Infection control interventions can be erroneously interpreted if outcomes are assessed in short periods. Also, statistical methods usually applied to compare outcomes before and after interventions are not appropriate for analyzing time series.
AimsTo analyze the impact of a bundle directed at reducing the incidence of ventilator-associated pneumonia (VAP) and other device-associated infections in two medical-surgical intensive care units (ICU) in Brazil.
MethodsOur study had a quasi-experimental design. Interrupted time series analyses (ITS) was performed assessing monthly rates of overall healthcare-associated infections (HCAI), VAP, laboratory-confirmed central line associated bloodstream infections (CLABSI) and catheter-associated urinary tract infections (CAUTI), from January 2007 through June 2019. Moreover, multivariate ITS was adjusted for seasonality in Poisson regression models. An intervention based on a bundle for VAP prevention was introduced in August 2010.
FindingsThe intervention was followed by sustained reduction in overall HCAI, VAP and CLABSI in both ICU. Continuous post-intervention trends towards reduction were detected for overall HCAI and VAP.
ConclusionInterventions aimed at preventing one specific site of infection may have sustained impact on other HCAI, which can be documented using time series analyses.
In the past decade, the focus of infection control practice has switched from surveillance to interventions.1,2 The combined application of measures (collectively referred to as "bundles") aimed at prevention and control of healthcare-associated infections (HCAI) has been extensively studied.3–5
In this setting, there are concerns over the energy and time spent in applying simultaneously several bundles directed at different sites of infection.6 Furthermore, the successful results in some reports may have been biased by short-time post-intervention follow-up. Short-run results may imply statistical variations around the historical average.7 Finally, since monthly rates of HCAI are not independent among themselves, usual statistical tests (such as Chi-square, Student’s T and ANOVA) are not appropriate for detecting changes in incidence before and after interventions.8,9
Therefore, we studied the impact of a bundle aimed at preventing ventilator-associated pneumonia (VAP) on the incidence of overall and device-associated infections in adult medical-surgical intensive care units (ICU) in a Brazilian hospital.
MethodsStudy settingThe study was conducted in a 500-bed teaching hospital of Faculdade de Medicina de Botucatu (Botucatu Medical School). It is a tertiary-care reference hospital for a São Paulo inner-state area, Brazil, comprising approximately one million inhabitants. The hospital has five ICU, two of which are medical-surgical units for adult patients, with 17 and 10 beds. The study intervention was performed in those medical-surgical ICU.
Study designThis was a quasi-experimental (before and after) study.
InterventionIn August 2010, a bundle for preventing VAP was introduced in the two study units. The bundle included the following measures: (1) 30°–45° bed head elevation; (2) chlorhexidine mouthwash twice daily; (3) cuff pressure measurement twice daily; (4) keeping breathing circuits bellow the patients bed height; (5) whenever feasible, interrupt sedation for one hour daily. Several meetings with medical doctors and nursing staff were held in the two months preceding the intervention. Adherence to bundle items was checked twice weekly, on randomly chosen days. The intervention goal was to reduce VAP incidence bellow the median rates reported by São Paulo State HCAI surveillance system.10
HCAI surveillanceContinuous surveillance of HCAI in the ICU followed guidelines from the Brazilian National HCAI Surveillance Program.11 Minor variations on HCAI governmental definitions during the study were carefully analyzed by the authors, revising records of individual cases notified in active surveillance. Our conclusion was that they did have a relevant impact on results of the time series. It is also worth noting that, though largely based on Centers for Disease Control and Prevention’s (CDC) National Healthcare Safety Network (NHSN) definitions, Brazilian HCAI prevention program did not adhere to the “ventilator-associated events” surveillance, as recently recommended by the CDC.12
Descriptive statisticsPre- and post-intervention rates of HCAI (per 1000 patient-days, or patient days with devices) and device use (patient days with devices/overall patient days) were analyzed using the Chi-square test in the free software OpenEpi 3.03 (Emory University, Atlanta, GA, USA).
