In recent years, there has been growing concern about an increasing rate of cardiovascular diseases in human immunodeficiency virus-infected patients, which could be associated with side effects of highly active antiretroviral therapy. It is likely that the metabolic disorders related to anti-human immunodeficiency virus treatment will eventually translate into a increased cardiovascular risk in patients submitted to such regimens.
ObjectiveTo evaluate if human immunodeficiency virus-infected patients receiving highly active antiretroviral therapy are at higher risk of cardiovascular diseases than human immunodeficiency virus infected patients not receiving highly active antiretroviral therapy, or the general population.
Research design and methodsWe conducted a computer-based search in representative databases, and also performed manual tracking of citations in selected articles.
ResultThe available evidence suggests an excess risk of cardiovascular events in human immunodeficiency virus-infected persons compared to non-human immunodeficiency virus infected individuals. The use of highly active antiretroviral therapy is associated with increased levels of total cholesterol, triglycerides, low-density lipoprotein and morphological signs of cardiovascular diseases. Some evidence suggested that human immunodeficiency virus-infected individuals on highly active antiretroviral therapy regimens are at increased risk of dyslipidemia, ischemic heart disease, and myocardial infarction, particularly if the highly active antiretroviral therapy regimen contains a protease inhibitor.
ConclusionPhysicians must weigh the cardiovascular risk against potential benefits when prescribing highly active antiretroviral therapy. Careful cardiac screening is warranted for patients who are being evaluated for, or who are receiving highly active antiretroviral therapy regimens, particularly for those with known underlying cardiovascular risk factors. A better understanding of the molecular mechanisms responsible for increased risk of cardiovascular diseases in human immunodeficiency virus-infected patients will lead to the discovery of new drugs that will reduce cardiovascular risk in human immunodeficiency virus-infected patients receiving highly active antiretroviral therapy.
The widespread use of highly active antiretroviral therapy (HAART) – comprising protease inhibitors (PIs) and/or non-nucleoside reverse transcriptase inhibitors (NNRTIs) combined with nucleoside reverse-transcriptase inhibitors (NRTIs) – has dramatically decreased the morbidity and mortality associated with human immunodeficiency virus (HIV) infection in the developed world.1,2
Since the introduction of HAART in 1995, a significant decrease in mortality was observed in HIV-infected patients associated with a marked reduction in the incidence of opportunistic infections and certain kind of cancers.3,4 However, current evidence suggests that patients on HAART are at increased risk of developing cardiovascular disease (CVD), and recent studies reported a higher prevalence of traditional risk factors for CVD in HIV-infected patients than in non-infected controls, such as arterial hypertension, dyslipidemia, and diabetes mellitus. These abnormalities may be associated with the use of certain antiretroviral drugs.5
HIV infection leads to a chronic systemic inflammatory process, which is increasingly accepted as having an important role in the pathogenesis of atherosclerosis and acute cardiovascular events. HIV-infected patients have been described as presenting unique histological features of coronary artery disease, including a rapid progression of diffuse circumferential arterial lesions with proliferation of smooth muscle cells, elastic fibers, and endoluminal protrusions.6
HIV-infected patients with acute coronary syndrome tend to be younger, with lower high-density lipoprotein (HDL) levels, higher prevalence of smoking, and less angiographically apparent coronary artery disease, when compared to non-HIV patients, which represents a different epidemiological pattern. HIV-infected patients may have concomitant traditional risk factors for CVD such as smoking, hypertension, and dyslipidemia, but the HIV and HAART may interact with these factors and contribute to the increased incidence of CVD. The long-term benefits of HAART are remarkable, but the associated complications make the overall management of HIV-infected patients more complex and costly.7
Because of the dissemination of HIV infection and its potential association with CVD, some authors have proposed a routine and systematic evaluation of HIV-infected adults and children, including medical history, cardiac examination and systematic echocardiographic monitoring, since asymptomatic cardiac disease and cardiac symptoms can often be misled by secondary effects of HIV infection.8
The aim of this review was to evaluate if HIV-infected patients receiving HAART are at higher risk of CVD in relation to HIV-infected patients not receiving HAART and to the general population.
