Neonatal infection is a serious public health problem. The aim of this study was to assess the influence of the antenatal care on the risk of early-onset neonatal healthcare associated infection in two Brazilian maternities.
MethodsCohort study – Newborns admitted at two public neonatal intensive care units from 2008 to 2009 were included in the study. Data on antenatal and perinatal variables were collected from maternal prenatal cards and medical charts. Newborns were actively surveyed for early-onset neonatal healthcare associated infection, defined as a neonatal infection diagnosed within 48h after birth. Multiple logistic regression was used to assess variables independently associated with early-onset neonatal healthcare associated infection.
Results561 neonate–mother pairs were included in the study. Early-onset neonatal healthcare associated infection was diagnosed in 283 neonates (51%), an incidence rate of 43.5/1000 live births. Neonates whose mothers had less then six antenatal visits were under risk significantly higher for early-onset neonatal healthcare associated infection (OR=1.69, 95% CI=1.11–2.57), after adjusting for birth weight, membranes ruptured for >18h, maternal complications during delivery, maternal infection at admission, and hospital where patients received care.
ConclusionsThe risk of neonatal early-onset neonatal healthcare associated infection was significantly associated with insufficient number of antenatal care visits. Further studies assessing the quality of antenatal care and targeting its improvement are warranted.
Neonatal infection is a major cause of morbidity and the second leading cause of neonatal death worldwide. It has been estimated that, in developing countries, neonatal infection causes 1.6 million deaths per year.1
Brazil follows global trends as the neonatal mortality rate (NMR) is the main component of the infant mortality rate (IMR). In fact, there was a decrease in Brazilian NMR from 27/1000 live births in 1990 to 10/1000 live births in 2011, but it still remains elevated as compared to the rates reported from other countries such as Japan (1/1000 live births), Canada (4/1000 live births), USA (4/1000 live births), and Chile (5/1000 live births). Additionally, little change has been observed in the early neonatal component of IMR, a period covering the first seven days of life.2
A considerable proportion of the deaths that occur during the first week of life in Brazil are associated with neonatal infections of maternal origin (MO), which are closely related to the health care provided to pregnant women during antenatal care.3,4 The vast majority of these infections present within 48h after birth and are called early-onset healthcare associated infections (EOHCAI). They occur mainly due to vertical transmission of microorganisms present in the maternal genital tract and are acquired mostly in the perinatal period and during delivery.5 They are associated with maternal risk factors such as: premature rupture of membranes (PROM) above 18h before delivery; chorioamnionitis; untreated maternal urinary tract infection (UTI); Streptococcus agalactiae vaginal colonization without intrapartum chemoprophylaxis; maternal fever 48h before delivery; maternal and fetal invasive procedures 72h before delivery.6–8
In Brazil, the EOHCAI, low birth weight, and prematurity have attributed to inappropriate assistance to pregnant women.9 The antenatal care is an opportunity to raise awareness and educate women about the care of their own health and of their concepts, related to changes in lifestyle habits (exercise and nutritional status) and behavioral risk factors (cessation of smoking, alcohol, drug using, and guidance on preventing sexually transmitted infections).10 This period allows for the diagnosis and treatment of various complications during pregnancy and consequently, the reduction or elimination of risk factors for EOHCAI.9
The main objective of this study was to assess whether adherence to antenatal care would decrease the risk of EOHCAI in two public Municipal hospitals (MHS) in the municipality of Rio de Janeiro, Brazil.
MethodsThe present study, undertaken through a partnership between the Universidade Federal do Rio de Janeiro (UFRJ) and Rio de Janeiro Municipality Health Department (RJMHS), was a prospective cohort study carried out in the Neonatal Intensive Care Unit (NICU) and Neonatal Intermediary Care Unit (NiCU) of two public hospitals of RJMHS, totaling 34 NICU beds and 28 NiCU beds in the period of July 2008 to February, 2009.
Both hospitals had a level II NICU, a conventional NiCU, and a kangaroo neonatal intermediate care unit. The intensive and intermediate care provided to newborns was carried out in separate environments by a team of health care workers that included neonatologists, pediatric residents, nurses, nurse-assistants, physiotherapists, and speech therapists. The overall average occupancy rate was (123%). High-complexity surgical procedures were not performed in any of the study centers.
In both centers, maternity care was provided by obstetricians and residents in obstetrics, anesthesiologists, nurses, and nurse-assistants. Unit 1 was a reference center for high risk pregnancies.
Both maternity hospitals had an infection control team. They performed active infection surveillance according to National Healthcare Safety Network.11 They also provided counseling on antimicrobial use, monitored multidrug-resistant microorganisms, and implemented basic measures for prevention and control of healthcare associated infections (HCAI). All newborns admitted to NICU/NiCU and their mothers were eligible for the study. Each neonate–mother pair was included in the study only after the mother signed a written informed consent. Patients were excluded if the delivery had not taken place in one of the two study centers. Twins and newborns who had less than 24h of follow-up were also excluded.