Time seriesTime series of overall and device-associated HCAI were analysed in two adult medical-surgical ICU from January 2007 through June 2019. Interrupted time series (ITS) was conducted using the “itsa” package in STATA 14 (Statacorp, College Station, TX, USA).13 We used multivariate Poisson regression models to adjust ITS for potential seasonality.
Ethical issuesThis study project was approved by the Committee for Ethics in Research from Faculdade de Medicina de Botucatu (Botucatu Medical School).
ResultsComplete adherence to the bundle was 53%. Adherence to specific items was above 80% in most surveillance instances, except for daily interruption of sedation. The ICU staff was reluctant to implement this measure, so adherence remained around 50%.
The overall HCAI rate during the study period was 37.71 per 1000 patient-days. The proportions of infectious sites were: VAP, 43.5%; bloodstream infection (BSI), 20.3%; catheter-associated urinary tract infection (CAUTI), 18.8%; other sites, 17.4%.
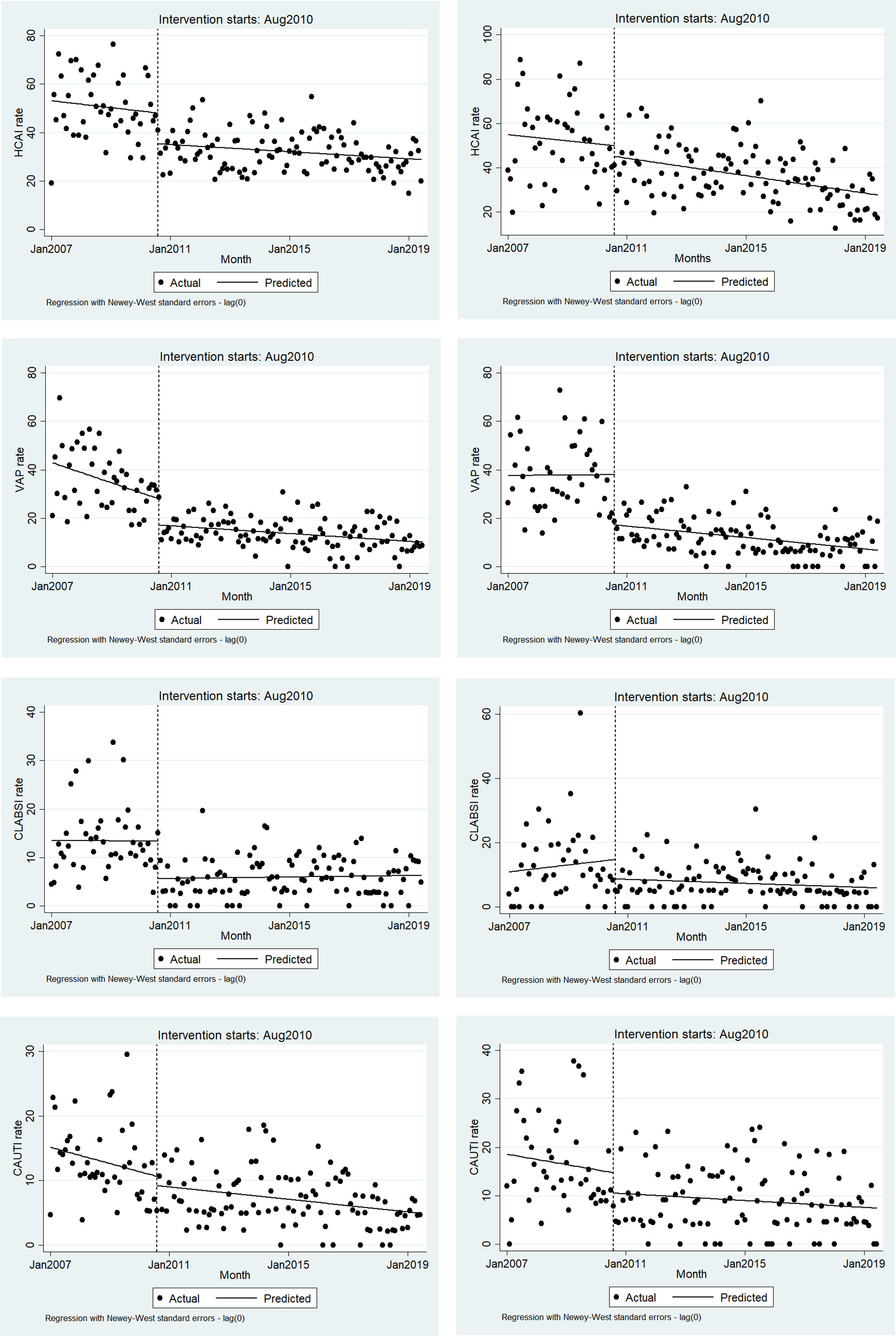
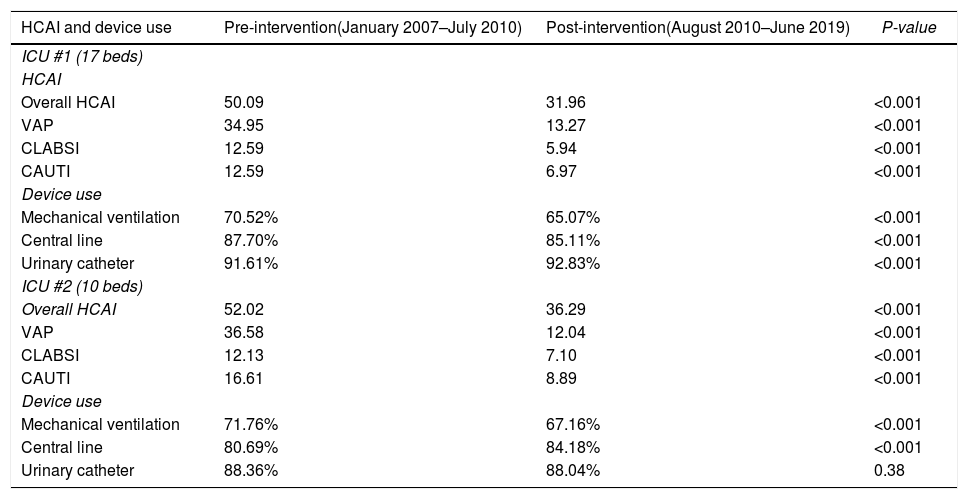
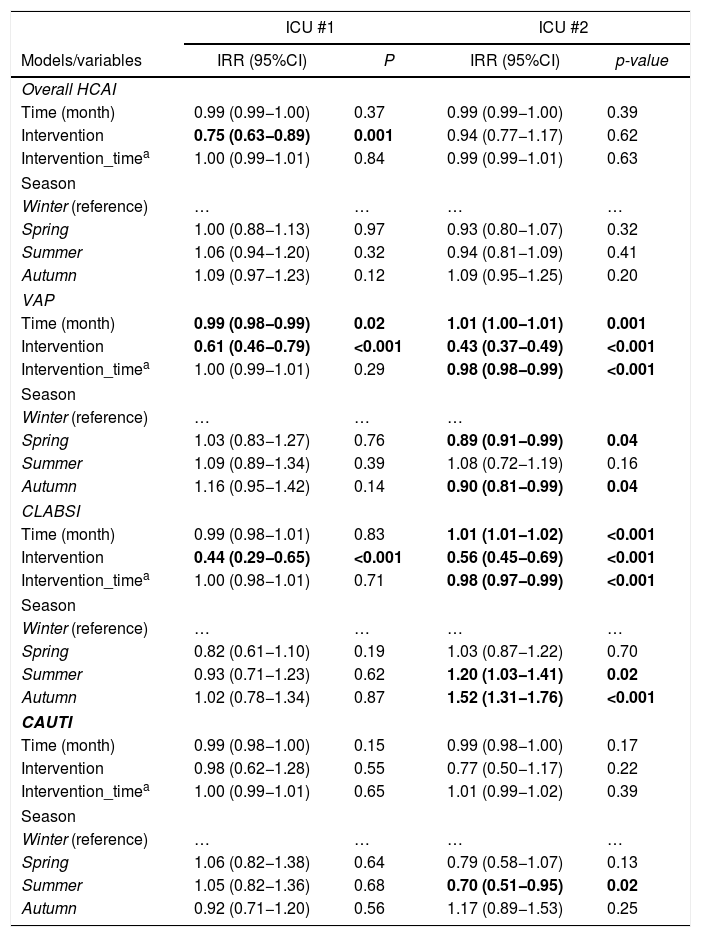
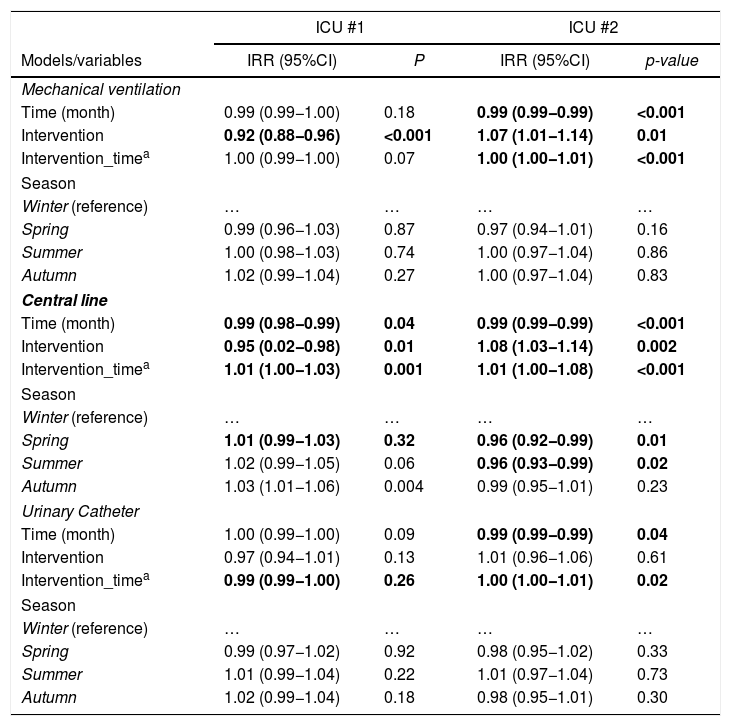
Pre- and post-intervention HCAI rates in the included ICU and use of invasive devices are presented in Table 1. It should be pointed out that the original goal of the VAP bundle was achieved in both ICU. Tables 2 and 3 present results from multivariate Poisson models of ITS for HCAI and use of invasive devices, respectively. Briefly, ITS models documented the impact of the intervention on overall HCAI (in ICU #1), VAP and BSI (in both ICU). The ITS graphics are presented in Fig. 1.
Rates of healthcare-associated infections in two intensive care units from a Brazilian teaching hospital, before and after the introduction of a bundle aimed at preventing ventilator-associated infections.
| HCAI and device use | Pre-intervention(January 2007–July 2010) | Post-intervention(August 2010–June 2019) | P-value |
