The burden of dengue in Brazil is poorly documented and is based on data from the public health care setting. This study estimated the prevalence and costs of dengue management in the private health care system in Brazil from 2015 to 2020 using a large claims database from Orizon.
MethodsWe selected claims with dengue ICD codes (ICD-10 A90 or A91) from January 2015 to December 2020. Prevalence was estimated based on the population enrolled in health insurance plans in the given year. Costs were adjusted for the inflation up to December 2021 and evaluated by measures of central tendency and dispersion.
ResultsA total of 63,882 unique beneficiaries were included, with a total of 64,186 dengue cases. The year with the highest prevalence was 2015 (1.6% of patients who used health plans), and there was also an increase in cases in 2016 and 2019. The median cost per hospitalization in 2015 was US$486.17, and in 2020, it reached US$696.72. The median cost of a case seen at an emergency room ranged from US$ 97.78 in 2015 to US$ 118.16 in 2017.
ConclusionsThe estimated prevalence of dengue in this population of private health-insured patients followed the epidemiological trends of the general population in Brazil, with the highest rates in 2015, 2016, and 2019. The cost of dengue management has increased in the private health care setting over the years.
Dengue is a mosquito-borne infection caused by four different serotypes (DENV -1 to 4) and represents a serious public health problem in almost all tropical and subtropical countries.1,2 The clinical spectrum of dengue ranges from mild, self-limiting forms, to severe conditions that often require hospitalization and high-cost support measures, such as transfusions and intensive care.1,3 Data on the impact and costs related to dengue are crucial for designing public health policies and conducting a cost-benefit evaluation of preventive measures.
Brazil is the country with the highest number of dengue cases in the world.4 In 2020, 1,467,142 cases were reported to the SINAN (National Disease Notification System).5 Among these, 828 cases were classified as severe, resulting in 554 deaths.5 As with any passive reporting system, these numbers are known to underestimate the real burden of the disease. Thus, it is estimated that, in epidemic periods, for each reported case of dengue, 12 are not identified.6 Regarding the hospitalization rate, the available data are even scarcer. Coelho et al. demonstrated the low sensitivity of the dengue surveillance system in detecting hospitalized dengue cases through a linkage between SINAN and the National Hospital Information System (SIH),7 which is an administrative database holding data on hospitalizations in the public health network as well as for affiliated private hospitals. Only 50% of hospitalizations due to dengue recorded in the SIH were reported to SINAN.7
According to the National Supplementary Health Agency, in 2021, approximately 25% of the country's population had private medical/hospital insurance.8 The majority of beneficiaries receive private health insurance through their employers as a benefit.9 Despite the relevant role of private health care as a complement to the health system, data on hospitalizations due to dengue in this population are still rare, mainly because of underreporting,7 but also due to scarce representative data sources. Thus, this study aimed at estimating the prevalence of dengue and the costs related to dengue management using a large database comprised of 14 health insurance companies of the Brazilian Supplementary Health System, from 2015 to 2020.
MethodsThis is a descriptive, observational, retrospective study using information extracted from a secondary database of the private health system in Brazil. Records from patients registered in the database between January 2015 and December 2020 with follow-up information until March 2021 were included. The analysis period was defined according to the availability of the database.
Since the data used for these estimates are the number of claims from a secondary database that has deidentified data only, the privacy and confidentiality of the subjects were considered well protected.
DatabaseThe Orizon database used in this study contains billing transaction data between health providers and operators, including patients with active health plans. Medical billing data come from Orizon's electronic system, which contains data from 14 health plan operators in Brazil for authorizations and the payment of private service providers.10 Health care providers send the data to health plan operators through the electronic ‘invoice’ system. Customers have their data anonymized through an encrypted, unique identifier. To prevent coding and spelling errors, all information sent by providers is validated and standardized to the Standard for Exchange of Supplementary Health Information (TISS), which is recommended by the National Agency for Supplementary Health and the Ministry of Health. Data are made available in a secure cloud environment with backup and SQL language. Approximately 70% of operators are located in the Southeast region.
