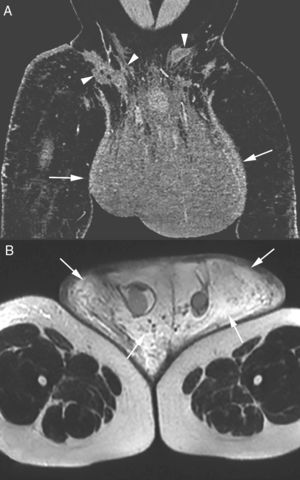
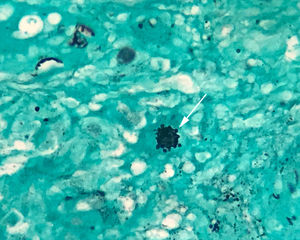
A 42-year-old black male, Brazilian farmworker presented with pain and progressive swelling of the scrotum for three years. He also had lower-limb edema, enlarged lymph nodes of the right groin, neck, and sternal furcula. A cervical lymph-node biopsy showed non-specific chronic inflammation. Serologies, including HIV, were negative. The nodule in the right groin increased in volume and gave rise to fistulization and purulent discharge. A chest X-ray was normal. Physical examination revealed a very enlarged scrotum with thickening of the skin and purulent discharge (Fig. 1). Computed tomography (Fig. 2A) and pelvic magnetic resonance imaging (Fig. 2B) showed a very enlarged scrotum with extensive subcutaneous thickening, and inguinal lymphadenopathy with multiple fistulous tracts in the skin. The left testicle had a reduced size, without testicular expansive lesions, and there was also bilateral hydrocele. Lymphoscintigraphy revealed an obstructive process in the inguinal region suggesting lymphatic involvement. The biopsy specimen of the right inguinal skin showed the “ship's wheel” appearance of yeast forms budding from the central parent yeast on silver stain, consistent with paracoccidioidomycosis (PCM) (Fig. 3). Serology for Paracoccidioides brasiliensis, based on double radial immunodiffusion test, was reagent (1:64). The patient was treated for 21 days with liposomal amphotericin B, followed by one-year treatment with oral trimethoprim/sulfamethoxazole (TMP/SMX). The patient remains on treatment. Later, a scrotoplasty was also performed.
Post-contrast coronal computed tomography of the pelvis (A) showing isodense scrotal enlargement (arrows) with multiple fistulous tracts (arrowheads) in the right inguinal region. T2-weighted magnetic resonance image of the pelvis (B) showing hyperintense scrotal enlargement due to significant subcutaneous edema (arrows).
Clinical features of involvement of the genital tract in PCM are very rare and occur in the disseminated chronic form. Urogenital involvement is thought to result from hematogenic dissemination, usually described in late-stage disease and associated with lesions in other organs, along with pulmonary PCM.1–4 The main affected sites are the epididymis, prostate, testicle, penis, and scrotal pouch. Testicular, epididymal, and prostatic lesions are usually misdiagnosed as neoplasms. Lesions on the external genitalia appear as ulcers or vegetations, and sexually transmitted diseases are important components of the differential diagnosis.2,3 In conclusion, in endemic areas, the differential diagnosis of a systemic disease with lymphadenopathy and scrotal involvement should include PCM.
FundingNone declared.
Conflicts of interestThe authors declare no conflicts of interest.