|---|---|---|---|
| ICU #1 (17 beds) | |||
| HCAI | |||
| Overall HCAI | 50.09 | 31.96 | <0.001 |
| VAP | 34.95 | 13.27 | <0.001 |
| CLABSI | 12.59 | 5.94 | <0.001 |
| CAUTI | 12.59 | 6.97 | <0.001 |
| Device use | |||
| Mechanical ventilation | 70.52% | 65.07% | <0.001 |
| Central line | 87.70% | 85.11% | <0.001 |
| Urinary catheter | 91.61% | 92.83% | <0.001 |
| ICU #2 (10 beds) | |||
| Overall HCAI | 52.02 | 36.29 | <0.001 |
| VAP | 36.58 | 12.04 | <0.001 |
| CLABSI | 12.13 | 7.10 | <0.001 |
| CAUTI | 16.61 | 8.89 | <0.001 |
| Device use | |||
| Mechanical ventilation | 71.76% | 67.16% | <0.001 |
| Central line | 80.69% | 84.18% | <0.001 |
| Urinary catheter | 88.36% | 88.04% | 0.38 |
Note. HCAI expressed by 1000 patient-days, overall and with devices (mechanical ventilation for VAP; central line for CLABSI; urinary catheter for CAUTI). Device use expressed in proportion (patient-days with devices/total patient days).
