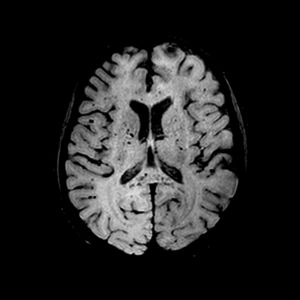
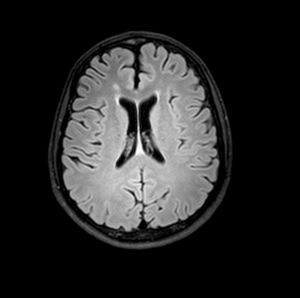
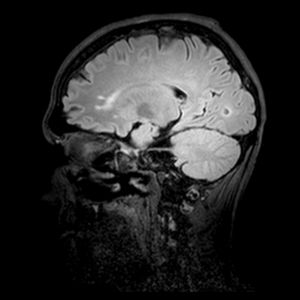
A 19-year-old male presented with asthenia, abdominal pain, vomiting, fever, jaundice, and rash. The patient quickly progressed to severe shock, purple lower limbs and toes necrosis. The diagnosis of Rickettsia spp (gene regions surveyed gltA (TaqMan) and internal control of the human RNAse P reaction) was made by PCR (polymerase chain reaction) of serum sample. Serial serology, with indirect immunofluorescence, also turned out positive with increasing IgG titers, initially <1/64 and then >1/256 two weeks later. The patient went on to present nystagmus and conjugate eye deviation. Magnetic resonance imaging (MRI) identified: multiple foci of marked hypointensity on susceptibility weighted imaging (SWI), evidenced in the corpus callosum, deep white matter, bilateral basal ganglia, thalamus and middle cerebellar peduncles, compatible with hemosiderin deposits, possibly petechial hemorrhages (Fig. 1). Foci of hyperintensity were observed on T2/FLAIR weighted images in the semiovale centrum, deep white matter and periventricular regions (Figs. 2 and 3). The patient was treated with chloramphenicol but progressed with extremity necrotic lesions, requiring bilateral transmetal amputation of toes and at the proximal phalanx of second, third, fourth, and fifth fingers of the right hand. He was discharged after 55 days of hospitalization for outpatient follow-up.
Magnetic resonance axial SWI (Susceptibility weighted imaging), at the level of the basal ganglia, shows multiple hypointense foci suggestive of petechial hemorrhages or possibly microthrombi in the white matter (subcortical and within the corpus callosum) and internal capsules and basal ganglia.
Rocky mountain spotted fever in Brazil still has high mortality rates (20–30%) when compared to other countries. It is an acute febrile infectious disease, caused by a Gram-negative coccobacillus of the Rickettsia genus (obligate intracellular bacterium), usually transmitted by infected tick bites. Early diagnosis and treatment are essential to avoid more severe forms of the disease, including neurological involvement.1
Dissemination to the central nervous system (CNS) occurs by hematogenous spread, with invasion of arterioles and capillaries, leading to inflammation and rupture of the blood–brain barrier. The possible findings on MRI include meningeal enhancement, varying degrees of swelling and periventricular and subcortical infarction, secondary to vasculitis, which tend to occur in a perivascular distribution, as observed in this case (which can mimic demyelinating disease).2,3 The CT scans of the head can be normal or show diffuse white matter changes, sulcal effacement and/or focal hypodensities consistent with infarctions.4 However, MRI is the exam that better characterizes CNS involvement in this entity, evidencing both multifocal hemorrhages and the foci of white matter changes due to vasculitis.
Considering that perivascular inflammatory response is the most important pathophysiology aspect of Rocky Mountain spotted fever vasculitis, similar CNS MRI findings have been described in other infectious diseases also known to cause perivascular inflammation, such as cryptococcosis and Lyme disease encephalitis.5,6
Conflicts of interestThe authors declare no conflicts of interest.