MethodsWe performed a computer-based search, querying Ovid MEDLINE (1950 to July 2012), CINAHL (Cumulative Index to Nursing and Allied Health, 1982 to July 2012), EMBASE (1980 to July 2012), and the Cochrane Central Register of Controlled Trials for original research articles published in English, Spanish and Portuguese. Medical Subject Headings (MeSH) were used as search terms when available, and keywords were used when appropriate. Terms for Anti-HIV Agents, HIV Infections, Cardiovascular Diseases, and Cardiovascular Diseases/complications were combined with a variety of MeSH terms to delimit relevant study designs and populations.
The selected outcome measures were common clinical cardiovascular outcomes (e.g. ischemic heart disease (IHD), heart failure (HF), cerebrovascular disease, acute coronary syndrome, myocardial infarction (MI) and peripheral vascular disease), or established traditional risk factors for CVD (e.g. hypertension and hypercholesterolemia).
One reviewer made the search and the initial selection of potentially relevant studies meeting the inclusion criteria and two independent reviewers selected articles that met the established inclusion and exclusion criteria. Studies were assessed for use of an appropriate source population, measurement methods of exposure and outcome, methods to deal with design-specific issues such as bias and lost to follow-up, use of analytical methods and use of statistics for primary analysis of effect. A manual tracking of citations in articles selected was also performed.
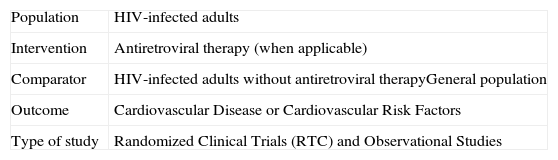
The structure of the search is shown in Table 1. Abstracts and relevant full-text articles were reviewed by one researcher.
PICO.
| Population | HIV-infected adults |
| Intervention | Antiretroviral therapy (when applicable) |
| Comparator | HIV-infected adults without antiretroviral therapyGeneral population |
| Outcome | Cardiovascular Disease or Cardiovascular Risk Factors |
| Type of study | Randomized Clinical Trials (RTC) and Observational Studies |
The search strategy identified 205 titles, 159 of which were excluded because they did not match the source population, outcome or study design did not address the research question. Of 46 potential articles, only 26 were directly related to the main goal of this review, and two studies were added after manual search. A total of 28 articles were included in the review: four randomized clinical trials and 24 observational studies being 22 prospective cohorts and two case–control studies.
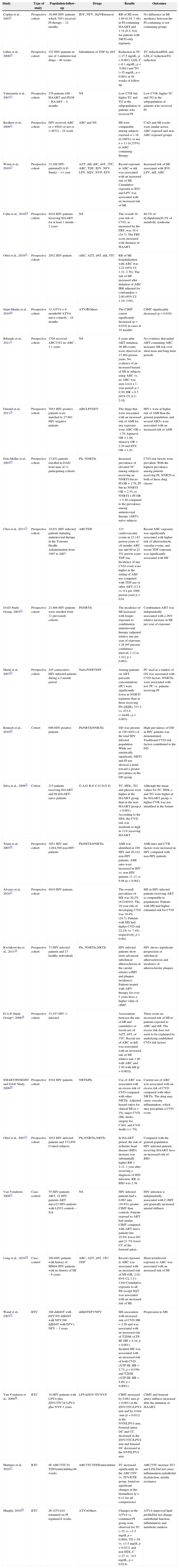
Table 2 summarizes the main characteristics and results of studies included in this review.
Study characteristics and results.
