Pulmonary complications are common among HIV-infected children. Early diagnosis and immediate care are important in order to reduce morbidity and mortality. Bronchoscopy with bronchoalveolar lavage (BAL) have been routinely used in the diagnostic approach of pulmonary complications caused by HIV-1.1,2
Due to immune defects, the risk of HIV-infected people to develop pneumonia is 10 to 100 times higher when compared to HIV-uninfected people. Infected patients present an increased susceptibility to pyogenic bacterial, viral, protozoal and mycobacterial infections and about 80% of them develop pulmonary disease more frequently and more severe.1,2
Bronchoscopy with BAL has been used in the diagnosis of these types of pneumonia in children and adults. Unlike lung biopsy, BAL is safe even in young infants, being less aggressive, and presenting less risk of complications.3
The aim of this study was to evaluate the importance of BAL to diagnose lung disease in HIV-infected children correlating epidemiology and laboratory data.
We retrospectively studied the microbiology and cytology data of BAL specimens performed by flexible bronchoscopy in HIV-infected children with pneumonia unresponsive to empiric antibiotic therapy, referred to the Respiratory Endoscopy Service at Antonio Pedro University Hospital – Universidade Federal Fluminense (APUH-UFF) from January 2000 to December 2009. Approval for this study was obtained from the APUH-FFU and Research Ethics Committee (CEP/HUAP/CAAE: 0178.0.258.000-10). Flexible bronchoscopy with BAL was carried out as previously described.3 The recovered lavage fluid was sent for microbiological (direct Acid Fast and Gram stain, and culture) and cytology (global and specific cytology) analysis. Using the protected catheter or quantitative culture can minimize the often contamination of the sample BAL when passing through the upper airway. We used quantitative culture in all study samples. 45 bronchoscopies were performed in 33 patients. Age ranged from 1 month to 16 years (median=4 years, interquartile range=1–6.5).
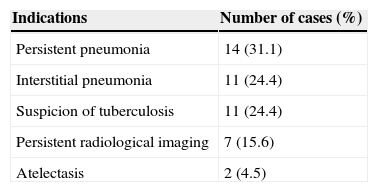
The indications for bronchoscopy with BAL are presented in Table 1. Ten children (four suspected of having tuberculosis (TB), three with pneumonia, two with persistent radiological imaging, and another with interstitial pneumonia) had bronchoscopic signs suggestive of TB (widening of carina and/or extrinsic compression of the tracheobronchial tree), one of them was confirmed by culture.
All bronchoscopy exams had a diffuse inflammatory process except one, with interstitial pneumonia which was normal. Cytological analysis in 12/45 (26.6%) of BAL showed neutrophilic (6/12), lymphocytic (4/12) and mixed cellularity, both neutrophilic and lymphocytic (2/12). The diagnosis was performed in 27/45 cases (60%): TB (15/45=33.3%), lymphocytic pneumonia (5/45=11.1%), bacterial infection (6/45=13.3%) and fungal infection (1/45=2.2%). The diagnostic yield of BAL in our study was 60.4%, similar to the literature (58%).
Pneumonia was the main indication (14/45=31.1%) for performing BAL, and this confirms the high frequency of lung disease in immunocompromised patients. Sheikh et al.2 studied 104 HIV-infected children and found that 75 (45.7%) had pneumonia with no complications, 24 (14.6%) recurrent pneumonia, and 18 (10.9%) persistent pneumonia.
Etiological confirmation of pulmonary diseases in HIV-infected children is crucial, since these patients often have severe infectious pulmonary complications that can cause death. Opportunistic bacteria, mycobacteria, viruses and fungi are pathogens that can be isolated, especially Staphylococcus aureus, Streptococcus pneumoniae, Pseudomonas aeruginosa, Haemophilus influenzae, Pneumocystis jiroveci and Streptococcus viridans.1,2,4
When there is strong clinical suspicion of bacterial infection, the specific isolation is not possible, but the presence of neutrophils in the BAL exceeding 30%, associated with high cellular count can be considered indirect evidence of the presence of infectious agent, justifying empiric antibiotic use. In the present study, bacterial infection was confirmed in six of 45 bronchoscopies (13.3%). Probably prior use of empiric antibiotics contributed to reduce the yield of the culture, which might have been a limitation of our study. However if we consider the presence of neutrophilic cellularity the yield of BAL will increase to 37.5%. Another limitation was the lack of viral studies.
The fungus most often present in HIV patients is Candida sp., same species isolated in one case of our study. Fungal infection is responsible for less than 1% of infections in these patients.
In children, the etiologic diagnosis of TB remains difficult to confirm. This disease presents nonspecific symptoms and radiological changes.4 In these cases, bronchoscopy with BAL is indicated because the procedure can detect abnormality in airway such as widening of the main carina, tracheobronchial tree extrinsic compression, bronchial fistula and caseum.4,5 Of the 15 cases (31.3%) suggestive of TB in this study, one had microbiological confirmation.
This study supported the high efficacy of bronchoscopy with BAL in diagnosing pulmonary diseases in HIV-infected children.
The presumptive diagnosis of TB should be considered when in the bronchoscopy there is bronchial involvement such as widening of the main carina, extrinsic bronchial compression, bronchial fistula or presence of caseum, regardless of the result of culture for Mycobacterium tuberculosis, especially in areas of high prevalence of TB. However, it is important to consider the World Health Organization diagnostic criteria before starting treatment.4
Conflict of interestAll authors declare to have no conflict of interest.