Study populationFrom 2015 to 2020, the Orizon database had an average of 9,577,482 patients. Considering approximate values for the period, the private health system accounts for 25% of the Brazilian population, and Orizon contains data from 20% of the private health system. Therefore, the population of the Orizon database represents approximately 5% of the Brazilian population from 2015 to 2020.
Dengue casesClaims from unique beneficiaries with ICD-10 A90 - Dengue (classical dengue) or A91 - Hemorrhagic fever due to dengue virus infection were eligible for inclusion. Claims that also had an ICD-10 of Zika, Chikungunya, Yellow Fever or COVID-19 or other well-established diagnoses (related to neoplasms, trauma, obstetric outcomes, chronic diseases and other infectious diseases) were excluded. For prevalence estimates, we used the date of diagnosis as the onset date. A dengue event was considered a reinfection if it occurred at least three months from the time of the previous infection. Each case was followed up for three months after the index date to assess associated health care resource utilization. Since January 2016, the ICD-10 code was no longer mandatory in the emergency room (ER) and clinic visits billing transactions; therefore, some dengue cases in these settings were not accounted for due to this database modification.
Dengue managementThe following procedures were assessed: exams, clinic visits, surgeries, and other procedures described while attending emergency care or during hospitalization. Medications included all medical supplies used by the patient during hospitalization or ER consultation, such as analgesics, antipyretics, antibiotics, saline solution, blood products, enteral diets, inotropic agents and special devices for drug administration.
CostsCosts included materials, medications, exams, consultation fees, daily fees, medicinal gases, orthotics, prostheses and special materials, surgeries, therapies and invasive procedures.
Statistical analysisPrevalence with 95% confidence intervals (CI) considered the number of claims cases by the number of beneficiaries that utilized the health care system and the total number of beneficiaries in the database in the year of interest. To describe the length of stay in the hospital and intensive care unit (ICU) and costs, measures of central tendency and dispersion, such as mean, median and interquartile range (IQR), were used.
Costs were adjusted for inflation using the “Citizen Calculator” of the Central Bank of Brazil, based on the IPCA-E index (IBGE). The values were adjusted for inflation as of December 2021, the latest available index and the month/year considered for the initial cost value was July (mid-year) of the year of the claim. Thus, the inflation indices used were 1.4196 for 2015 costs, 1.3026 for 2016, 1.2582 for 2017, 1.2136 for 2018, 1.1687 for 2019, and 1.1467 for 2020. For comparison purposes, the costs reported in other studies were converted to the Brazilian currency (Real) using the conversion reported in the article itself, considering July 2009 for Suaya et al. 2009,11 December 2010 for Vieira Machado et al. 2014,12 and November 2013 for Martinelli et al. 201513 and adjusted for inflation for December 2021. Then, all costs were converted to US dollars (US$) using an average exchange rate (R$ 1 = US$ 0.1792 on December 31, 2021).