HCAI, healthcare associated infections; ICU, Intensive Care Unit; VAP, ventilator associated pneumonia; CLABSI, central-line associated bloodstream infection; CAUTI, catheter-associated urinary tract infection.
Bold values signifies p < 0.05.
Multivariate Poisson regression models for Interrupted Time Series Analysis of the impact of the intervention (VAP bundle) on HCAI incidence in the two study ICU.
| ICU #1 | ICU #2 | |||
|---|---|---|---|---|
| Models/variables | IRR (95%CI) | P | IRR (95%CI) | p-value |
| Overall HCAI | ||||
| Time (month) | 0.99 (0.99−1.00) | 0.37 | 0.99 (0.99−1.00) | 0.39 |
| Intervention | 0.75 (0.63−0.89) | 0.001 | 0.94 (0.77−1.17) | 0.62 |
| Intervention_timea | 1.00 (0.99−1.01) | 0.84 | 0.99 (0.99−1.01) | 0.63 |
| Season | ||||
| Winter (reference) | … | … | … | … |
| Spring | 1.00 (0.88−1.13) | 0.97 | 0.93 (0.80−1.07) | 0.32 |
| Summer | 1.06 (0.94−1.20) | 0.32 | 0.94 (0.81−1.09) | 0.41 |
| Autumn | 1.09 (0.97−1.23) | 0.12 | 1.09 (0.95−1.25) | 0.20 |
| VAP | ||||
| Time (month) | 0.99 (0.98−0.99) | 0.02 | 1.01 (1.00−1.01) | 0.001 |
| Intervention | 0.61 (0.46−0.79) | <0.001 | 0.43 (0.37−0.49) | <0.001 |
| Intervention_timea | 1.00 (0.99−1.01) | 0.29 | 0.98 (0.98−0.99) | <0.001 |
| Season | ||||
| Winter (reference) | … | … | … | |
| Spring | 1.03 (0.83−1.27) | 0.76 | 0.89 (0.91−0.99) | 0.04 |
| Summer | 1.09 (0.89−1.34) | 0.39 | 1.08 (0.72−1.19) | 0.16 |
| Autumn | 1.16 (0.95−1.42) | 0.14 | 0.90 (0.81−0.99) | 0.04 |
| CLABSI | ||||
| Time (month) | 0.99 (0.98−1.01) | 0.83 | 1.01 (1.01−1.02) | <0.001 |
| Intervention | 0.44 (0.29−0.65) | <0.001 | 0.56 (0.45−0.69) | <0.001 |
| Intervention_timea | 1.00 (0.98−1.01) | 0.71 | 0.98 (0.97−0.99) | <0.001 |
| Season | ||||
| Winter (reference) | … | … | … | … |
| Spring | 0.82 (0.61−1.10) | 0.19 | 1.03 (0.87−1.22) | 0.70 |
| Summer | 0.93 (0.71−1.23) | 0.62 | 1.20 (1.03−1.41) | 0.02 |
| Autumn | 1.02 (0.78−1.34) | 0.87 | 1.52 (1.31−1.76) | <0.001 |
| CAUTI | ||||
| Time (month) | 0.99 (0.98−1.00) | 0.15 | 0.99 (0.98−1.00) | 0.17 |
| Intervention | 0.98 (0.62−1.28) | 0.55 | 0.77 (0.50−1.17) | 0.22 |
| Intervention_timea | 1.00 (0.99−1.01) | 0.65 | 1.01 (0.99−1.02) | 0.39 |
| Season | ||||
| Winter (reference) | … | … | … | … |
| Spring | 1.06 (0.82−1.38) | 0.64 | 0.79 (0.58−1.07) | 0.13 |
| Summer | 1.05 (0.82−1.36) | 0.68 | 0.70 (0.51−0.95) | 0.02 |
| Autumn | 0.92 (0.71−1.20) | 0.56 | 1.17 (0.89−1.53) | 0.25 |
Note. Statistically significant results are presented in boldface. ICU, Intensive Care Unit; IRR, Incidence Rate Ratio; CI, Confidence interval; HCAI, healthcare-associated infections; VAP, ventilator-associated pneumonia; CLABSI, central line-associated bloodstream infections; CAUTI, catheter-associated urinary tract infection.
