In this study, Entamoeba histolytica had high prevalence and unusual presentation by affecting high proportion of infants under 1 year; severe clinical manifestations, and laboratory findings that were known to be usually encountered in invasive amebiasis as significant leukocytosis for age, neutrophilic leukocytosis for age, and positive C-reactive protein were found among more than 50% of admitted Saudi infants and children with E. histolytica infection in our locality. E. histolytica can be a re-emerging serious infection when it finds favorable environmental conditions and host factors which are mainly attributed to inadequate breastfeeding in this study. This may occur in any other area of the world with the same risk factors, so we must be ready to tackle it with effective and more powerful preventive measures.
Amebiasis, caused by the intestinal parasite Entamoeba histolytica, has an estimated worldwide prevalence of 500 million cases of symptomatic disease, and 40.000–110.000 deaths annually. Amebiasis is the 3rd leading parasitic cause of death worldwide.1,2 It is an important health problem, especially in developing countries.3 The rate of infection by E. histolytica differs among countries, socio-economic and sanitary conditions, and populations.4 It is highly endemic throughout poor and socio-economically deprived communities in the tropics and subtropics. Environmental, socio-economic, demographic, and hygiene-related behavior is known to influence the transmission and distribution of intestinal parasitic infections.5 A study in Brazil identified place of residence, age, ingestion of raw vegetables, and drinking water quality as important risk factors.6
Because transmission is frequently associated with contaminated food and water, young infants are not expected to develop amebiasis very often. More severe disease is associated with young age, malnutrition and immunosuppression.7
Intestinal parasitic infection is still a common and significant public health problem among children in Saudi Arabia. In our study area, Jeddah, the prevalence of E. histolytica during the period December 1995–October 1996 was found to be 2.2% of 576 fecal samples collected from children (0–5 year(s) old) suffering from acute diarrhea and attending hospitals and outpatient clinics in Jeddah.8
Between the months of March and November 2005, in Makkah 70km from Jeddah, a high prevalence of intestinal parasitic infections (70.5%) was detected among the studied patients. E. histolytica/Entamoeba dispar and Giardia lamblia were found to be the most common intestinal parasites among patients.9
Another cross-sectional study was undertaken between March and August 2007 in Jeddah at two major public hospitals, and E. histolytica/E. dispar was detected at a prevalence of 8.3% inpatient and 5.9% outpatient.10
After the observation of a considerable number of infants and children admitted to our 2 main hospitals at south Jeddah, Ibn Sina College Hospital and Al-Jedaani Hospital with gastroenteritis caused by E. histolytica, we decided to conduct this study to assess the prevalence, characteristic nature, and risk factors for the problem of severe amebiasis necessitating hospitalization in infants and children of our locality, and in comparison with other hospitalized cases with non-E. histolytica gastroenteritis (GE).
Materials and methodsPatient selectionThis study was carried out at 2 main tertiary care hospitals at south Jeddah, Ibn Sina College Hospital and Al-Jedaani Hospital during the period from July 2010 to July 2011. Infants and children between the ages of 1 month and 16 years and admitted with GE that necessitated hospitalization were recruited in the study. This study was approved by the research and ethical committee of Ibn Sina College Hospital. For better comparative analysis and characterization of our E. histolytica cases, a cross-sectional comparative study was conducted as all GE cases were divided into 3 main groups: group I (confirmed E. histolytica cases), group II (confirmed Rotavirus (RV) cases), and group III (GE due to other enteropathogens or non-E. histolytica, non-RV cases).
Exclusion criteriaPatients less than 1 month, and more than 16 years, wasted and/or stunted malnourished patients, and patients with immunodeficiency, immunosuppression, or having any extra-intestinal infection at the time of hospitalization. Cases with diarrheal illness who had received antibiotics in the preceding 2 months that might be related to Clostridium difficile-associated diarrhea or antibiotic-associated pseudomembranous colitis were also excluded from this study.
MethodologyThe following data were recorded on admission for all patients, age, gender, nationality, residence, socioeconomic level, degree of education, occupation, household sanitary and hygiene conditions, household use of tap water, personal hygiene habits such as washing hands before eating, and water source for drinking. Complete data about type of feeding (breast fed or formula feeding) were taken. Inappropriate or inadequate breastfeeding practice was defined as complete absence or lack of exclusive breastfeeding for any duration from birth till the age of 6 months.