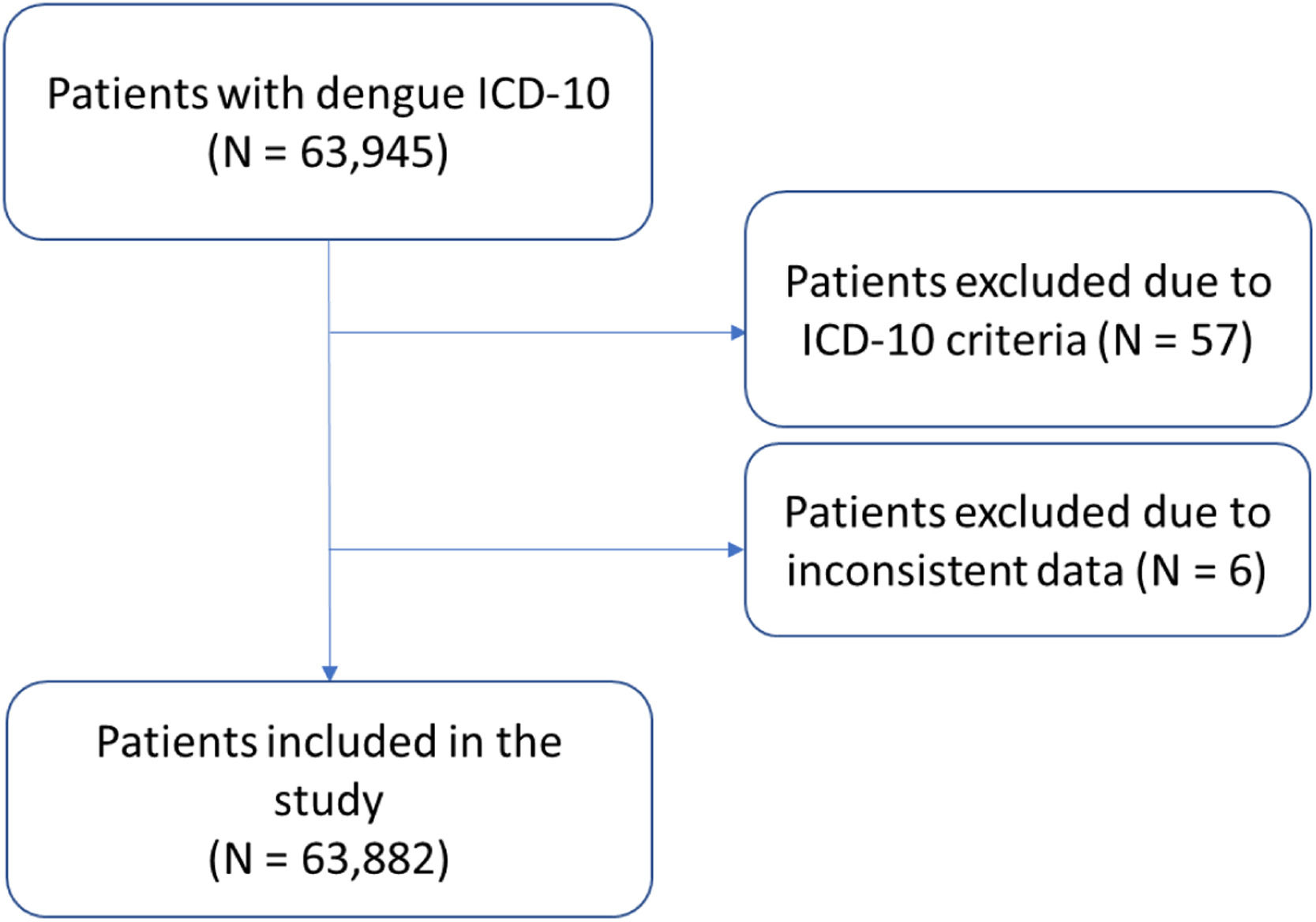
ResultsA total of 63,945 claims met the eligibility criteria. Of these, 57 had ICD-10 codes that met the exclusion criteria, and six had inconsistencies and were excluded (Fig. 1). The final set of dengue claims comprised 63,882 unique beneficiaries. Table 1 shows the prevalence of dengue claims by year among patients who utilized the system and by the total population of beneficiaries. The number of dengue claims ranged from 43,637 in 2015 to 1,868 in 2020.
Dengue claims cases by year and health care utilization.
The prevalence of dengue in this sample of private health care users was highest in 2015 (0.45%; 95% CI 0.45–0.46) and 2016 (0.13%; 95% CI 0.13–0.14), as was the prevalence of health care service utilization due to dengue (1.6%; [95% CI 1.59–1.62] for 2015 and 0.46% [95% CI 0.46-0.47] for 2016). The prevalence of dengue was 0.01% (95% CI 0.01–0.01), 0.01% (95% CI 0.01–0.01), and 0.04% (95% CI 0.04–0.05) for 2017, 2018, and 2019, respectively.
