The purpose of this study was to assess the risk of abnormal anal cytology in women with known genital squamous intraepithelial lesion. This study evaluated 200 women with and without genital squamous intraepithelial lesion who were recruited for anal Pap smears. Women who had abnormal results on equally or over atypical squamous cells of undetermined significance were classified as having abnormal anal cytology. A multiple logistic regression analysis (stepwise) was performed to identify the risk for developing abnormal anal cytology. Data were analyzed using the SPSS 20.0 program. The average age was 41.09 (±12.64). Of the total participants, 75.5% did not practice anal sex, 91% did not have HPV-infected partners, 92% did not have any anal pathology, and 68.5% did not have anal bleeding. More than half (57.5%) had genital SIL and a significant number developed abnormal anal cytology: 13% in the total sample and 17.4% in women with genital SIL. A significant association was observed between genital squamous intraepithelial lesion and anal squamous intraepithelial lesion (PR=2.46; p=0.03). In the logistic regression model, women having genital intraepithelial lesion were more likely to have abnormal anal Pap smear (aPR=2.81; p=0.02). This report shows that women with genital squamous intraepithelial lesion must be more closely screened for anal cancer.
Anal and cervical cancers have many similarities that include association with human papillomavirus (HPV) infection, occurrence in an epithelial transformation zone, and coexistence with high-grade squamous intraepithelial lesions.1
HPV has been observed in 99% of cervical cancers and 80–90% of anal cancers.2–4 It is likely that the pathogenesis of anal cancer is similar to that of cervical cancer: that is, anal HPV infection, in conjunction with other yet to be determined factors, leads to the development of high-grade anal intraepithelial neoplasia (HGAIN), which is a probable precursor to anal cancer.4,5
Considering that programmatic screening for cervical cancer with cytology has been associated with considerably decreased incidence and mortality rates of cervical cancer,6 anal cytology has been assessed as a screening method for anal neoplasia in high-risk individuals in some countries such as the USA.7
Subjects with abnormal anal screening cytology are referred for a high-resolution anoscopy (HRA) or colposcopic evaluation of the anus. In cases diagnosed with HGAIN through directed biopsies, an ablation of HGAIN lesions must be done.8
Regardless of the extensive data on cervical neoplasia and HPV infection in women, there are limited data on anal neoplasia, anal HPV infection, and cytology. The purpose of this study was to assess the risk of abnormal anal cytology in women with known genital SIL.
This study, conducted at the LNRCC-Luis Antonio Hospital (hospital for cancer in Rio Grande do Norte, Brazil), assessed 200 HIV-seronegative women (using enzyme-linked immunosorbent assay [ELISA] and Western blot), 115 with and 85 without genital SIL. The first group of women had genital SIL diagnosed by cytology, genitoscopy, and biopsy, and the second group of women presenting for cervical cancer screening had no genital SIL, based on cytology (two negative Papanicolaou smears) and a negative genitoscopy. An expert pathologist reviewed the Papanicolaou tests and biopsies. Patients in use of immunosuppressive therapy, transplanted, and HIV-infected were excluded.
After obtaining written informed consent, each subject provided a detailed history of routine gynecologic healthcare and risk factors for the development of anal cytologic abnormalities. A standardized questionnaire inquired about history of anal intercourse; number of sexual partners; history of sexually transmitted diseases; cervical cytologic abnormalities; vulvar warts; cervical, vulvar, or vaginal cancers; solid organ transplantation; chronic corticosteroid use; history of cigarette smoking; and drug and alcohol use.
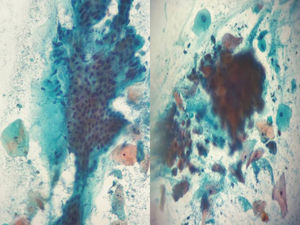
After administering the questionnaire and completing the patient history, a visual examination of the lower genital tract was performed, and samples were collected for cervical and anal cytology. The anal Pap smear was collected using a cytobrush, which was inserted 4cm into the anal canal. The cytobrush was rotated 360° in a cone-shaped area and removed. The sample was then smeared onto a glass slide, immediately fixed in 95% ethyl alcohol and transported to the laboratory. Papanicolaou staining was used for cytopathologic diagnosis and any cytological finding from ASCUS was considered abnormal (Fig. 1).