| Study | Type of study | Population-follow-up | Drugs | Results | Outcomes |
|---|---|---|---|---|---|
| Coplan et al., 20039 | Prospective cohort | 10,986 HIV-patients which 7951 received PI therapy – 12 months | IDV, NFV, SQVRitonavir | RR of MI were 1.69 (0.54, 7.48) in PI-containing HAART and 1.74 (0.5, 9.0) for patients with NRTI-only regimens. | No difference in MI incidence between the PI containing or not containing groups |
| Llibre et al., 200610 | Prospective cohort | 352 HIV-patients in use of 3 antiretroviral drugs – 48 weeks | Substitution of TDF by d4T | Reduction in TC (−17.5mg/dL; p<0.001), LDL-C (−8.1mg/dL; p<0.001) and TG (−35mg/dL; p<0.001) at 48 weeks of follow up. | TC reductionHDL and LDL-C reductionTG reduction |
| Velenzuela et al., 200711 | Prospective cohort | 276 patients:168 – HAART and PI108 – HAART – 4 months | NS | Low CVR but higher TC and TG in the subpopulation of patients who received PI | Low CVR; higher TC and TG in the subpopulation of patients who received PI |
| Brothers et al., 200912 | Prospective cohort | HIV received ABC (n=9502) or not (n=4672) – 24 week | ABC and NS | MI were comparable among subjects exposed n=16 (0.168%); or not n=11 (0.235%) to ABC-containing therapy. | CAD and MI events were similar across ABC-exposed and non-ABC-exposed groups |
| Worm et al., 201013 | Prospective cohort | 33,308 HIV-patients(D:A:D Study) – >1 year | AZT, ddI, ddC, d4T, 3TC, ABC, TDF, IDV, NFV, LPV, SQV, NVP, EFV | Recent exposure to ABC or ddi was associated with an increased risk of MI. Cumulative exposure to IDV and LPV was associated with an increased risk of MI. | Increased risk of MI associated with IDV, LPV, ddI, ABC |
| Cahn et al., 201014 | Prospective cohort | 4010 HIV-patients receiving HAART for at least 1 month – 2 years | NS | The overall 10-year risk of CVD, as measured by the FRF, was 10.4 (24.7). The FRF score increased with duration of HAART. | 80.2% of dyslipidemia20.2% of metabolic syndrome |
| Obel et al., 201015 | Prospective cohort | 2952 HIV-patient | ABC, AZT, d4T, ddI, 3TC | RR of MI hospitalization with ABC was 2.22 (95% CI 1.31–3.76). The risk of MI increased after initiation of ABC IRR adjusted for confounders=2.00 (95% CI 1.10–3.64). | |
| Saint-Martin et al., 201016 | Prospective cohort | 33 ATV/r>6 months99 ATV/r naive controls – 18 months | ATV/ROthers | The CIMT course significantly decreased (p=0.018) in cases at 18 months. | CIMT significantly decreased (p=0.018) |
| Ribaudo et al., 201117 | Prospective cohort | 1704 received ABC3352 no ABC – 3.1 years | NS | 6 years after ART initiation, 36 MI events were observed in 17,404 person-years. No evidence of an increased hazard of MI in subjects using ABC vs. no ABC was seen (over a 1-year period: p=0.50; HR=0.7 [95% CI, 0.2–2.4]). | No evidence that initial ART containing ABC increases MI risk over short-term and long-term periods |
| Durand et al., 201118 | Prospective cohort | 7053 HIV-positive patients were matched to 27,681 HIV-negative patients | ABCLPVEFV | The drugs that were associated with an increased risk of AMI for any exposure were ABC OR=1.79, lopinavir OR=1.98, ritonavir OR=2.29 and EFZ OR=1.83. | HIV+ were at higher risk of AMI than the general population, and several ARTs were associated with an increased risk of AMI |
| Friis-Moller et al., 200319 | Prospective cohort | 17,852 patients enrolled in DAD from nine of 11 participating cohorts | PIs, NNRTIs | Increased prevalence of elevated TC among subjects receiving an NNRTI but no PI OR=1.79, PI but no NNRTI OR=2.35, or NNRTI+PI OR=5.48 compared to the prevalence among antiretroviral therapy (ART)-naïve subjects. | CVD risk factors were prevalent. With the highest prevalence among patients receiving PI, NNRTI or both of these drug classes |
