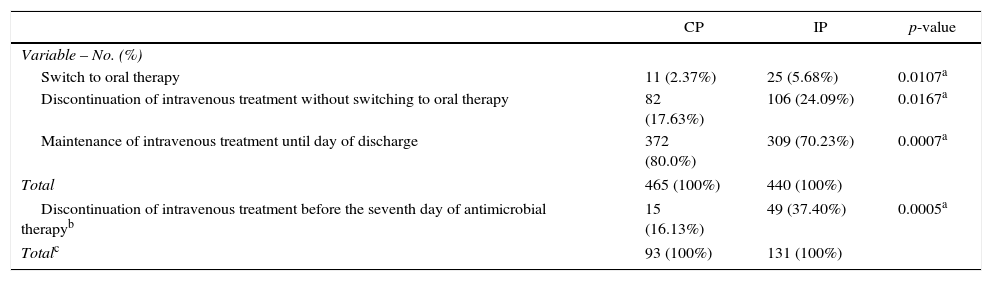
The intervention was associated with a significant increase in the number of patients who had their intravenous antimicrobial therapy stopped either by switching to oral therapy or by discontinuation without switching to oral therapy. The intervention was also associated with a significant increase in the number of patients who had their intravenous antimicrobial therapy discontinued before the seventh day (Table 2).
Frequency and type of changes in the antimicrobial intravenous treatment in patients evaluated during the control period (CP) and intervening period (IP).
| CP | IP | p-value | |
|---|---|---|---|
| Variable – No. (%) | |||
| Switch to oral therapy | 11 (2.37%) | 25 (5.68%) | 0.0107a |
| Discontinuation of intravenous treatment without switching to oral therapy | 82 (17.63%) | 106 (24.09%) | 0.0167a |
| Maintenance of intravenous treatment until day of discharge | 372 (80.0%) | 309 (70.23%) | 0.0007a |
| Total | 465 (100%) | 440 (100%) | |
| Discontinuation of intravenous treatment before the seventh day of antimicrobial therapyb | 15 (16.13%) | 49 (37.40%) | 0.0005a |
| Totalc | 93 (100%) | 131 (100%) | |
The results indicate that the tested intervention was effective, since it led to a significant increase in the number of patients who had their intravenous antimicrobial therapy stopped by switching to oral therapy or by having the treatment discontinued without switching to oral therapy. The results also indicate that the number of patients who had their intravenous antimicrobial treatment discontinued before the seventh day increased significantly by 21.27% during the intervention.
The significant increase in switching to oral therapy was less than impressive (3%). This percentage is much lower than that found in other studies conducted in other parts of the world.24,25,28 The low switching frequency to oral therapy in the HCU was already known.29 This study does not add to the understanding of this fact. This may occur due to organizational problems and medical practice, which could be reduced by educational intervention or structural changes. Furthermore, since the study design was not intended to follow patients after their discharge, the number of patients who had their antimicrobial therapy switched to oral therapy may have been underestimated. In the HCU, as well as in other Brazilian hospitals, problems such as overcrowding and waiting lists for admission encourage early discharge of patients.30 It is likely that as soon as the hospitalized patient can stop the treatment with intravenous antimicrobials or use it orally, he or she is discharged and oral therapy is started at home.
Among the criteria for switching to oral therapy are the ability to ingest drugs and the normal gastrointestinal function. Since in the two periods of the study most of the patients were using oral drugs from other pharmacological groups concomitantly with intravenous antibiotics, these patients probably did not have gastrointestinal intolerance, thus able to ingest and absorb oral antibiotics. Therefore, by hypothesis, gastrointestinal intolerance must not have been the cause for maintaining intravenous antimicrobial treatment in most cases.