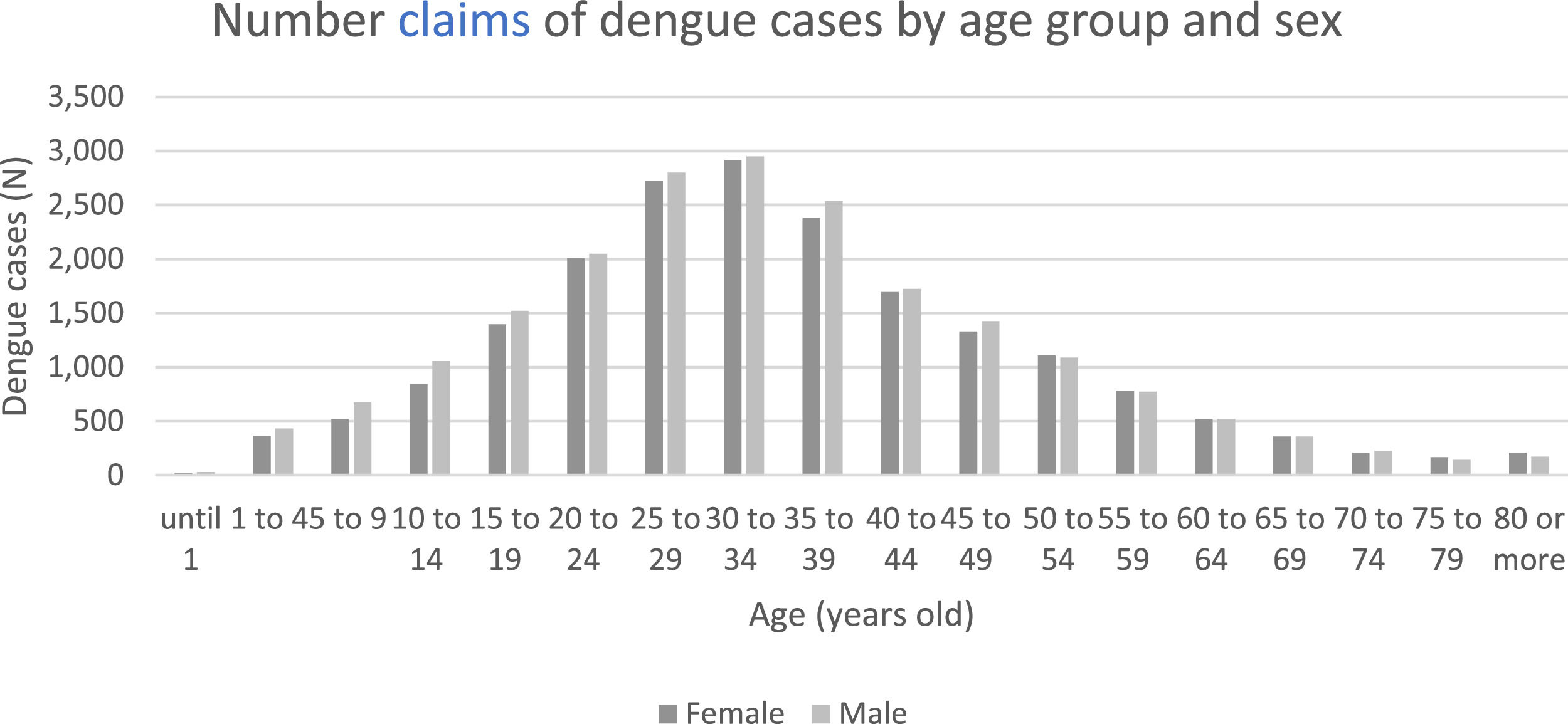
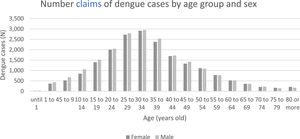
Regarding demographic characteristics, 30.6% were female, 32.1% were male and 37.3% had no information on sex. The median age of dengue cases was 33 years (IQR 24–46), and the majority of patients (51%) were in the age range of 20–39 years old (Fig. 2). The vast majority of beneficiaries (81.0%) were from the Southeast region, where the state of Sao Paulo accounted for 64.1%.
