As of August 30, 2020, Brazil ranked second among countries with the highest number of COVID-19 cases, with the city of São Paulo as the national epidemic epicenter. Local public healthcare institutions were challenged to respond to a fast-growing hospital demand, reengineering care provision to optimize clinical outcomes and minimize intra-hospital coronavirus infection. In this paper we describe how the largest public hospital complex in Latin America faced this unprecedented burden, managing severe COVID-19 cases while sustaining specialized care to patients with other conditions. In our strategic plan a 900-bed hospital was exclusively designated for COVID-19 care and continuity of care to those not infected with coronavirus ensured in other inpatient facilities. After 152 days, 4241 patients with severe COVID-19 were hospitalized, 70% of whom have already been discharged, whereas the remaining Institutes of the complex successfully maintained high complexity inpatient and urgent/emergency care to non-COVID-19 patients.
On March 11, 2020, the World Health Organization (WHO) declared COVID-19 a pandemic1 and since then it has taken an unprecedented course. As of August 30, 24,854,140 COVID-19 cases and 838,924 related deaths were reported worldwide.2 On the same date, Brazil ranked second among countries with the highest number of officially confirmed SARS-CoV-2 infections globally, with 3,804,803 reported cases,2 and yet this may well be underscored.
With a population estimate of 12,325,232 inhabitants in 2020,3 São Paulo, Brazilian largest city, is ranked among the most populous megacities in the world. In such a demographic scenario facing the COVID-19 pandemic would certainly be a public health challenge. Indeed, São Paulo was soon recognized as the national epicenter of the epidemic, leading to the declaration of a statewide quarantine on March 21.4
In this context, similarly to what was previously experienced in foreign health systems or academic health centers,5,6 public healthcare institutions in Brazil were challenged to respond to a fast-growing hospital demand to cope with the need to provide inpatient care for severely ill individuals with a life-threatening contagious condition.
Such a hard undertaking required a thorough reengineering of long consolidated practices with flexible adaptations of services in terms of routine governance, workflows, and task responsibilities.
Our institution was no exception in this scenario. Hospital das Clinicas is the largest public hospital complex in Latin America. Affiliated to the Faculty of Medicine of the University of São Paulo academic health system and located in the central area of São Paulo, it comprises eight specialized Institutes (Central, Heart and Pneumology, Orthopedics, Psychiatry, Children, Cancer, Rehabilitation, and Radiology) and has 2400 beds altogether. At this setting, healthcare is provided as part of the national unified public health system framework (Sistema Único de Saúde – SUS), with the specific task of undertaking high complexity care within the hierarchical distribution of responsibilities among health services. Our workforce comprises 20,000 employees, including multi-professional healthcare and support teams. Moreover, being part of an academic health center, Hospital das Clinicas hosts the largest medical residency program in the country, with 1664 physicians under training in academic programs that cover all nationally-accredited medical specialties, as well as 360 senior medical students in hospital internship rotations in 2020.
It is noteworthy to mention that in 2013 an institutional Crisis Management Committee was established at the hospital with the aim of putting together a disaster plan, based on the methodology proposed by the California Emergency Medical Services Authority (EMSA) and consolidated in the Hospital Incident Command System (HICS).7 The plan can be activated whenever there is a need to respond fast to emergencies or even to non-emergency situations in which healthcare demand is predicted to far exceed our regular provision capacity, conditions fully met by the COVID-19 pandemic.