| Choi et al., 201121 | Prospective cohort | 10,931 HIV-infected patients initiating antiretroviral therapy in the Veterans Health Administration from 1997 to 2007 | ABCTDF | 123 cardiovascular events in 15,142 person-years of <6 months ABC use and 90 in 22 551 person-years TDF use. Incidence of any CVD event were higher in the setting of ABC use compared with TDF use or other ART (13.4 vs. 9.4 per 1000 person-years p<0.01. | Recent ABC exposure was significantly associated with higher risk of atherosclerotic vascular events, and recent TDF exposure was significantly associated with HF |
| DAD Study Group, 200322 | Prospective cohort | 23,468 HIV-patients were enrolled from 11 previously cohorts | PIsNRTIs | The incidence of MI increased with longer exposure to combination antiretroviral therapy (adjusted relative rate per year of exposure, 1.26 [95 percent confidence interval, 1.12 to 1.41]; p<0.001). | Combination ART was independently associated with a 26% relative increase in MI per year of exposure |
| Masiá et al., 200723 | Prospective cohort | 245 consecutive HIV-infected patients during a 2-month period | NaïveNNRTIsPI | Among patients on ART, peroxide concentrations (PC) were significantly lower in NNRTI regimens than in those receiving PIs ([IQR], 331.2 vs. 472.8t∼mol/L; p=0.003). | PC used as a marker of OS was associated with CVD factors. NNRTIs were associated with low PC vs. patients receiving PI |
| Reinsch et al., 201024 | Cohort | 698 HIV-positive patients | PIsNRTIsNNRTIs | DD was present in 336 (48%) of the total HIV infected population. While not statistically significant, NRTI and PI use showed a trend toward a greater prevalence in the DD group. | High prevalence of DD in HIV patients was demonstrated. Traditional CVD risk factors contributed to the DD |
| Silva et al., 200925 | Cohort | 215 patients receiving HAART and 69 HAART-naive patients | G A:G B:G C:G D:G E: | TC, HDL, TG and glucose were higher in the HAART group than in the non-HAART group p<0.001). According to the FRS, the CVD risk was moderate to high in 11% receiving HAART. | Although the mean values for TC, HDL-c and TG were higher in the HAART group, a higher CVR was not identified in the former |
| Triant et al., 200726 | Prospective cohort | 3851 HIV and 1,044,589 non-HIV patients | PIsNRTIsNNRTIs | AMI was identified in 189 HIV and 26,142 non-HIV patients. AMI rates were increased in HIV vs. non-HIV patients 11.13 vs. 6.98 (p<0.001). | AMI rates and CVR factors were increased in HIV compared with non-HIV patients |
| Alvarez et al., 201027 | Prospective cohort | 4010 HIV patients | The overall prevalence of MS was 20.2% (812/4010). The 10-year risk of developing CVD was 10.4% (24.7). Patients with MS had higher CVD risk 22.2% vs. 7.4%, respectively, p<0.001. | MS in HIV-infected patients receiving ART is comparable to populations. Patients with MS had higher estimated risk for CVD | |
| Kwiatkowska et al., 201128 | Prospective cohort | 72 HIV infected patients and 27 healthy individuals | PIs, NNRTIs,NRTIs | HIV infected patients show more advanced subclinical atherosclerosis in the carotid arteries (cIMT and plaques incidence). Patients treated with ARV therapy for over 5 years have a higher value of cIMT. | HIV shows significant progression of subclinical atherosclerosis and incidence of atherosclerotic plaques |
| D:A:D Study Group*, 200829 | Prospective cohort | 33,347 HIV-1-infected | Associations between the rate of MI and cumulative or recent use of AZT, d4T, or 3TC. Recent use of ABC or ddI was associated with an increased rate of MI relative rate 1.90 with ABC and 1.49 with ddI [p=0.003]). | There exists an increased risk of MI in patients exposed to ABC and ddI. The excess risk does not seem to be explained by underlying established CVD risk factors | |