Regarding outcomes, 61,078 (95.6%) were discharged, 2,748 (4.3%) were transferred or had new admissions, and 46 (0.1%) died. Of the 46 deaths, 20 (0.05%) were in 2015, 11 (0.09%) in 2016, two in 2017 (0.2% of cases), one in 2018 (0.1% of cases), eight in 2019 (0.2% of cases), and four were in 2020 (0.2% of cases).
Regarding the length of hospital stay, the median duration was four days (IQR: 3.0-5.0). Approximately 40% stayed for 1-3 days, and 46.8% stayed for 4-6 days. Regarding the time in the ICU, 73.1% of the cases stayed from 1-3 days (median: 2 days; IIR: 2.0-4.0) (Table 2).
The total, hospitalization and emergency costs are shown in Table 3. The median cost per case in 2015 was US$114.03, increasing substantially over the years and reaching US$ 818.15 in 2020. The median cost of an emergency room visit ranged from US$ 97.78 in 2015 to US$118.16 in 2017. The median cost of hospitalization ranged from US$ 465.39 in 2016 to US$ 696.72 in 2020.
Total costs, costs per emergency care (EC), and hospitalization costs per dengue case.
Table 4 shows a comparison of the 2020 length of stay and costs of hospitalization with data from other studies. Compared to this study, the median length of stay in all other studies was shorter (3 vs. 4 days), and the average costs were lower (US$ 599.47, US$ 631.60 and US$ 588.14 vs. US$ 1,466.45).
Comparison of duration and adjusted costs per case of patients in the private health care system.
| Cases (N) | Median duration of hospitalization (days) | Hospitalization average cost (US$) | Hospitalization median cost (US$) | |
|---|---|---|---|---|
| Orizon database* | 1,861 | 4 | 1,466.45 | 696.72 |
| Martinelli et al., 2015⁎⁎ | 27 | NA | 599.47 | NA |
| Suaya et al., 2009 | 140 | 3 | 631.60 | NA |