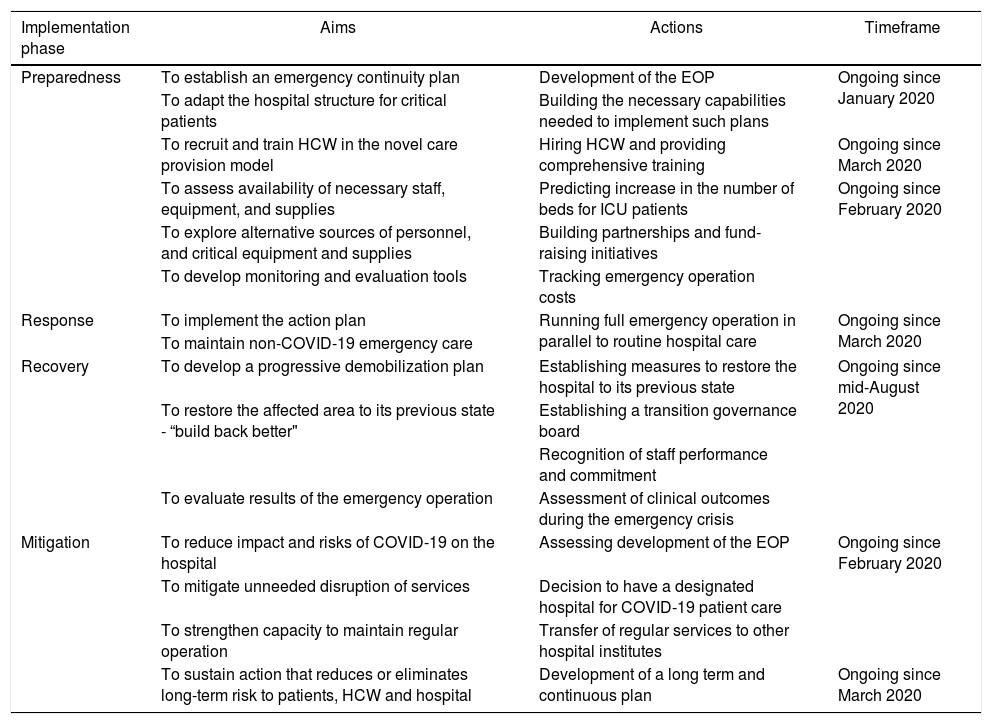
On January 30, 2020, the Crisis Management Committee was therefore activated, approximately one month before the very first COVID-19 case was actually reported in the city of São Paulo. The Committee, run by four medical doctors with large experience in disaster management, developed a strategic Emergency Operational Plan (EOP) to be carried out in four subsequent phases, namely, preparedness, response, recovery, and mitigation, as described in Table 1.
Strategic Emergency Operational Plan (EOP) designed for the COVID-19 response. Hospital das Clinicas, São Paulo, Brazil, 2020.
| Implementation phase | Aims | Actions | Timeframe |
|---|---|---|---|
| Preparedness | To establish an emergency continuity plan | Development of the EOP | Ongoing since January 2020 |
| To adapt the hospital structure for critical patients | Building the necessary capabilities needed to implement such plans | ||
| To recruit and train HCW in the novel care provision model | Hiring HCW and providing comprehensive training | Ongoing since March 2020 | |
| To assess availability of necessary staff, equipment, and supplies | Predicting increase in the number of beds for ICU patients | Ongoing since February 2020 | |
| To explore alternative sources of personnel, and critical equipment and supplies | Building partnerships and fund-raising initiatives | ||
| To develop monitoring and evaluation tools | Tracking emergency operation costs | ||
| Response | To implement the action plan | Running full emergency operation in parallel to routine hospital care | Ongoing since March 2020 |
| To maintain non-COVID-19 emergency care | |||
| Recovery | To develop a progressive demobilization plan | Establishing measures to restore the hospital to its previous state | Ongoing since mid-August 2020 |
| To restore the affected area to its previous state - “build back better" | Establishing a transition governance board | ||
| Recognition of staff performance and commitment | |||
| To evaluate results of the emergency operation | Assessment of clinical outcomes during the emergency crisis | ||
| Mitigation | To reduce impact and risks of COVID-19 on the hospital | Assessing development of the EOP | Ongoing since February 2020 |
| To mitigate unneeded disruption of services | Decision to have a designated hospital for COVID-19 patient care | ||
| To strengthen capacity to maintain regular operation | Transfer of regular services to other hospital institutes | ||
| To sustain action that reduces or eliminates long-term risk to patients, HCW and hospital | Development of a long term and continuous plan | Ongoing since March 2020 |
HCW: healthcare workers; Source/Notes: SOURCE – authors, adapted from California Emergency Medical Services Authority.5
For its governance, the plan encompasses five major functional areas: command, operation, planning, logistics, and finance/administration, under the responsibility of skilled staff members. Achievable expectations were established for its development, as well as continuous progress assessment using measurable outcomes. It was also necessary to guarantee enough flexibility to allow alternative settlements for a better strategic and tactical response to an expected dynamically changing situation. Our ultimate objective with this institutional initiative was to ensure preservation of as many lives as possible.
