A 19-year-old patient who mistakenly received two doses of influenza vaccine 10 days before presentation, was admitted with malaise, weakness, and a purpuric non-blanching rash most prominent on the ankles followed by abdominal pain and hematochezia 72h later. The diagnosis of influenza vaccine-related Henoch–Schonlein vasculitis was made. This complication, although rare, is the most common vasculitis related to immunization.
IgA vasculitis, or Henoch–Schonlein purpura (HSP), is a rare autoimmune disease that usually presents in the pediatric and teenage population. Development of HSP has been linked to viral and bacterial infections. A particular association with vaccination has also been documented. In particular, HSP has rarely developed after influenza vaccination. Although a benign outcome is usually the rule, HSP is the most common immunization-related vasculitis. We present a case of HSP that developed in a young man who received an unusually high dose of the influenza vaccine.
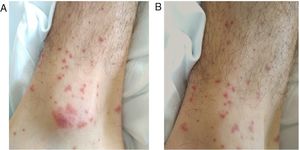
CaseA 19-year-old man presented in February to an emergency department in Houston, with a history of three episodes of vomiting for the last two days accompanied by headache, malaise and weakness. A purpuric rash on the extremities was noted which was not associated with pain, burning sensation or pruritus. Ten days before the start of symptoms, he received influenza vaccine which was administered twice in the same day; the initial dose was mistakenly administered subdermally, with an additional dose given intramuscularly. Two days after vaccination, the patient developed dry cough, rhinorrhea, malaise and diffuse myalgia. He only referred severe seasonal allergies as relevant past medical history. On the initial physical examination, he was well appearing, afebrile, and with normal vital signs. There was no oropharyngeal erythema, oral lesions or lymphadenopathy. A palpable non-blanching purpuric rash on the calves, knees and elbows (but most prominent on the ankles) was evident (Fig. 1). The rest of the physical examination was unremarkable.
The patient had leukocytosis (11,500WBC/μL) with 80% neutrophils and normal platelet counts (232,000platelets/μL). Urinalysis, creatinine and liver function tests were within normal limits; C-reactive protein was 7.4mg/dL (reference <3mg/dL). A respiratory viral panel, HIV ELISA, RPR, HBsAg and HCV antibodies were negative. Both chest X-ray and CSF analyses showed no abnormalities. C3 and C4 levels were decreased but the rest of the rheumatologic panel (anti-dsDNA, Anti-Ro, Anti-La, Anti-SM, Anti-RMP and antineutrophil cytoplasmic antibodies) was negative. After 72h in hospital, he developed abdominal pain, bloody diarrhea and left scrotal pain; testicular ultrasound showed mild varicocele and an abdominal CT scan showed thickening of the ascending colon walls. The patient received symptomatic pain management, along with one dose of intravenous methyl-prednisolone, followed by three additional doses of oral prednisone when the gastrointestinal bleeding resolved. He was discharged once the oral corticosteroid regimen was completed, as there was no recurrence of the gastrointestinal bleeding. The rest of the symptoms resolved within two weeks after hospital admission. At six months of follow up, the patient did not have any recurrence and never developed kidney dysfunction.
DiscussionBased on the clinical presentation, the presence of palpable skin purpura and diffuse abdominal pain with hematochezia, a clinical diagnosis of IgA vasculitis or Henoch–Schonlein Purpura (HSP) was made.1 This entity most commonly presents in children and adolescents and is caused by deposition of IgA–IgA antibody complexes in small blood vessels. Although the pathophysiology is not completely understood, the association with immunologic triggers such as infections or, as in our case, the administration of influenza vaccine, has been previously documented. In our case, the large antigenic trigger due to the unusual dose may have contributed to the development of the disease.
HSP associated with influenza vaccination usually occur within 21 days after administration and most patients (73%) are younger than 17 years-old.2,3 It is usually a self-limiting illness, although, secondary progression of pre-existent kidney disease has been reported.4 A recent descriptive analysis and systematic review of the literature reported that influenza vaccine was the most commonly associated vaccine with all types vasculitic events (up to 25% of cases) and HSP as the most frequent vasculitis presenting after any immunization (19% of reports).2,3
Finally, due to the obvious benefits of influenza vaccination, it is not recommended to limit this immunization to the general population. However, its safety in patients with prior diagnosis of vasculitis is still debatable.5
End noteAlexandre Malek, and Sara I. Gomez-Villegas contributed equally to this manuscript.
FundingThis work supported by NIH-National Institute of Allergy and Infectious Diseases grant number K24-AI114818 to CAA.
Conflicts of interestThe authors declare no conflicts of interest.