All infants and children admitted for GE were subjected to thorough history taking, anthropometric measurements, general and systemic examinations, and laboratory investigations (CBC including total and differential leukocyte count, C-reactive protein (CRP), stool examination, and stool E. histolytica-specific antigen detection). Leukocytosis and neutrophilia were defined according to age-related specific values for each individual case.11 Imaging investigations (abdominal and pelvic ultrasound, abdominal X-ray, and CT) were performed when needed on case-by-case basis.
Our protocol of treatment included a combination of metronidazole infusion and intravenous 3rd generation cephalosporine (ceftriaxone). Ceftriaxone was used for E. histolytica cases with clinical (high fever and toxic state) and/or laboratory (leukocytosis and positive CRP) evidence of invasive amebiasis or possible unrevealed coinciding bacterial infections that are associated with E. histolytica infection.12 The high likelihood of having a severe bacterial infection was expected in the presence of polymorphonuclear leukocytes greater than 10.000/mm3 or nonsegmented polymorphonuclear leukocytes greater than 500/mm3.13 Blood cultures were also done for these cases to detect possible associated bacteremia.
The patient course of illness, follow-up, and response to treatment was recorded for each admitted case with GE.
Sampling and laboratory techniquesFresh stool samples were collected in sterile containers and sent immediately to the hospital laboratory.
Examination of feces for protozoa and helminthsFecal samples were examined for adult worms, segments of tapeworms, ova, cysts, larvae, trophozoites, and cellular exudates such as WBCs, RBCs, and macrophages.
Stool specimens were transported very rapidly to the laboratory and examined within 30min of collection of the specimen to avoid disintegration of trophozoites. Fecal preparations (formol-ether concentrations) were used to examine for the presence of ova, cysts, and larvae.
Microscopic examination of fecal material or from the concentrated specimens was done by saline wet mount to detect worm eggs or larvae, protozoan trophozoites, and cysts and to reveal the presence of RBCs and WBCs. Iodine wet mount was used to stain glycogen and nuclei of the cysts. Modified Ziehl–Neelsen and acid-fast stains were used to examine for Cryptosporidium and Cyclospora.
Entamoeba histolytica antigen detectionThe stool samples with E. histolytica trophozoites were tested to confirm the presence of E. histolytica using the E. histolytica II antigen detection Kit (TechLab, Blacksburg, VA) following the instructions provided by the manufacturer.14 This was done to exclude the association with the non- pathogenic form of Entamoeba (E. dispar).
Examination of feces for virusesRotavirus was detected after collecting sufficient quantity of feces (1–2mL or 1–2g) in a clean dry container and the fecal specimen was analyzed by Acon One Step Rota Virus Test Device (Acon Laboratories, Inc. 4108 Sorrento Valley Boulevard, San Diego, CA 92121, USA). It is a one-step lateral-flow immunoassay (qualitative test) for detection of rotavirus in human feces with a relative sensitivity of >99.9%, relative specificity of 97.8%, and relative accuracy of 99.0%.
Adenovirus was detected by VIro-Capture kit (Bioincell), according to the manufacturer's protocol.15
Examination of feces for bacterial enteropathogensStool cultures for enteric bacteria were mainly limited to Salmonella, Shigella, Campylobacter spp., and Shiga toxin-producing Escherichia coli as E. coli serotype 0157:H7 based on the ability of such enteropathogens to cause dysentery-like illness such as E. histolytica, the previous epidemiologic prevalence of these enteropathogens in stool cultures of our locality, and the availability of their diagnostic tests.
Shigella and Salmonella were identified by standard bacteriologic methods with primary isolation on MacConkey, XLD (xylose lysine deoxycholate) agar, and Salmonella–Shigella agar to inhibit the growth of normal flora and growth amplification of Salmonella in tetrathionate broth.16,17 No further biochemical or serological identification was done for the detected Salmonella and Shigella species.
Campylobacter species were cultured by first plating the stools onto modified Skirrow's agar and incubating the plates at an elevated temperature (42°C) and under microaerophilic conditions (5–10% oxygen) for up to 72h before a negative report is issued. Only culture plates with colonies showing the characteristic Campylobacter growth morphology, Gram-stain characteristics and oxidase positivity were then reported as Campylobacter spp.18 Further identification to the species level was not attempted.