Few local adaptations in the HICS framework were required for the COVID-19 crisis, the most important being the Institutional commander’s scope of authority, which was shared among three full professors (Clinical director, Vice-clinical director and Infectious disease specialist), who were integrated into the incident management process with strategic hands-on activities. The Hospital Superintendence, in charge of its administrative governance, played a relevant role in the process, interacting with governmental stakeholders (São Paulo State Health Department - SES), who financed the plan, and giving logistical support to provision of appropriate medical equipment and supplies, in exceptional amounts as compared to our regular operation needs. It also coordinated complementary fund-raising efforts that led to successful donations being obtained from societal partners. Moreover, the medical school dean was instrumental in facilitating communication with all full professors of Faculty of Medicine, who act as institutional academic leaders and heads of health services at the hospital within their fields of expertise. Members of the institutional Crisis Management Committee fully understood the need to keep all stakeholders, despite having to move beyond their comfort zones, ae to the emergency plan to enhance its chance of success.
A major challenge to the EOP, however, was how to build a minimally safe strategy to allow the academic health system to continue providing urgent/emergency tertiary care and management of relative urgencies for non-COVID-19 cases, simultaneously to the compelling need to establish specialized care units for COVID-19 patients in the same hospital building.
The best model we could conceive to reconfigure our hospital operation in order to meet the needs of this public health emergency was to physically isolate the Central Institute, an 11-floor building with 900 hospital beds, to become entirely and exclusively designated to COVID-19 care. A similar experience was previously reported by He et al.8 at the Wuhan Red Cross Hospital, a 15-floor general hospital in the Chinese province of Hubei, cradle of the COVID-19 pandemic.
The specific goals of our initiative were multiple: (1) to maximize favorable outcomes in the management of COVID-19 patients, by establishing standardized clinical protocols, to be followed in all inpatient wards and ICUs, as well as specialized supervision teams, composed by skilled personnel to support frontline healthcare workers (HCW) in specific tasks, such as advanced airway access, catheters’ insertion, pronation, tracheostomy, and kidney replacement therapy; (2) to reduce the risk of inpatients with other diseases from getting infected with coronavirus; and (3) to avoid mobility of HCW between the Central Institute (area of high exposure to COVID-19) and the other hospital facilities in the complex. This endeavor required an overly complex preparation, since at the time the decision to turn the Central Institute into a designated hospital was taken, it had approximately 400 non-COVID-19 inpatients, 85 of whom under intensive care. Furthermore, this Institute hosts the busiest highly specialized tertiary Emergency Department (ED) in the city of São Paulo that accounts for 42,000 medical emergency visits and 14,000 admissions per year.
Such an audacious plan was implemented in two weeks, even though it required reallocation of the multidisciplinary ER (including Internal Medicine, Neurosurgery, Neurology, Gastroenterology, General Surgery, Vascular Surgery, Liver transplantation and Kidney transplantation) to the Emergency Department of the Heart Institute (InCor). The sharp reduction in the number of ER visits that occurred right after quarantine was established in the city allowed these specialized groups to get adapted to the new care provision model. It is important to highlight that such a vast and complex operational change required not only infrastructure adaptations in the ER at the Heart Institute, but also in its inpatient wards and ICUs.
In order to make the Central Institute a reference center for healthcare to women with suspected or confirmed COVID-19, we transferred our gynecology and obstetrics ER to a secondary hospital, located on the main campus of the University of São Paulo (Hospital Universitário).
In addition, 21 inpatient wards of the different medical specialties were reallocated into the Orthopedic, Psychiatric, Children, and Cancer Institutes, and once more, the virus-imposed decrease in number of hospitalized patients with other diseases provided the right setting to accommodate these groups in their new environment.
Multidisciplinary healthcare personnel had also to be divided into teams that would work exclusively either in the Central Institute or in the other buildings of the hospital complex (Institutes with low exposure to COVID-19). The main criterion for this HCW distribution was to keep people at higher risk of developing severe COVID-19, based on age and existing comorbidities, in low-exposure Institutes. Approximately 60% of the workforce fulfilled this condition, what led to the urgent need to hire new personnel for COVID-19 care.
In order to reduce intra-hospital coronavirus infection, screening rules for flu-like symptoms were established for both employees and patients when entering hospital facilities of all Institutes. For HCW with low suspicion of COVID-19, a mandatory immediate 3-day leave was given, with recommendation for a follow-up medical visit on day 4. In contrast, those with sustained symptoms for longer than three days were submitted to a nasopharyngeal swab collection and RT-PCR testing for SARS-CoV-2. If tested positive for viral RNA, they were kept on leave until day 14 after symptom onset. Patient screening when entering the outpatient clinic buildings was based on a specially designed questionnaire to assess COVID-19 symptoms (fever, cough, sneezing, and difficult breathing) in the previous 14 days. In case any of these symptoms was reported, patients would be referred to a special area in the outpatient building for clinical evaluation and proper management. In addition, suspected or confirmed cases of COVID-19 were prioritized to be transferred from any of the low exposure Institutes to the Central Institute.