After inclusion in the study, data on the antenatal care was gathered using a standardized questionnaire to be filled in by the mother. Additional data on the prenatal care were abstracted from the antenatal care card. This is a document that all pregnant women who attend antenatal care in Brazil must have, in which dates of medical visits and clinical, laboratory, and medication data are recorded. It is recommended that pregnant women take this card to the maternity hospital at the time of delivery. The medical charts of mothers and neonates were also used to collect data on perinatal variables and on neonate infections. The following variables were assessed: maternal age at delivery; gestational age at birth (Ballard method); number of antenatal care visits; number of previous pregnancies, births and abortions, previous prematurity, previous stillbirth, previous neonatal death; gestational complication (hypertension, diabetes, sexually transmitted infections); risk behavior (smoking, alcohol use, illicit drug use during pregnancy); antenatal tests: VDRL, urine culture, serology for HIV and toxoplasmosis, culture for S. agalactiae; and treatment procedures; type of delivery, duration of ruptured membranes and labor; antepartum maternal fever; birth complications; antibiotic use in the antenatal care, labor/delivery/neonatal periods; maternal infections, and neonatal infections diagnosed in the first 48h of life. These data were collected by BRM and AF under the supervision of the study coordination. Both professionals were trained in the methodology of the project and worked in line with the infection control team of both centers.
The primary outcome of the study was the occurrence of EOHCAI defined as infections diagnosed in the first 48h of life. Infection was defined by the presence of at least one of the following clinical manifestations that could not be explained by other known cause: fever (>38°C), hypothermia (<36°C), apnea, bradicardia, taquicardia, respiratory distress, slow peripheral perfusion, hemodynamic instability and letargy, associated with the decision of the assistant physician to start antimicrobial therapy. The secondary outcomes of the study were laboratory-confirmed EOHCAI (infections defined according to National Healthcare Safety Network, and with an etiological agent isolated from an sterile site); delivery complications (prematurity, intense bleeding and/or placenta abruption); death associated with or caused by EOHCAI (as defined by the infection control team of each center); and maternal infection (sexually transmitted infections, abnormal vaginal discharge, urinary tract infection, chorioamnionitis, pneumonia, surgical wound infection).
Statistical analysisData were stored in a database developed with a Microsoft Access 2007® software platform. Subsequently, the distribution of all variables was studied. Univariate analysis of the association of EOHCAI and the studied variables was performed using Student's t test or Mann–Whitney test for continuous variables and chi-square or Fisher's exact test for categorical variables. Multivariate analyses using backwards stepwise logistic regression were performed. In these models, the dependent variable was EOHCAI. The independent variables selected for the multivariate analyses were those associated with a p-value <0.15 in the univariate analysis. Variables with a p-value ≤0.05 were kept in the final adjusted model if associated with a p-value ≤0.05, calculated by the log likelihood ratio test. Statistical analysis was performed using the statistical package STATA version 9.0, Texas, USA.
This project was submitted and approved by the Ethics Committees of the University Hospital Clementino Fraga Filho (HUCFF-UFRJ) (Protocol No. 235/04) and of the Municipality of Rio de Janeiro Ethical Committee (Protocol No. 75/08).
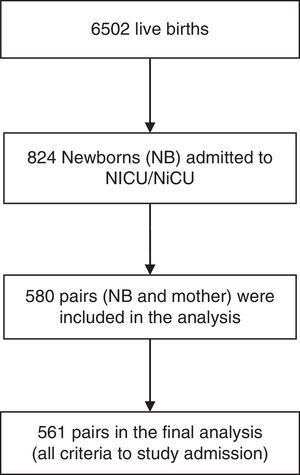
ResultsThere were a total of 6443 deliveries in the two participating maternity hospitals (2460 and 3983 in each), during July 2008-February 2009, with 6502 live births (2557 and 3945 in unit 1 and 2, respectively) including twin births. Of the 824 newborns admitted to NICU/NiCU during the study period, 580 (70.4%) were included in the study. After merging neonate and maternal databases, it was possible to evaluate data for 561 neonate–mother pairs; 18 pairs were excluded because the hospitalization and the discharge date of the newborns were the same, and one due to loss of maternal records (Fig. 1). The incidence of EOHCAI was 50.5% (283/561). Considering that 6443 deliveries took place in the two units during the study, and probably all EOHCAI were admitted to NICU/NiCU, the incidence density of EOHCAI was 43.5 per 1000 live births. The incidence of laboratory confirmed EOHCAI was 2.1%; the isolated organisms were Staphylococcus aureus (two), Staphylococcus haemolyticus, S. agalactiae, viridans group Streptococci, and Streptococcus sp. (one each).