The diagnosis of diarrheagenic E. coli infection was made by initial isolation of the bacteria from stool cultures, and based on biochemical criteria (e.g., fermentation patterns). Enterohemorrhagic E. coli (EHEC or O157:H7) was suggested by the failure to ferment sorbitol on MacConkey sorbitol medium.19
The sample size and power of the studyThe level of confidence in this study was set at 95% with alpha error=0.05. With a previously detected prevalence of E. histolytica in inpatient cases at our locality of 8.3%,10 the maximum expected prevalence was 15%. The power of this study was settled at 90 with beta error of 0.10. The estimated sample size was 438. The research team decided to increase the sample size by about one third to increase the power of the study and guard against incomplete data by using Medcalc program available at www.Medcalc.be.
Statistical analysisThe data were analyzed by using statistical package for social science program version 16. Mann–Whitney U-test was used for comparison between two groups as the data were non-parametric using Kolmogorov–Smirnov test. The qualitative data were presented in the form of number and percentage. Chi-square test was used for comparison of qualitative data. The risk was estimated by using odds ratio and 95% confidence interval. Significance was considered at p value less than 0.05.
ResultsOne thousand three hundred and twenty-five pediatric cases were admitted at Ibn Sina college Hospital and Al-Jedaani Hospital in one year from July 2010 to July 2011. Gastroenteritis was the most common cause for pediatric hospitalization as more than 50% of total pediatric case admission during this period was due to GE (738/1325=55.7%).
One hundred and thirty-eight cases were excluded due to failure to fulfill the inclusion criteria (49) and mixed infections (89). The most common combined infection associated with E. histolytica was Shigella infection (in 11 cases) and they were also among the excluded cases in the present study.
Six hundred cases with GE were included in this study and were subsequently divided into 3 main groups: group I (E. histolytica group=120 cases), group II (RV group=113 cases), and group III (non-E. histolytica, non-RV group=367 cases). Group III comprised cases of GE due to viruses other than RV such as adenovirus (29 cases, 8%) and bacteria such as Salmonella (56 cases, 15.3%), Shigella (49 cases, 13.4%), E. coli (33 cases, 9%, only one isolate was considered as EHEC), and Campylobacter (8 cases, 2.2%). Also, few cases of GE in group III were associated with G. lamblia (5 cases, 1.4%) and helminthic infection (6 cases, 1.6%), mainly Ascaris lumbricoides (3), Trichinella spiralis (1) and Strongyloides stercoralis (2). One hundred and eighty-seven cases (187/367; 49.32%) in group III did not have specific diagnosis for their diarrheal illness which might be due to other unidentified enteropathogens such as astrovirus, enteroviruses, Aeromonas, Plesiomonas, Yersinia, or due to non-infectious etiology for diarrhea.
E. histolytica was the most common prevalent enteropathogen associated with GE in the present study (120 case; 20%) which was even more common than RV cases as well as cases of enteric bacteria caused by either Salmonella or Shigella.
The median age was significantly higher in the E. histolytica group than in RV group and non-E. histolytica, non-RV group (p1<0.001 and p3=0.021 respectively). Significantly lower median age was found in RV group compared to E. histolytica group and non-E. histolytica, non-RV group (p1<0.001, and p3=0.012, respectively). The percentage of cases under one year of age was significantly higher in RV group than in E. histolytica group and non-E. histolytica, non-RV group (p1=0.021, and p3<0.001, respectively). No significant difference was found between the 3 studied groups as regards gender and residence at south Jeddah (p>0.05). Saudi nationality was significantly more common among E. histolytica cases than the other 2 groups (p1=0.021, and p2=0.016, respectively). The demographic factors that demonstrated small risk for E. histolytica infection included age under one year in E. histolytica group compared to group III (OR 2: 1.48), and male gender (OR 1: 1.32, OR 2: 1.1), and residence at south Jeddah (OR 1: 1.18, OR 2: 1.46) when E. histolytica group was compared to group II and group III. Saudi nationality was found to be associated with more risk to acquire E. histolytica (OR 1: 3.25 OR 2: 3.05) Table 1 shows the demographic characteristics of the studied groups.