At the onset of the EOP implementation, we agreed with the State Health Department (SES) to provide 200 ICU beds and 700 ward beds solely for the care of severe COVID-19 patients. This required an initial expansion of our capacity in 115 ICU beds, which occurred in 4 weeks. This first step was possible with the full support received from state health officials, which allowed rapid activation of an already existing project to expand our ICU capacity with additional governmental funding. Later in the process, we were requested to scale it further up to 300 ICU and 500 ward beds, initiative currently underway.
The occupation process of the COVID-19 designated Institute required transformation of administrative rooms into support areas, such as sleeping and dressing rooms and pantry, and opening of training space for newly hired HCW and setting up of on-site simulation stations.
To support this exceptional demand for inpatient care, 700 medical residents, affiliated to 41 different specialty training programs, were also reallocated to COVID-19 wards and ICUs, under the supervision of skilled physicians (infectious disease, pneumology and internal medicine specialists), with additional technical support of anesthesiologists with airway and prone position management expertise. As reported by Miethke-Morais et al.,9 backing residents up to cope with stressful clinical situations they were not used to face in everyday practice contributed to increase their motivation to engage in the institutional effort to provide high-quality COVID-19 care. In order to bring medical students on board while maintaining them off the COVID-19 inpatient care frontline, we invited them to join a broad range of voluntary activities that addressed needs of patients and their families and supported the healthcare team in actions related to health education, clinical research or fund-raising initiatives.10
After 152 operation days under this new care provision model, we can conclude it was extremely positive. All low-exposure Institutes were able to maintain high complexity tertiary inpatient care and urgent/emergency care to non-COVID-19 patients. In this context, for instance, 44 liver and 36 kidney transplants were successfully performed by their respective multi-professional teams in the newly assigned Institute in this period, demonstrating that even highly specialized healthcare could be sustained in spite of the necessary service reallocation due to the epidemic.
Localized COVID-19 outbreaks in the rearranged low-exposure institutes, though expected due to the fact that community transmission of the novel coronavirus is currently established in the city of São Paulo and to the high contagiousness of this infection, are being successfully contained with active surveillance, patient and HCW testing and isolation measures by our Hospital Infection Control team.
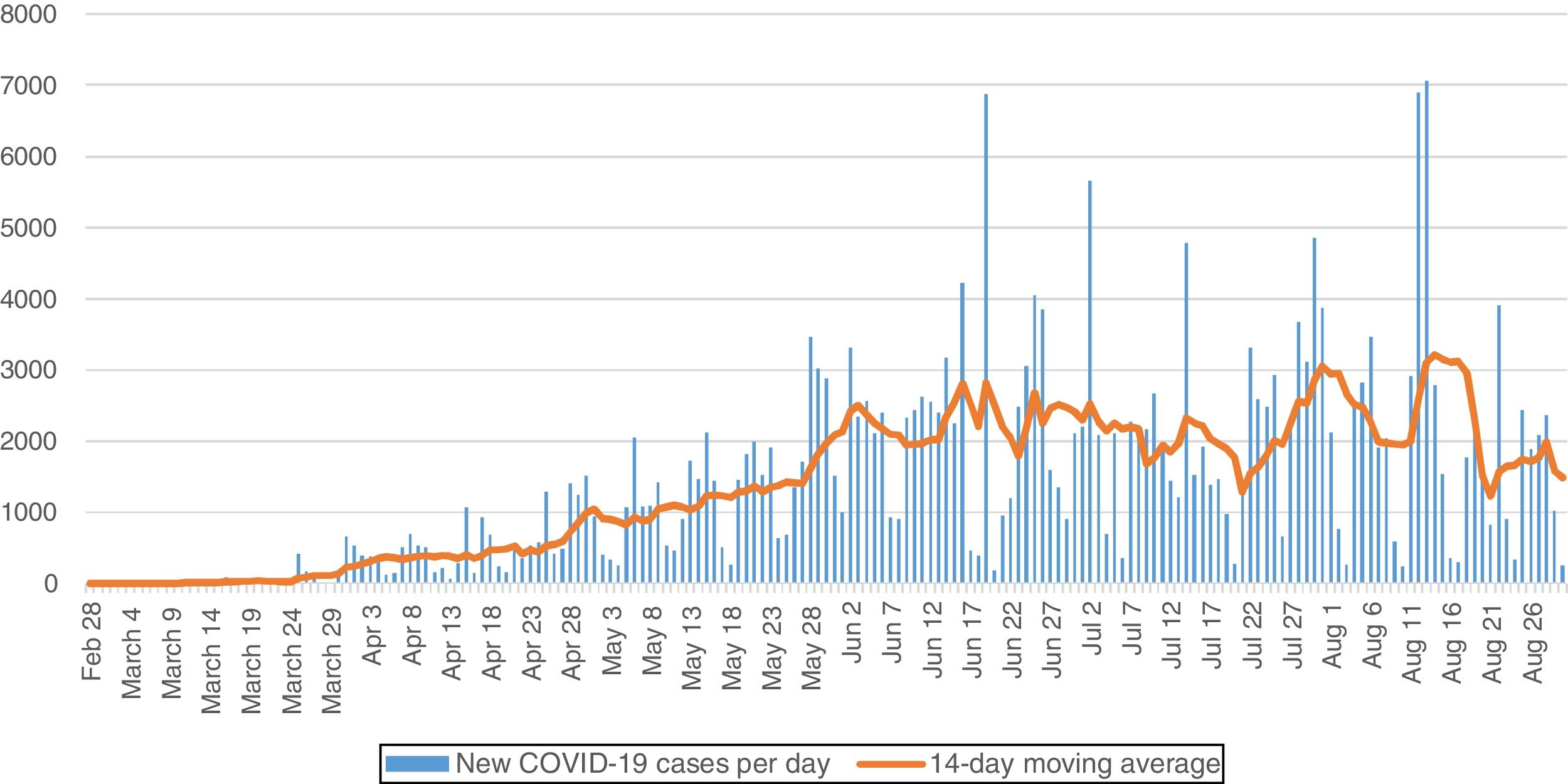