| Vieira Machado et al., 2014 | 156 | 3 | 588.14 | 302.31 |
NA, not available.
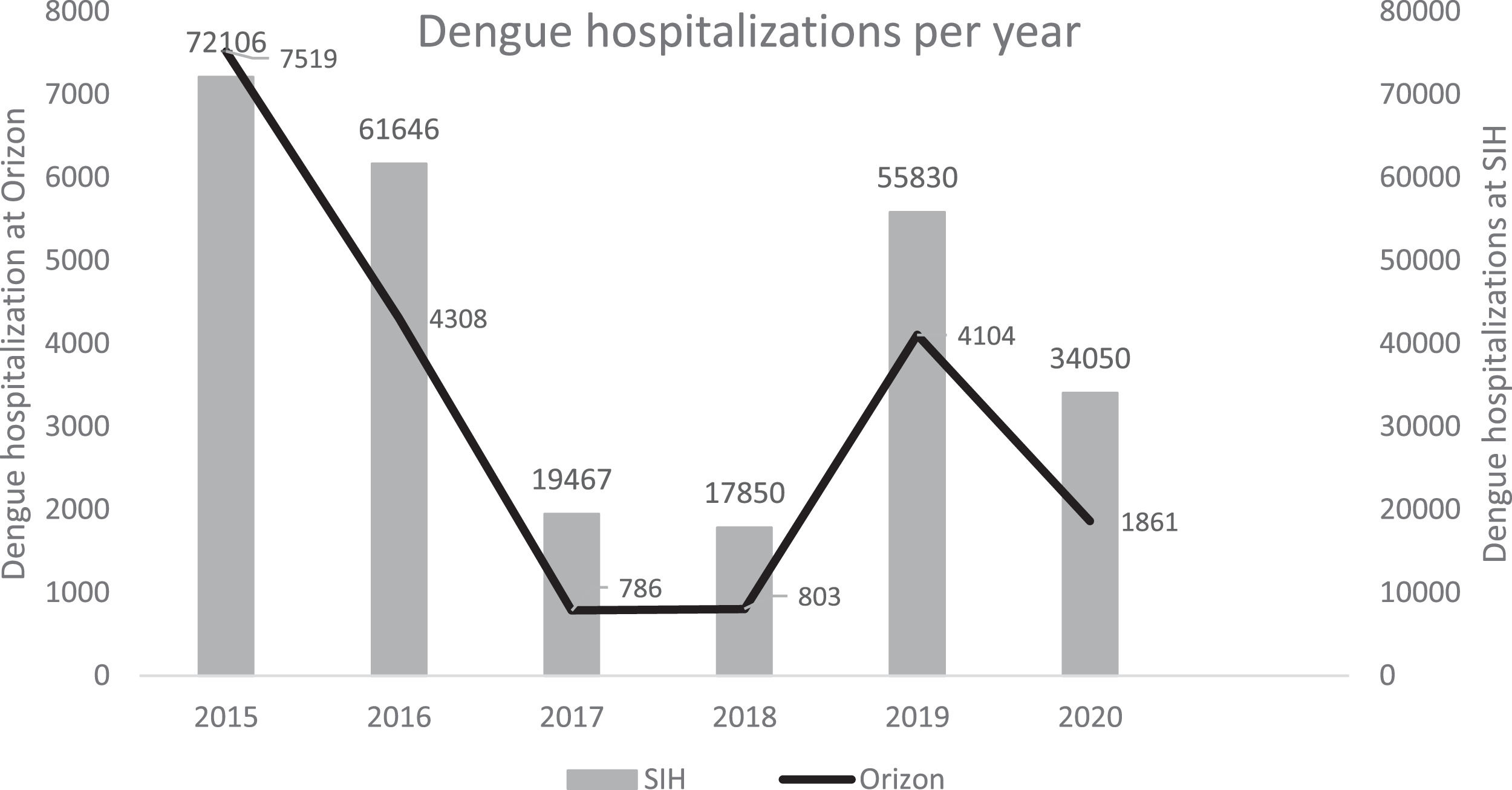
This study estimated the prevalence of dengue cases in the period between 2015 and 2020 and costs related to dengue management in a large supplementary health system database. The prevalence of dengue in this population was consistent with the epidemiological profile of dengue in Brazil during the study period. Although it is not possible to establish direct comparisons on the hospitalization rates between private and public health system users, we observed a greater absolute and relative number of cases in 2015, 2016 and 2019, years during which dengue was considered epidemic in Brazil (Fig. 3), suggesting that the population of private health service users, represented by wealthier and more educated families, was similarly affected by dengue. Several studies have suggested a relationship between socioeconomic status and dengue risk,14–16 but few have been able to establish a direct causal relationship or the strength of the association, as demonstrated in a comprehensive systematic review by Mulligan et al.17 Our data support the hypothesis that factors other than traditional indicators of poverty may play a role in the risk of becoming ill with dengue, such as geospatial and environmental determinants.18–21 We compared the demographic characteristics of our sample to those in the SIH database, considering only the Southeast region. Although we do not know whether hospitals in the Orizon database are affiliated with SIH, we observed a similar age distribution in both public and private hospitals, suggesting that our sample is representative of dengue cases that occurred in the Southeast region.