| SMART/INSIGHT and DAD Study, 200830 | Prospective cohort | 4544 HIV patients | NRTIsPIs | Use of ABC was associated with an excess risk of CVD compared with other NRTIs. Adjusted hazard ratios for clinical MI (n=19), major CVD (MI, stroke, surgery for CAD, and CVD death; n=70). | Current use of ABC was associated with an excess risk of CVD compared with other NRTIs. The drug may cause vascular inflammation, which may precipitate a CVD event |
| Obel et al., 200731 | Prospective cohort | 3953 HIV-infected patients and 373,856 Control subjects | PIs,NNRTIs,NRTIs | In HAART period, the risk of ischemic heart disease (IHD) increase was substantially higher RR=2.12. 1 year after receiving a diagnosis of HIV infection, RR of IHD was 2.38. | Compared with the general population, HIV-infected patients receiving HAART have an increased risk of IHD |
| Van Vonderen 200933 | Case–control | 55 HIV-patients ART, 22 HIV-patients ART naive23 HIV-patients with LD52 controls – NA | NS | HIV infected patients had a 0.067mm (10.8%) greater CIMT than controls. Patients exposed to ART had similar CIMT compared with ART-naive patients but 25.9% lower DC and 21.7% lower CC of the femoral artery. | HIV infection is independently associated with C-IMT and generally increased arterial stiffness |
| Lang et al., 201034 | Case–control | 289 HIV-patients with history of MI884 HIV-patients with no history of MI – 6 years | ABC, AZT, d4T, 3TC, TDF | Recent exposure to ABC was associated with an increased risk of MI (OR, 2.01; 95% CI, 1.11–3.64) Cumulative exposure to all PIs except SQV was associated with an increased risk of MI. | Short-term/recent exposure to ABC was associated with an increased risk of MI |
| Wand et al., 200735 | RTC | 288 ddI/d4T with EFV305 ddI/d4T with NFV288 ddI/d4T with EFV+ NFV – 3 years | ddId4TEFVNFV | MS association with increased risk of CVD HR=2.56 and was associated with an increased risk of T2DM (ATP-III: HR=4.34; p=0.001). Incident MS was associated with an increased risk of both CVD (ATP-III: HR=2.73; p=0.036) and T2DM (ATP-III: HR=4.89; p<0.0001). | Progression to MS |
| Van Vonderen et al., 200936 | RTC | 19 HIV-patients with LPV/r plus ZDV/3TC18 LPV/r plus NVP-3 years | LPV/rZDV3TCNVP | CIMT increased by 0.061mm (p<0.001) in the ZDV/3TC/LPV/r arm and by 0.044mm (p=0.012) in the NVP/LPV/r arm. Femoral artery DC and CC decreased in the ZDV/3TC/LPV/r arm and femoral DC decreased in the NVP/LPV/r arm. | CIMT and femoral artery stiffness increased after the initiation of HAART |
| Martınez et al., 201037 | RTC | 46 ABC/3TC34 TDF/emtricitabine)48 weeks | ABC3TCTDFEmtricitabine | TC increased significantly in the ABC/3TC vs. TFV/ETB group, found no significant changes in the biomarkers (p=0.12 for all comparisons) | ABC/3TC increase TCl and LDLDid not cause inflammation,endothelial dysfunction, insulin resistance |
| Murphy 201038 | RTC | 26 ATV/r24 remained on PI regimen24 weeks | ATV/rOthers | Changes in the ATV/r vs. continued PI group were observed for TC (−25 vs. +1.5mg/dl, p=0.009), TG (−58 vs. +3.5mg/dl, p=0.013), and non HDL-C (−27 vs. −0.5mg/dL, p=0.014). | ATV/r improved lipid profileDid not change endothelial function, inflammatory and metabolic markers |
TC, total cholesterol; HDL-C and LDL-C, high and low-density lipoprotein cholesterol; TG, triglycerides; CVR, cardiovascular risk; MI, myocardial infarction; AMI, acute myocardial infarction; FRF, Framingham risk score; CAD, coronary artery disorder; CIMT, carotid intima–media thickness; LD, lipodystrophy; MS, metabolic syndrome; 3TC, lamivudine; AZT, zidovudine; d4T, stavudine; ddC, zalcitabine; ddI, didanosine; EFV, efavirenz; IDV, indinavir; LPV, lopinavir/ritonavir; NFV, nelfinavir; NVP, nevirapine; SQV, saquinavir; TDF, tenofovir; ATV/r, atazanavir; ABC, Abacavir; ETB, emtricitabine; OPG, osteoprotegerin; ADT, adiponectin.
G A: (AZT)+(3TC)+EFV; G B: AZT+3TC+LPV e AZT+3TC+NFV; G C: AZT+3TC+ATV/r; G D: (d4T)+3TC+EFV; G E: d4T+3TC+LPV e d4T +3 TC+NFV e d4T+ddI+LPV (RTI) – reverse transcriptase inhibitors not specified (NS); not applicable (NA); relative risk (RR).