Comparison of the demographic characteristics between the studied groups.
| Character | E. histolyticaGroup I (n=120) | RVGroup II (n=113) | Non-E. histolytica, non-RVGroup III (n=367) | Odds ratio(95% CI) | p values | |||
|---|---|---|---|---|---|---|---|---|
| Age | ||||||||
| Median | 35 months | 11 months | 26 months | p1<0.001*** | ||||
| Range | 1–192 | 2–58 | 3–126 | p2=0.021* | ||||
| IQ range | 11–68 | 8–30 | 18–84 | p3=0.012* | ||||
| Age under one year | ||||||||
| (Number, %) | 44 | 36.7 | 58 | 51.3 | 103 | 28 | OR 1=0.55 (0.31–0.96) | p1=0.021* |
| OR 2=1.48 (0.93–2.34) | p2=0.74 | |||||||
| p3<0.001*** | ||||||||
| Male gender | ||||||||
| (Number, %) | 74 | 61.7 | 62 | 54.9 | 218 | 59.4 | OR 1=1.32 (0.76–2.31) | p1=0.29 |
| OR 2=1.1 (0.71–1.72) | p2=0.66 | |||||||
| p3=0.39 | ||||||||
| Saudi nationality | ||||||||
| (Number, %) | 115 | 95.8 | 99 | 87.6 | 324 | 88.3 | OR 1=3.25 (1.05–10.76) | p1=0.021* |
| OR 2 =3.05 (1.12–8.99) | p2=0.016* | |||||||
| p3=0.94 | ||||||||
| Residence at south Jeddah | ||||||||
| (Number, %) | 109 | 90.8 | 101 | 89.2 | 320 | 87.2 | OR 1=1.18 (1.09–1.7) | p1=0.71 |
| OR 2=1.46 (0.7–3.09) | p2=0.28 | |||||||
| p3=0.53 | ||||||||
p1 group I versus group II; p2 group I versus group III; p3 group II versus group III; OR 1=group I versus group II; OR 2=group I versus group III.
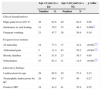
Cases with GE due to E. histolytica were admitted because of any or combination of the following symptoms; high-grade fever, frequent vomiting and intolerance to oral food or drink, severe abdominal pain, dehydration, and electrolyte disturbances. The group of infants under 1 year of age presented with significantly higher intolerance to oral feeding, more frequent loose motions, and dehydration than the 1–16 years age group (p=0.009, p<0.001, and p<0.001, respectively). The 1–16 years group had significantly higher presentation with abdominal pain than the group of infants less than 1 year (p<0.001). No significant difference was detected between both age groups regarding symptoms such as high-grade fever, frequent vomiting, bloody diarrhea as well as laboratory findings (p>0.05). Table 2 shows the percentages of these variable clinical manifestations and laboratory findings in 2 main age groups: <1 year and from 1 to 16 years.
Clinical manifestations and laboratory findings of admitted cases of E. histolytica gastroenteritis in the 2 main age groups.
| Age <1 year (n=44) | Age 1–16 years (n=76) | p value | |||
|---|---|---|---|---|---|
| Number | % | Number | % | ||
| Clinical manifestations | |||||
| High grade fever ≥39°C | 28 | 63.6 | 49 | 64.5 | 0.89 |
| Intolerance to oral feeding | 31 | 70.5 | 35 | 46.1 | 0.009** |
| Frequent vomiting | 21 | 47.7 | 28 | 36.8 | 0.24 |
| Frequent loose motions | |||||
| ≥5 times/day | 34 | 77.3 | 17 | 22.4 | <0.001*** |
| Abdominal pain | 5 | 11.4 | 45 | 59.2 | <0.001*** |
| Bloody diarrhea | 14 | 31.8 | 23 | 30.3 | 0.85 |
| Dehydration | 27 | 61.4 | 11 | 14.5 | <0.001*** |
| Laboratory findings | |||||
| Leukocytosis for age | 29 | 65.9 | 39 | 57.4 | 0.15 |
| Neutrophilic leukocytosis for age | 26 | 59.1 | 37 | 50 | 0.27 |
| Positive CRP | 19 | 43.2 | 41 | 55.4 | 0.25 |
No significant differences were found between the studied groups in the risk factors of gastroenteritis including mother's or father's level of education, income, practice of washing hands before eating, type of drinking water, contact with farm animals, and performing agricultural work (p values >0.05). Considering odds ratios, small risk to have E. histolytica was found in comparison with either group II (OR 1) or group III (OR 2) as regards mother's level of education (OR 1: 1.01) or father's level of education (OR 1: 1.64), income (OR 1: 1.07, OR 2: 1.38), contact with farm animals (OR 1: 1.05) and performing agricultural work (OR 1: 1.13), but higher risk was associated with drinking water from wells in jars (OR 1: 2.14). All families of patients with GE were using or used tap water from home tanks for non-drinking purposes. Table 3 shows the risk factors for gastroenteritis in the studied groups.