The analysis of costs by type of care (visits to the emergency room and hospitalization) was only possible for 2015, since the change in the coding affected the way ICD was recorded in later years. Nevertheless, we observed that hospitalization costs accounted for most of the total cost in all years. This finding is consistent with previous analyses that pointed out the use of hospital resources as the main component of direct costs in dengue management.22–28
In addition, a significant increase in the average cost of hospitalization was observed over the years, ranging from US$968.40 to US$1,466.45. This finding could indicate an increase in the occurrence of more severe cases, which required hospitalization, or a treatment bias, whereby expenses with increasingly complex and expensive complementary tests were incorporated in the management of hospitalized cases in private hospitals. These hypotheses require future studies designed for this purpose.
When compared with other studies that evaluated private hospitalization costs, our study found an adjusted mean cost two-fold higher and longer hospital stays. There are two possible explanations for this finding: the Orizon database may represent more expensive health plans compared with those evaluated by Suaya et al.11 Vieira Machado et al.12 and Martinelli et al.13 or the components that make up the total cost were different. Studies using standardized data collection would be necessary to ensure real comparability.
Our study has several limitations. The main limitation is related to the secondary nature of the data used, which conditions the quality of the data entry and recording. This limitation is clearly depicted in the proportion of missing information on demographic data. However, the sensitivity analysis in this subgroup did not show differences in length of stay or cost of hospitalization, suggesting that this bias was nondirectional. The use of active beneficiaries as a denominator is also a limitation, as it may vary over time and is dependent, to some extent, on employability, since the majority of health plans in Brazil are part of the benefit package for employees. However, we did not observe substantial fluctuations in the number of beneficiaries over time. In addition, since dengue is an acute condition, our prevalence estimate may be a reliable marker of incidence in this population. Finally, the use of confirmed dengue cases may have underestimated prevalence and cost data. We also did not include ICD-10 codes of other hemorrhagic fevers that could potentially be a misdiagnosed dengue case, which might have resulted in a loss of sensitivity.
In conclusion, this is the first database study to assess the impact of dengue on a population of private health care users. In this population, there was a significant increase in dengue cases in 2015, 2016 and 2019, consistent with the epidemiological scenario in the country. The decline in dengue-related claims observed in 2020 in this database followed an overall trend seen in several dengue-endemic countries and could be a result of restrictive measures imposed by the SARS-COV 2 pandemic.29 In addition, the nature of the data allowed us to generate a reliable estimate of the hospitalization cost for dengue, since they are not based on preestablished packages or composite costs, common payment practices in the SUS (the public Unified Health System). The data presented here contribute to the understanding of dengue disease burden and serve as a subsidy for health and economic studies aimed at estimating the impact of prevention and control measures.
FundingThis study was funded by Takeda Pharmaceuticals Brazil.
Author summaryDengue is a major public health problem in Brazil, the country with the highest number of dengue cases in the world. While the majority of Brazilians rely on the public health care system, which is free of cost, 25% of the population—mostly middle- and higher-income residents—have access to private health insurance. This study used a large database of claims from the private health care system and found that the prevalence of dengue in this population followed the same trend as dengue in the country, with the highest rates in 2015, 2016 and 2019. In addition, this is the largest study evaluating dengue costs in a real-world scenario in the private system in Brazil. The cost of dengue management was higher than estimated in previous studies and increased over the years. This study provides information that can be used to assist in better estimating the impact of dengue prevention and control measures.
CRediT authorship contribution statementDenise Alves Abud: Conceptualization, Methodology, Writing – review & editing. Claudia Yang Santos: Conceptualization, Methodology, Supervision, Project administration, Validation, Visualization, Writing – review & editing. Abner Augusto Lobao Neto: Conceptualization, Methodology, Funding acquisition, Supervision, Writing – review & editing. Juliana Tosta Senra: Conceptualization, Methodology, Supervision, Writing – review & editing. Suely Tuboi: Conceptualization, Methodology, Supervision, Validation, Visualization, Writing – review & editing.
We would like to thank the company Orizon Healthtech for providing the database for the study. We would also like to acknowledge Fernando Alencar from Origin for his statistical settings.