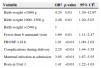
Table 1 shows, in the univariate analysis, a statistically significant association of EOHCAI with the following variables: gestational age, birth weight, complications in labor, period of ruptured membranes, number of prenatal visits, use of antibiotic during childbirth, presence of maternal infection during hospitalization.
Risk factors for early-onset neonatal healthcare associated infection (EOHCAI) – univariate analysis.
| Variable | EOHCAIN=283 (50.4%) | Without EOHCAIN=278 (49.6%) | Relative risk | p-value |
|---|---|---|---|---|
| Male gender | 148 (52) | 152 (55) | 0.95 | 0.57 |
| Gestational age at birth – weeks | 34.00 (3.79) | 36.56 (3.42) | <0.01 | |
| Mean (SDa) | ||||
| Birth weight (g) | ||||
| >1500 | 202 (71) | 255 (91) | ||
| 1000–1500 | 52 (18) | 16 (5) | ||
| <1000 | 29 (10) | 7 (2) | <0.01 | |
| PROM >18h | 95 (33) | 168 (60) | 1.94 | <0.01 |
| APGAR <5 on 5th min | 19 (6) | 19 (6) | 0.98 | 0.97 |
| Vaginal delivery | 119 (42) | 115 (41) | 1.02 | 0.94 |
| Neonatal Surgery | 6 (2) | 6 (2) | 1.0 | 0.97 |
| Antenatal care | 259 (91) | 262 (94) | 0.96 | 0.21 |
| Fewer than antenatal visits | 182 (64) | 113 (40) | 1.62 | <0.01 |
| Number of pregnancies (including the studied) | 1.11 (1.38) | 1.06 (1.40) | 0.66 | |
| Mean (SDa) | ||||
| Parity (including the studied) | 1.11 (1.38) | 1.06 (1.40) | 0.66 | |
| Mean (SDa) | ||||
| Previous prematurity | 40 (14) | 29 (10) | 1.4 | 0.24 |
| Previous natimortality | 13 (5) | 15 (7) | 0.86 | 0.70 |
| Hypertension on pregnancy | 65 (23) | 71 (25) | 0.88 | 0.48 |
| Sexually transmitted infections in pregnancy | 7 (2) | 9 (3) | 0.76 | 0.58 |
| Infections in pregnancy | 93 (33) | 85(31) | 1.07 | 0.50 |
| Tobacco exposure in pregnancy | 45(16) | 41(15) | 1.08 | 0.69 |
| Alcohol exposure in pregnancy | 25(9) | 25(9) | 0.98 | 0.55 |
| Antibiotic use on antenatal care | 77 (27) | 81(29) | 0.93 | 0.68 |
| Complication during delivery | 221 (78) | 135 (49) | 1.59 | <0.01 |
| Antibiotic use in labor/delivery | 183(64) | 149(53) | 1.22 | <0.01 |
| Invasive procedures in the mother at the admission | 8(3) | 1(0.3) | 8.0 | <0.01 |
| Maternal infection at the admission | 78 (27) | 27 (10) | 2.7 | <0.01 |
| Maternal age in years | 26.36 (7.14) | 25.95 (6.60) | 0.47 | |
| Mean (SDa) | ||||
| Born in Unit 1 | 138 (48) | 65 (23) | 2.0 | <0.01 |
In Table 1, nine maternal invasive procedures were described at hospital admission. All of them were indwelling urinary catheter placement
Table 2 shows the results of multivariate analysis. Variables with a statistically significant association with EOHCAI were: PROM >18h, less than six antenatal care visits, maternal infection at admission, birth weight <1000g and 1000–1500g, and to be born in Unit 1.
Risk factors for early-onset neonatal healthcare associated infection (EOHCAI) – multivariate analysis.
| Variable | ORa | p-value | 95% CIb |
|---|---|---|---|
| Birth weight <1000g | 4.24 | 0.01 | 1.39–12.97 |
| Birth weight 1000–1500g | 2.46 | 0.01 | 1.20–5.03 |
| Birth weight >1500g | 1 | ||
| Fewer than 6 antenatal visits | 1.69 | 0.01 | 1.11–2.57 |
| PROMc >18h | 1.01 | <0.01 | 1.00–1.02 |
| Complications during delivery | 2.25 | <0.01 | 1.44–3.55 |
| Maternal infection at admission | 3.05 | <0.01 | 1.67–5.55 |
| Born in Unit 1 | 1.41 | <0.01 | 1.22–1.63 |
There was an important association between maternal infection at admission and EOHCAI. Chorioamnionitis (8.1%) and UTI (5.9%) were the most frequent maternal infections. There were 30 deaths: 6.0% among newborns with EOHCAI and 4.7% in the group without infection (p=0.15). Therefore, a relationship between death and EOHCAI was not observed.