Although the duration of the intravenous antimicrobial therapy decreased by one day, the reduction was not significant. However, as the criteria for switching to oral therapy or discontinuing the treatment were only evaluated in the IP, it was not possible to assess the effect of the intervention on the duration of intravenous antimicrobial therapy just in patients who met the criteria. Thus, the effect of the intervention on the duration of intravenous antimicrobial treatment was diluted since the analysis also included patients who did not meet the criteria, which was a limitation of the study.
While one might think that the good results of interventions evaluated in other studies are due to the fact that they were carried on more developed countries, with more organized healthcare facilities van Niekerk et al.31 demonstrated that despite facing difficulties, interventions in a developing country have led to an increased number of patients who had intravenous therapy switched to oral therapy, rising from 16% to 43.9%. There was also a decrease in the duration of the intravenous therapy and costs. This probably occurred because feedback to physicians and direct attempt to convince them to change the therapy were also part of the intervention.31
Although the two study periods occurred in different months of the year, allowing for possible seasonal bias, the demographic and clinical characteristics found were similar among the populations studied in the two different periods.
As noted in other studies in which interventions to reduce the duration of intravenous antimicrobial therapy was successful, we also observed no indication that there was any interference with the effectiveness of the treatment and patient safety.23,24,26 There was no difference between the two periods regarding the frequency of resuming intravenous antimicrobial treatment and mortality. In this context, the detected increase in the global percentage of readmissions in the IP could indicate a harmful effect of the intervention. However, when we analyze the percentage related only to the group of patients who switched to oral therapy, or who had antimicrobial treatment stopped, there was no significant difference. Then, the global increase probably occurred for reasons other than the intervention itself. We do not have enough data to explain the reason for such global increase.
The difference found in both periods regarding commonly used antimicrobial classes may be due to episodes of shortage of some antimicrobials, which occurred in both study periods. However, there was no lack of antimicrobials used orally in neither of the periods.
The significant result of this study contrasts with a previous study carried out in the same hospital, in which strategies involving preparation, presentation and distribution of guidelines, and daily reminders to physicians through labels affixed on non computerized prescriptions turned out ineffective.29 The difference is probably due to the use of computerized features in the present study that delivered the messages at the time the prescription were prepared and, above all, due to prescription suspension, which required physicians to fill in the justification for continued use of intravenous antimicrobials. These resources have been successfully used for the appropriateness of antimicrobials use.14,32
It must be considered that, despite the modest benefit of the intervention evaluated in this study, its implementation in places where the prescription system is similar, is simple and comes at a low cost. Other studies may test this intervention with some modifications. As this intervention was interrupted with the physician's justification, one could argue whether it would be more effective if the justification was assessed and if it was not convincing there should be an attempt to persuade the physician in charge. Perhaps a direct contact with the prescribers would produce even more significant outcomes. However, this study was looking for an effective, inexpensive, and easy to maintain strategy.
As long as computerization already exists, the proposed intervention can be easily implemented and enforced by the pharmacist in daily practice with good acceptance by physicians. A recent acknowledgment by Cochrane recognized that due to the complexity of healthcare organizations, individual hospitals will always have to evaluate their own interventions and that multi-faceted and complex interventions are not necessarily more effective than simple interventions.33
ConclusionWe conclude that the intervention carried out in this study is effective with regard to the early discontinuation of intravenous antibiotics and/or switch to oral therapy. Although this conclusion is not necessarily valid for all types of hospitals, this study suggests it is worthwhile at least testing the evaluated strategy in hospitals that wish to deploy some intervention toward that end. The cost/benefit ratio of the intervention should be ascertained, including whether computerization and/or appropriateness of the prescription system already exists or whether they are still necessary.
Other approaches related to the rational use of antimicrobial agents can also be added to the intervention as well as feedback to physicians for appropriateness of antimicrobial therapy. This study indicates that despite the difficulties faced in developing countries, pharmacists can contribute to an improvement in the use of antimicrobials in hospitals, and simple interventions such as the one proposed here are of low cost and easy to implement, which is especially important with regard to their maintenance and sustainability.
Conflicts of interestThe authors declare no conflicts of interest.