Statistical analysis with 95% confidence intervals performed using descriptive and inferential statistics. A dichotomous variable of anal SIL was used to assess its association with the other nominal variables using Chi-square and Fisher exact test. A multiple logistic regression analysis (stepwise) was performed to identify predictors independently associated with anal SIL. Data were analyzed using the SPSS 20.0 program, and the level of significance was set at 5%. This study was approved by the Ethics Research Committee of the institution (CAAE 1 07769612.3.0000.5293).
The mean age for patients included in this study was 41.09 (±12.64). Most were nonwhite (56%) and nonsmokers (91.5%), with up to eight years of school education (50.5%). Regarding the description of contextual variables, 55.5% used oral contraceptives, 9% used condoms, 80% had already been pregnant and of these 30% had had an abortion. The majority had up to three partners (73.5%) and had not contracted other (concomitant) sexually transmitted infection (STI), besides HPV (74%). More than half reported not practicing anal sex (75.5%), 91% had partners with no clinical evidence of HPV-induced lesions. 87.5% had not used drugs, and 96.5% denied bisexual relations. A large percentage of the women did not report any anal pathology (92%) or anal bleeding (68.5%). However, more than half had low genital intraepithelial lesions (57.5%), and a significant number developed abnormal anal cytology: 13% of the total sample and 17.4% among women with genital SIL. Concerning the association between anal SIL and the socioeconomic and contextual variables, a significant association was only observed between genital SIL and anal SIL (PR=2.46; p=0.03). There was no significant association between anal SIL and all other studied variables. In the logistic regression model, after adjusting for the variables age and partner with HPV, women with genital intraepithelial lesions presented more risk for abnormal anal Pap smear (aPR=2.81; p=0.02) (Table 1). Abnormal anal cytology was observed in 11 patients with cervical high squamous intraepithelial lesion (HSIL – NIC2 and 3), nine patients with cervical low squamous intraepithelial lesion (LSIL – NIC1), and in six women with inflammatory samples. However no differences were observed between the HSIL and LSIL groups. Vulvar lesions (genital warts) were found in four patients with LSIL – NIC1 cervical samples.
The risk of anal SIL in women with genital HPV induced lesions.
| Variable | Category | Anal SIL | PR | CI 95% | p | aPRb | aCI 95% | pc value | |
|---|---|---|---|---|---|---|---|---|---|
| Yes (%) | No (%) | ||||||||
| GSIL | Yes | 20 (17.4%) | 95 (82.6%) | 2.46 | 1.03–5.87 | 0.03a | 2.81 | 1.16–6.79 | 0.02 |
| No | 6 (7.1%) | 79 (92.9%) | |||||||
| Age | Until 41 years | 11 (11.3%) | 86 (88.7%) | 0.78 | 0.38–1.61 | 0.49 | |||
| >41 years | 15 (14.6%) | 88 (85.4%) | |||||||
| Race | White | 8 (9.1%) | 80 (90.9%) | 0.57 | 0.26–1.24 | 0.14 | |||
| Non White | 18 (16.1%) | 94 (83.9%) | |||||||
| Years of study | <8 years | 13 (12.9%) | 88 (87.1%) | 0.98 | 0.48–2.01 | 0.95 | |||
| >8 years | 13 (13.1%) | 86 (86.9%) | |||||||
| Smoking | Yes | 1 (5.9%) | 16 (94.1%) | 0.43 | 0.06–2.98 | 0.362 | |||
| No | 25 (13.7%) | 158 (86.3%) | |||||||
| Contraceptive use | Yes | 16 (12.6%) | 111 (87.4%) | 0.92 | 0.44–1.92 | 0.824 | |||
| No | 10 (13.7%) | 63 (86.3%) | |||||||
| N. partner | >3 | 18 (12.2%) | 129 (87.8%) | 0.81 | 0.37–1.75 | 0.59 | |||
| >3 | 8 (15.1%) | 45 (84.9%) | |||||||
| STD | Yes | 6 (11.3%) | 47 (88.7%) | 0.83 | 0.35–1.96 | 0.67 | |||
| No | 20 (13.6%) | 127 (86.4%) | |||||||
| HPV partner | Yes | 4 (22.2%) | 14 (77.8%) | 1.84 | 0.71–4.75 | 0.22 | |||
| No | 22 (12.1%) | 160 (87.9%) | |||||||
| Anal sex | Yes | 8 (16.3%) | 41 (83.7%) | 1.37 | 0.63–2.95 | 0.42 | |||