Bold values signifies p < 0.05.
Multivariate poisson regression models for interrupted time series analysis of the impact of the intervention (VAP bundle) on use of invasive devices in the two study ICU.
| ICU #1 | ICU #2 | |||
|---|---|---|---|---|
| Models/variables | IRR (95%CI) | P | IRR (95%CI) | p-value |
| Mechanical ventilation | ||||
| Time (month) | 0.99 (0.99−1.00) | 0.18 | 0.99 (0.99−0.99) | <0.001 |
| Intervention | 0.92 (0.88−0.96) | <0.001 | 1.07 (1.01−1.14) | 0.01 |
| Intervention_timea | 1.00 (0.99−1.00) | 0.07 | 1.00 (1.00−1.01) | <0.001 |
| Season | ||||
| Winter (reference) | … | … | … | … |
| Spring | 0.99 (0.96−1.03) | 0.87 | 0.97 (0.94−1.01) | 0.16 |
| Summer | 1.00 (0.98−1.03) | 0.74 | 1.00 (0.97−1.04) | 0.86 |
| Autumn | 1.02 (0.99−1.04) | 0.27 | 1.00 (0.97−1.04) | 0.83 |
| Central line | ||||
| Time (month) | 0.99 (0.98−0.99) | 0.04 | 0.99 (0.99−0.99) | <0.001 |
| Intervention | 0.95 (0.02−0.98) | 0.01 | 1.08 (1.03−1.14) | 0.002 |
| Intervention_timea | 1.01 (1.00−1.03) | 0.001 | 1.01 (1.00−1.08) | <0.001 |
| Season | ||||
| Winter (reference) | … | … | … | … |
| Spring | 1.01 (0.99−1.03) | 0.32 | 0.96 (0.92−0.99) | 0.01 |
| Summer | 1.02 (0.99−1.05) | 0.06 | 0.96 (0.93−0.99) | 0.02 |
| Autumn | 1.03 (1.01−1.06) | 0.004 | 0.99 (0.95−1.01) | 0.23 |
| Urinary Catheter | ||||
| Time (month) | 1.00 (0.99−1.00) | 0.09 | 0.99 (0.99−0.99) | 0.04 |
| Intervention | 0.97 (0.94−1.01) | 0.13 | 1.01 (0.96−1.06) | 0.61 |
| Intervention_timea | 0.99 (0.99−1.00) | 0.26 | 1.00 (1.00−1.01) | 0.02 |
| Season | ||||
| Winter (reference) | … | … | … | … |
| Spring | 0.99 (0.97−1.02) | 0.92 | 0.98 (0.95−1.02) | 0.33 |
| Summer | 1.01 (0.99−1.04) | 0.22 | 1.01 (0.97−1.04) | 0.73 |
| Autumn | 1.02 (0.99−1.04) | 0.18 | 0.98 (0.95−1.01) | 0.30 |
Note. Statistically significant results are presented in boldface. ICU, Intensive Care Unit; IRR, Incidence Rate Ratio; CI, Confidence interval.