Evidence from the included studies indicates that exposure to antiretroviral drugs is associated with an increased rate of CVD events. HIV infection decreases good cholesterol, increases triglycerides (TG), total cholesterol (TC), and vascular inflammation.10,16–19,22,24,25,30 Traditional cardiovascular risk (CVR) factors substantially contribute to the development of diastolic dysfunction (DD) in the HIV-infected patients.15
The use of several antiretroviral agents favors the occurrence of multiple metabolic and morphologic abnormalities, including dyslipidemia, insulin resistance, subcutaneous fat loss, visceral fat accumulation, and metabolic syndrome (MS), which are associated with an increased risk of premature atherosclerosis and MI.6,9,11,13,16,18,28 HAART may also indirectly or directly induce endothelial dysfunction.19,24
HIV infection itself is an independent risk factor for acute myocardial infarction (AMI), and increase arterial stiffness. Compared with the general population, HIV-infected patients receiving HAART have an increased risk of AMI and IHD,18,26,31,33,36 and increase in thickness of the intima–media complex.28,33
Combination antiretroviral therapy is associated with MI,9,13,22,29 and longer exposure to HAART and/or PIs seem to increase the risk of MI.29,32 HIV-infected patients using PI had slightly higher CVD risk than those using NNRTI, and slightly increased risk for patients using abacavir (ABC) or didanosine (ddI).18,26 Recent ABC exposure was significantly associated with higher risk of atherosclerotic vascular events, CVD, and an increased risk of MI.21,30,34 There exists an increased risk of MI in patients exposed to ABC and ddI within the preceding six months.29
DiscussionCardiovascular complications of HIV disease are generally late manifestations and may be related to prolonged effects of immunosuppression and a complex interplay of mediator effects from opportunistic infections, autoimmune response to viral infection, drug-related cardiotoxicity, nutritional deficiencies, and prolonged immunosuppression.39
There are many ways to assess the risk of CVD and multiple risk factors can be examined, such as age, gender, body mass index (BMI), TC, LDL, TG, MS, MS, carotid intima–media thickness (CIMT). These traditional risk factors for CVD increase risk of cardiovascular events in both HIV-infected and uninfected individuals.
For HIV-infected patients the retroviral chronic infection per se, the use of HAART and/or at least some of the antiretroviral drugs, and lipodistrophy can be considered additional risk factors. HIV infection plays a substantial role on blood lipids disorders and can induce endothelial cells injury which leads to a local inflammatory response that could promote thrombosis, impair vessel responsiveness, and is an important factor for arterial plaque formation. HIV replication may activate endothelial surfaces directly or via up-regulation of pro-inflammatory cytokines.
Some studies suggested that even though the overall cardiovascular event rate is low, there is an excess risk of cardiovascular events in HIV-infected persons compared to non-HIV-infected individuals. Some evidence suggested that HIV-infected individuals on HAART regimens are at increased risk of dyslipidemia, IHD, and MI, particularly if the HAART regimen contains a PI. While lipid-lowering drugs are a routine strategy for CVR reduction in the general population, HIV-infected people are usually not on those drugs even when clinically indicated.40
In this review we observed some different outcomes associated with different results. When the outcome was MI and the use of ABC was investigated, in three studies increased MI incidence was detected13,15,34 and in two studies there were no significant differences.12,17 Recently, the U.S. Food and Drug Administration (FDA) conducted a meta-analysis in which ABC use was randomized as part of a combined antiretroviral regimen and found no association between the use of ABC and MI.41
When the outcome was the change in lipid profile, two studies showed a reduction on TC, LDL, TG,10,38 and two demonstrated an increase in blood lipids.11,37 Two studies showed an increase in CIMT,10,33 and one demonstrated a decrease in CIMT.16
We must be aware that the population studied in all of the reviewed studies are HIV-infected adult patients, but with different characteristics. The studied populations had different age ranges and gender; different stages of HIV infection and most of them were receiving different antiretroviral drugs regimens, which could have different effects not only in the surrogate markers of CD risk but mainly in the incidence of CVD.
In spite of individual studies suggesting that currently available PIs could increase the CVR,18,26,29,32 the PI class remained a very effective class of antiretroviral drugs for HIV infection therapy. Life expectancy for HIV-infected patients has improved by 20 years for those diagnosed at age 25–33 years, and it is still improving. The HIV-infected population is becoming more susceptible to all chronic diseases that are observed in non-HIV-infected patients with the presence of additional risk factors for CVD due to infection and the treatment itself.42
The clinical expression of cardiac involvement is variable and is affected by the stage of HIV disease, the degree of immunodeficiency, and the use of drugs to treat HIV disease or to treat or prevent opportunistic infections and neoplasms.43 CVR must be considered in the overall care of adults with HIV infection. However, such risk should not influence the decision of when to initiate antiretroviral therapy, and the decision of which antiretroviral regimen to use should be made based on risk and benefit analysis that includes the clear survival benefit associated with maximal viral suppression.