| No | 18 (11.9%) | 133 (88.1%) | |||||||
| Drug user | Yes | 1 (20.0%) | 4 (80.0%) | 1.56 | 0.26–9.35 | 0.63 | |||
| No | 25 (12.8%) | 170 (87.2%) | |||||||
| Anal disease | Yes | 1 (6.3%) | 15 (93.8%) | 0.46 | 0.07–3.18 | 0.40 | |||
| No | 25 (13.6%) | 159 (86.4%) | |||||||
| Anal bleeding | Yes | 5 (7.9%) | 58 (92.1%) | 0.52 | 0.20–1.31 | 0.149 | |||
| No | 21 (15.3%) | 116 (84.7%) | |||||||
GSIL, genital squamous intraepithelial lesions; SIL, squamous intraepithelial lesion; PR, prevalence ration; CI, confidence interval; aPR, adjusted prevalence ration; aCI, adjusted confidence interval; STD, sexually transmitted disease.
The anal Pap smear has been a beneficial tool for early detection of intra-anal dysplasia in patients at risk, such as HIV-infected men and women.9,10
In this study, there was no difference in the sociodemographic characteristics of women with genital lesions and women without HPV-associated genital lesions. Age and anal sex were not significantly associated with abnormal anal cytology or anal HPV-induced lesions in the study group, which is in contrast to past studies.11,12
Concerning prevalence, in this group we found abnormal anal cytology in 13% of the total sample and in 17.4% among women with genital SIL. Earlier, Jacyntho et al.11 observed similar rates comparing 184 women with known genital SIL and 76 controls without genital SIL. Anal intraepithelial neoplasia was observed in 32 (17.4%) of the 184 women with genital SIL compared with two (2.6%) of the 76 controls without genital SIL.11 Tatti et al.,13 studying 481 immunocompetent and immunosuppressed women with genital SIL, found a higher prevalence of abnormal anal cytology (27.8%), probably due to the inclusion of HIV-infected patients.12 Several studies have reported that HIV-infected women have higher rates of abnormal anal cytology and histopathology results than HIV-uninfected women.10,13,14 These results suggest that mainly in HIV-infected women, the presence of genital HPV-induced lesions could predict a probable abnormal anal cytology.
Considering that HPV infection is strongly linked with anal cancer and usually considered a field infection of the anogenital tract, it is possible that women with a history of genital SIL may be under a higher risk for anal cancer. Many large-scale cancer registry studies support robust associations between a history of genital SIL and cancers of the anus.15–17 In a population-based cohort study, Edgren and Sparén15 evaluated the risk of anal cancer in women with a later history of CIN3 by linking Swedish national registries with cancer registries. The incident rate ratio was 4.68 for women with prior high-grade cervical lesion when compared with those with no cervical lesion. The risk was substantially elevated five years after the diagnosis for all ages.15
A recent study examined women with high-grade disease (defined as in situ) or invasive cervical, vulvar, or vaginal cancer. The authors identified a significant association between previous genital SIL and invasive cancers of the cervix, vulva, vagina, and anus.16
A large study examined the long-term risk trend for a second cancer among 104,760 women with cervical cancer. Women with diagnosed cervical cancer had greater risk of developing anal cancer than women in the general population.17
In conclusion, there is powerful epidemiological evidence18 showing a raised risk of anal cancer in women with a previous history of in situ and invasive cancers of the cervix, vagina, and vulva compared with the general population. In this study, we observed a higher risk for abnormal anal cytology in women with genital HPV-induced lesions, suggesting that these women must be more closely screened for anal cancer.
Conflicts of interestThe authors declare no conflicts of interest.