In recent years, HCAI have been recognized by the World Health Organization [WHO] as a major threat for public health, especially in developing countries.14,15 In our study, we faced the challenge of reducing VAP in a resource-limited and understaffed setting.16 Not surprisingly, our team encountered nihilistic attitudes from ICU staff. This challenge was managed with continuous education during visits of infection control nurses to the ICU to perform surveillance and measure adherence to the bundle.
The positive impact of bundles in preventing VAP (or, more recently, “ventilator-associated events”) has been reported by several authors,17–20 with few exceptions.21 The serendipity in our results was that improved surveillance for adherence to the bundle seemed to impact on the incidence of other HCAI. It is worth noting that there were no changes in policies for prevention of other device-associated infections during the study period.
Recent emphasis has been placed in socio adaptive approaches to improve adherence to infection control practices.22 Positive deviance, link nurses, behavioural economics and social network interventions have been tested, often with positive results.22–24 Our argument is that even simple measures which reinforce the presence and interaction of infection control team with other HCWs can improve safety culture, with widespread beneficial approach. Naturally, that interaction can be improved by more robust theory-laden approaches.22 One should notice that adherence to the whole bundle was only moderate, but we still achieved reduction in VAP and other HCAI rates. So, the bundle itself does not fully explain our results. We hypothesize a phenomenon similar to the so-called “surveillance effect”, in which adherence to a national surveillance system leads to decrease in HCAI incidence.25 In both cases, there is mobilization of infection control and other healthcare workers towards improving outcome indicators.
Our results also reinforce the importance of using ITS methods, instead of comparing “before and after” rates. The latter approach is suboptimal, since tests like Chi-square, Student’s t-test and others were developed for comparing independent variables, and adjacent time periods do not meet the criteria of statistic independence.8 Furthermore, impacts on time trends may be lost or even misunderstood.9 Finally, ITS requires long-term follow up, which is appropriate to identify sustainable impact of interventions.
As a secondary finding, there was evidence of seasonality for central-line associated bloodstream infection (CLABSI) in ICU #2, a finding in line with our previous studies.26,27 Finally, trends of use of invasive devices before and after the intervention may vary towards increasing or diminishing.
Our study has some limitations. First, over such a long period, it is evident that the infection control team performed continuous normative and educational measures, which possibly reinforced the prevention of HCAI. However, there was no other strong point intervention, so we believe that our premise that VAP bundle had a wide impact in infection control remains valid. Indeed, the continuous visits necessary for observing adherence to items of the bundle probably increased the proximity between infection control nurses and the ICU team. Second, we targeted the “old-fashioned” VAP, using diagnostic criteria often described as subjective.12 However, using this stable definition allowed us to study a long-term time series. Also, the impact of our intervention was noticed in the much more objectively defined CLABSI. Third, adherence to hand hygiene was continuously measured only after year 2016. This information was missing for most of the study period, and therefore could not be included in our model. Data on individual severity-of-illness was not included in the analysis. It should stressed that both hospital administrative data and information collected in previous studies from our group27 found no variation of severity-of-illness of patients in the evaluated ICU. Finally, the methodological design of this study shares the usual limitations of ecologic epidemiological approaches (mainly not adjusting for individual-based factors). Still, ecologic studies are the most appropriate methods for addressing collective exposures and/or interventions.28 Other strengths of our study include using ITS and the long-term follow up of the intervention. In developing countries, where structure for infection control is often suboptimal,15,29 intensification of interventions and the appropriate analysis of their results may be especially useful for improving patient safety.
In conclusion, we found that a partially successful implementation of a bundle aimed at reducing VAP resulted in long-term, positive impact on overall HCAI, VAP and CLABSI. Novel and continuous approaches may result in further improvement.
Conflicts of interestThe author declares no conflicts of interest.
MOS received a student grant from São Paulo State Research Foundation (FAPESP, grant #2015/06521-8), with CMCBF as her advisor.