In the previous report, human co-infection cases of at least two respiratory viruses appeared as a rare event in symptomatic patients.1,2 However, at present the occurrence of multiple cases emerges as an increasing trend.3,4 In this study, from Apr 2010 to Mar 2012, the prevalence of human respiratory viruses every month was monitored for determining the aetiological role and epidemiological profile of every common respiratory virus among outpatients with acute respiratory tract infections (ARTIs) in Beijing. On the other hand, we put more attention in the co-infection cases increasing recently because of complicated clinical symptoms. Multivariable logistic-regression analysis was conducted to preliminarily explore some clinical risk factors associated with these co-infected cases.
Recruitment of outpatients with ARTIs at five hospitals (Chaoyang hospital, Dongfang hospital, Chuiyangliu hospital, Longfu hospital and Shunyiqu hospital) distributed in different districts of Beijing took place from Apr 2010 to Mar 2012. In order to include potential viral ARTIs and to exclude typical bacterial infections, patients enrolled in the study were selected by physicians according to the following criteria: with respiratory symptoms such as cough or wheezing, acute fever (body temperature≥38°C), and normal or low leukocyte count, with or without radiological pulmonary abnormalities. A total of 1791 throat swabs were collected and tested. The information of the subject's age, gender and presence of underlying diseases was collected during a face-to-face interview. Multiple PCR diagnostic kit for simultaneously detecting 12 pathogens of respiratory viruses (Hangzhou Neuro-Hemin Biotech Co., Ltd., China) was used to confirm the pathogen. The clinical features of the disease were closely monitored and summarized. Epidata software was used to store the dataset.
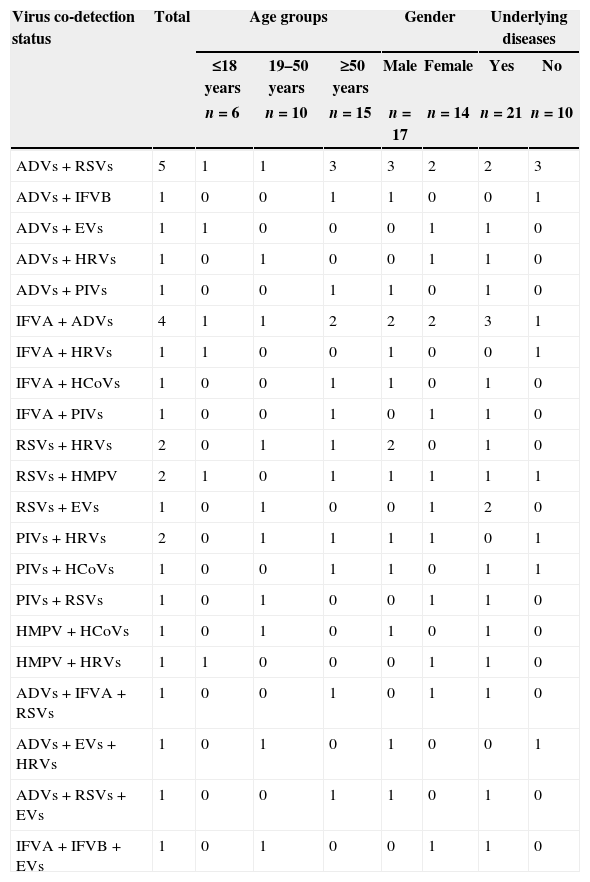
The overall positive rate of single respiratory virus in 1791 samples was 23.17%. Among the co-infected cases, multiple (≥2) respiratory viruses were observed in 31 cases (31/1791, 1.73%). Dual infections were present in 27 patients (27/1791, 1.51%), from which adenoviruses (ADVs) were co-detected in 9 cases, influenza viruses A (IFV A) in 7 cases, respiratory syncytial virus (RSV) in 5 cases, parainfluenza viruses (PIVs) in 4 cases and human metapneumovirus (HMPV) in 2 cases, and triple infections in 4 cases (4/1791, 0.22%). All co-infection cases are summarized in Table 1. Multivariable logistic-regression analysis identified independent risk factors for co-infection in relation to single viral infection: age of more than 50 years (odds ratio, 1.29; 95% confidence interval [CI], 1.08 to 1.57; p=0.031), and having an underlying disease (odds ratio, 1.67; 95% confidence interval [CI], 1.44 to 2.01; p=0.022). These data suggest that being more than 50 years and having and underlying disease are independent risk factors associated with co-infection among outpatients with acute respiratory tract infections (ARTIs) in Beijing. The widespread prevalence of respiratory viral co-infection in the elderly was higher than that in other age groups, and cases with underlying diseases.
Co-infection cases of respiratory viruses in subjects among different groups.
| Virus co-detection status | Total | Age groups | Gender | Underlying diseases | ||||
|---|---|---|---|---|---|---|---|---|
| ≤18 years | 19–50 years | ≥50 years | Male | Female | Yes | No | ||
| n=6 | n=10 | n=15 | n=17 | n=14 | n=21 | n=10 | ||
| ADVs+RSVs | 5 | 1 | 1 | 3 | 3 | 2 | 2 | 3 |
| ADVs+IFVB | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 1 |
| ADVs+EVs | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 |
| ADVs+HRVs | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 |
| ADVs+PIVs | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 |
| IFVA+ADVs | 4 | 1 | 1 | 2 | 2 | 2 | 3 | 1 |
| IFVA+HRVs | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 |
| IFVA+HCoVs | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 |
| IFVA+PIVs | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 0 |
| RSVs+HRVs | 2 | 0 | 1 | 1 | 2 | 0 | 1 | 0 |
| RSVs+HMPV | 2 | 1 | 0 | 1 | 1 | 1 | 1 | 1 |
| RSVs+EVs | 1 | 0 | 1 | 0 | 0 | 1 | 2 | 0 |
| PIVs+HRVs | 2 | 0 | 1 | 1 | 1 | 1 | 0 | 1 |
| PIVs+HCoVs | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 |
| PIVs+RSVs | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 |
| HMPV+HCoVs | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 |
| HMPV+HRVs | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 |
| ADVs+IFVA+RSVs | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 0 |
| ADVs+EVs+HRVs | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 1 |
| ADVs+RSVs+EVs | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 |
| IFVA+IFVB+EVs | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 |
ADVs, adenoviruses; EVs, enteroviruses; HCoVs, human coronaviruses; HMPV, human metapneumovirus; HRVs, human rhinoviruses; IFVA, influenza A virus; IFVB, influenza B virus; PIVs, parainfluenza viruses; RSVs, respiratory syncytial viruses.
This survey provides some evidence for respiratory viral co-infection and the risk factors among outpatients with ARTIs. The clinical significance of such co-detection is unclear.5 Multiple viruses add to the complexity of the clinical symptoms making the clinical diagnosis more difficult. Further research is warranted among co-infected cases throughout other regions of China in order to fully understand risk factors among outpatients in China.
Conflict of interestAll authors declare to have no conflict of interest.
We would like to thank Prof. Jianwei Wang for total guidance. This study was funded by two Program of China during the 12th Five-Year Plan Period, the National Major Science and Technology Research Project for Control and Prevention of Major Infectious Diseases of China (2012ZX10004206-002) and the Nation Key Program for Infectious Disease of China (2012ZX10004215-003-001).