DiscussionIn Brazil, the Ministry of Health guidelines recommend that pregnant women have at least six antenatal visits. Antenatal care is indeed one important means of decreasing neonatal morbidity, since proper antenatal care can decrease the risk of maternal infection, hypertension, drug use and other factors leading to prematurity, neonatal complications, and EOHCAI.1,3,6,9
In this prospective study, carried out in two public hospitals in the city of Rio de Janeiro, a significant increase in the risk of EOHCAI was observed among neonates born to women who did not follow this recommendation. This association remained significant in a multivariate model adjusted for other established risk factors such as PROM for more than 18h, maternal infection at labor, and low-birth weight.
The proportion of pregnant women who adhered to at least six antenatal visits in this study (38%) was much lower than the average rate of 61%, observed in Brazil in 2010. The causes of such low number of antenatal visits were not addressed in the present study, but are likely related to factors such as poor access to primary care clinics, or lack of health education to understand the importance of antenatal care to prevent maternal and neonatal complications.
Further studies are warranted to clarify this issue and to evaluate strategies to improve adherence to antenatal care in middle-income countries such as Brazil, and to analyze the impact of these strategies on EOHCAI incidence.
In line with the results of previous studies, we observed that PROM for more than 18h, maternal infection at labor, and low-birth weight were associated with EOHCAI.12–17 Reports from the last two decades have associated maternal infections with undesirable outcomes such as premature birth, stillbirth, and fetal and neonatal infection.18–20 Moreover, infection and fetal inflammation syndrome have been implicated in the genesis of short- and long-term morbidities, such as intrauterine growth retardation, intraventricular hemorrhage, respiratory distress syndrome, necrotizing enterocolitis, cerebral palsy, and chronic lung disease.21,22
The most prevalent maternal infections in our study were chorioamnionitis and UTI, which were also important risk factors for neonatal infection. In Canada, a multicenter study conducted in two periods, 2003–2005 and 2006–2008, where 405 (6.5/1000 admissions) newborns were diagnosed with EOHCAI, maternal chorioamnionitis occurred in 26–36% of neonates with early sepsis, in the respective periods.23 Other studies have also found an association between maternal chorioamnionitis or UTI and neonatal sepsis.24–28
Prolonged PROM is significantly associated with the risk of maternal, fetal, and neonatal infections, as described in a nested case-control study conducted in the US in newborns with a gestational age greater than or equal to 34 weeks, in 14 hospitals in the period 1993–2007. The chance of early neonatal infection increased in parallel with the duration of ruptured membranes.29
This study has some limitations that must be acknowledged. The results demonstrated a very high incidence of EOHCAI, 43.5/1000 live births. Most of these infections were based on clinical, not laboratory confirmed, and were likely overestimated. However, the same definitions were used during the whole study period, and these definitions were used not only for surveillance, but also for treatment purposes. Consequently, although overestimated, this EOHCAI incidence rate reflected the reality of neonatal care in two public hospitals in Rio de Janeiro. Have we considered only the laboratory confirmed infections, EOHCAI incidence would have been highly underestimated, probably reflecting issues related to lack of blood specimen collection and intensive maternal antibiotic use during labor and delivery.
Since neonatologists use the maternal history to assess the chance of neonatal infections, the associations between EOHCAI and PROM or maternal infections could be an assessment bias. Therefore, even if biased, this association must be studied and described, since neonates were diagnosed and treated as if they were infected, and the biological plausibility of these associations was clear. It would be impossible not to consider and adjust for these variables. However, since neonatologists were unaware to the number of ANC visits, this association should not be considered biased.
Another limitation of the study was the lack of assessment of the quality of ANC and its possible relationship with the risk of EOHCAI. Studies conducted in Brazilian municipalities of São Luis, Recife, and Rio de Janeiro evaluating the performance of ANC programs described poor quality of care, even of patients with more than six visits.10,30,31
In conclusion, this was a multicenter study carried out in public hospitals, considering the mother and newborn pair, placed in the context of clinical practice in a metropolitan area of a large city in Latin America demonstrating a very high incidence of EOHCAI. Even adjusting for known perinatal risk factors, poorer ANC (less than six visits) was associated with EOHCAI. Studies to evaluate and improve the quality of ANC must be encouraged.
Conflicts of interestThe authors declare no conflicts of interest.
We received funding support for the study from the Fundação de Amparo a Pesquisa do Rio de Janeiro, grant number: E-26/110.473/2007, for Cunha AJ, and Conselho de Aperfeiçoamento do Ensino Superior (CAPES).