HIV-infected patients confront an escalating epidemic of CVD that is comparable to that faced by the general population more than half a century ago. Stratifying risk among HIV-infected patients and devising cardiovascular preventive strategies are priorities.44 The initial choice of ART regimen and subsequent modifications also may be considered in planning CVD prevention strategies, because the risks of inadequately treated HIV infection outweigh any increase in CVD risk that may be associated with ART, and with the understanding that uncontrolled viral infection may itself contribute to CVD risk.45,46
CVD risk assessment and risk reduction are essential components of preventive medical care that are increasingly important for patients with HIV. Physicians should systematically assess their HIV-infected patients for CVR factors and should closely monitor patients receiving HAART, especially those with additional risk factors for CVD.47
The role of the cardiologist in the evaluation and treatment of patients with HIV infection should therefore be expanded to include patients who are being evaluated for or who are receiving HAART regimens, especially those with underlying CVR. It may be important to consider traditional coronary risk profiles and to alter those that can be modified in the evaluation and continued therapy of patients with HAART.48 It is especially important to develop simple and clear messages to educate patients about the importance of CVD prevention, the importance of identifying and treating CVD risk factors or high CVD risk, and how smoking, adverse dietary habits, and physical inactivity increase CVD risk.49
Treatment options include the use of pharmacological and non-pharmacological methods for managing dyslipidemia and hyperglycemia, as well as considering lipid-neutral HAART regimens for their patients, especially with the availability of drugs in this class with less adverse impact on lipid profile.47 One potential strategy to manage dyslipidemia is switching the ARV drug that promotes the lipids increase. However, it should be taken into consideration that it depends on the availability of remaining active drugs without impact on plasma lipids. In addition, switching requires a careful evaluation of the risks of virological failure, especially for patients with previous failure to ARV regimens.
Dyslipidemic HIV/HAART patients have elevated levels of lipoprotein-associated phospholipase A2 (Lp-PLA2). The main physiological action of Lp-PLA2 is the hydrolysis of strongly inflammatory phospholipids, such as platelet-activating factor which may increase risk of CVD.50,51 Elevated plasma Lp-PLA2 can be reduced by an intensive diet and exercise program in patients with HIV/HAART-associated dyslipidemia.51
Current guidelines recommend dietary intervention as first line treatment for HIV dyslipidemia.52,53 Omega-3 supplementation has a triglyceride-lowering effect that may impact on cardiac outcomes. Triglyceride levels represent an important biomarker of CVD, because of their association with atherogenic remnant particles. The 33,308 HIV-infected included in the study of Worm et al., with elevated triglyceride levels, experienced 580 MIs over 178,835 person-years. The risk of MI increased by 67%, per doubling in triglyceride level.54
Recently, Stradling et al. conducted a Systematic Review and Meta-Analysis which provides evidence for a comparable clinical benefit of dietary intervention or omega-3 supplementation in reducing triglycerides.55 Diet supplementation with fish oil is prescribed when a suppression of lipid mobilization is desired. The use of antihyperlipidemic drugs should be reserved for patients at high risk of cardiovascular events.56
Lifestyle changes (healthy diet, smoking cessation, and daily physical exercise) reduce the probability of a coronary event by up to 80% in the general population. Dietary, pharmacological interventions and exercise are established interventions to reduce metabolic changes and the relevant risk.56
Exercise is consistently listed among the three most common complementary and alternative therapies utilized by HIV-infected persons. A training program that involves concurrent endurance and strength training must be prescribed. Exercise aerobic should be performed at a moderate intensity: from 11 to 14 on the Borg Rating of Perceived Exertion Scale, or 50–85% of peak heart rate and resistance training should focus on large muscle groups, with intensity of 60–80% of one maximal repetition and 8–12 repetitions.56,57
A significant body of evidence suggests that there is a measurable increase in the risk of CVD in HIV-infected patients with varying effects from different antiretroviral drugs. In spite of studies, the impact of HIV and different HAART regimens on the risk of CVD in HIV-infected patients remains somewhat obscure. Differences in study design, endpoints, patient populations and limited follow-up in some studies prevent definitive comparisons.58
This review has several limitations, most of them due to the varying methodologies and study designs and inherent limitations of observational studies, which makes it difficult to control for population or selection bias. Furthermore, substantial variations in study design complicate the analysis of the associations between HAART and CVD risk. Considering its descriptive purpose and the findings of this review, it seems reasonable to believe that both HIV infection and HAART have potential adverse impact on CVR factors and on the incidence of CVD.
ConclusionThere are many studies addressing the relationship between HAART and CVD and it is an issue still under debate. However, it is clear that this combined antiretroviral therapy remarkably decreased the overall mortality associated with HIV infection. Our review confirms that HIV-infected patients present risk of CVD, and for this reason preventive strategies should be focused on smoking cessation, increase physical exercise, and diet.
Conflicts of interestThe authors declare no conflicts of interest.