The COVID-19 epidemic in the city São Paulo is still underway.11 Even though recent epidemiological reports show a reduction in the incidence of the disease (Fig. 1), the emergency operation at our hospital is not concluded. In terms of overall results, it should be highlighted that from March 30 to August 30, 2020 4241 COVID-19 severely ill patients were admitted to the Central Institute, after referral through the state urgency/emergency regulation network, and approximately 70% of these have already been discharged after recovery. In this timeframe, Hospital das Clinicas has been the second hospital in number of hospitalized COVID-19 patients in the city, being only surpassed by Hospital Estadual de Campanha COVID-19 Ibirapuera, a field hospital set up by the state health department as an alternate care delivery facility for the COVID-19 emergency response. However, our patient profile differed significantly from that seen in that setting, where basically only mild cases were admitted. As such, Hospital das Clinicas accounted for the largest number of ICU admissions due to COVID-19 in the state of São Paulo.
COVID-19 confirmed cases. São Paulo city, São Paulo, Brazil, February-August 2020.
Source/Notes: SOURCE – Fundação SEADE.11 Bars show number of new COVID-19 confirmed cases per day. Line shows 7-day moving average of new COVID-19 confirmed cases.
Throughout the operation, the overall mortality rate of COVID-19 patients in our hospital remained stable, around 30%, which could be considered a very favorable outcome, given the severe disease presented by our hospitalized patients. Among those who required intensive care (50% of cases), 80% needed orotracheal intubation and mechanical ventilation, and their mortality rate was 41%.
So far, 13% of our 20,000 employees had COVID-19 infection confirmed by PCR, whereas 41% of the workforce went on sick leave due to flu-like symptoms in the same period. Interestingly, the rate of infection among HCW was not higher in the COVID-19 designated Institute as compared to the low exposure hospital buildings.
In summary, we conclude that upfront organized planning as a preparedness measure can be effective when facing public health emergencies, such as the COVID-19 epidemic, in a middle-income country. Our experience suggests that having a large hospital building physically isolated to provide exclusive care to inpatients with COVID-19 was a remarkably effective measure that helped standardize care provision to a significant number of patients, leading to favorable clinical outcomes. Furthermore, we were able to reduce intra-hospital viral spread and cross-infection of patients and HCW providing care for non-COVID-19 in. and outpatients, a need not always met elsewhere in Brazil and in other countries experiencing the coronavirus pandemic crisis. Finally, it provided a higher awareness of infection risk for those working in the COVID-19 designated Institute, giving them the chance of improving their individual protection skills with appropriate training.
Conflict of interestAll authors declare that they have no conflict interests.
FundingThis research did not receive any specific grant from funding agencies in the public, private or non-for-profit sectors.