Comparison of the risk factors for gastroenteritis between the studied groups.
| Variable | E. histolyticaGroup I (n=120) | RVGroup II (n=113) | Non-E. histolytica, non-RVGroup III (n=367) | Odds ratio(95% CI) | p values | |||
|---|---|---|---|---|---|---|---|---|
| Mother level of education | ||||||||
| Secondary school and less (Number, %) | OR 1 =1.01 (0.58–1.79) | p1=0. 95 | ||||||
| 45 | 37.5 | 42 | 37.2 | 145 | 39.5 | OR 2=0.92 (0.59–1.43) | p2=0.65 | |
| p3=0.24 | ||||||||
| Father level of education | ||||||||
| Secondary school and less (Number, %) | OR 1=1.64 (0.95–2.85) | p1=0.057 | ||||||
| 70 | 58.33 | 52 | 46.01 | 202 | 55.04 | OR 2=0.87 (0.56–1.35) | p2=0.52 | |
| p3=0.09 | ||||||||
| Income less than 1800 Saudi RS=500$US | ||||||||
| (Number, %) | 112 | 93.3 | 105 | 92.9 | 334 | 91 | OR 1=1.07 (0.35–3.26) | p1=0.90 |
| OR 2=1.38 (0.59–3.35) | p2=0.42 | |||||||
| p3=0.52 | ||||||||
| No practice of washing hands before eating | ||||||||
| (Number, %) | 10 | 8.3 | 13 | 11.5 | 67 | 8.1 | OR 1=0.70 (0.27–1.79) | p1=0.41 |
| OR 2=0.41 (0.19–15.7) | p2=0.95 | |||||||
| p3=0.27 | ||||||||
| Inadequate breastfeeding | ||||||||
| (Number, %) | 103 | 85.3 | 46 | 40.7 | 151 | 41.1 | OR 1=8.82 (4 .48–15.7) | p1<0.001*** |
| OR 2=8.67 (4 .84–15.7) | p2<0.001*** | |||||||
| p3=0.93 | ||||||||
| Drinking water wells in jars | ||||||||
| (Number, %) | OR 1=2.14 (0.75–16.75) | p1=0.52 | ||||||
| 120 | 100 | 111 | 98.2 | 361 | 98.4 | OR 2=0.94 (0.23–3.16) | p2=0.52 | |
| p3=0.92 | ||||||||
| Contact with farm animals | ||||||||
| (Number, %) | 10 | 8.3 | 9 | 7.9 | 31 | 8.4 | OR 1 =1.05 (0.38–2.95) | p1=0.91 |
| OR 2=0.99 (0.98–2.18) | p2=0.96 | |||||||
| p3=0.87 | ||||||||
| Agricultural work | ||||||||
| (Number, %) | 13 | 10.8 | 11 | 9.7 | 29 | 7.9 | OR 1=1.13 (0.45–2.84) | p1=0.78 |
| OR 2=1.42 (0.67–2.95) | p2=0.99 | |||||||
| p3=0.53 | ||||||||
p1 group I versus group II; p2 group I versus group III; p3 group II versus group III; OR 1=group I versus group II;OR 2=group I versus group III.
Significantly higher percentage of inadequate breastfeeding among E. histolytica cases (mainly in infants under 1 year; 41/44=93.2%) was observed compared to the other 2 groups (p1<0.001, and p2<0.001, respectively, and OR 1=8.82 (95% CI: 4.48–15.7), OR 2=8.67 (95% CI: 4.84–15.7) (Table 3).
The laboratory findings presented significantly higher percentage of leukocytosis for age, neutrophilic leukocytosis for age, and positive CRP in E. histolytica cases compared to the other 2 groups (p1<0.001 and p2<0.001 for leukocytosis, p2<0.001 for neutrophilic leukocytosis, and p1<0.001 and p2=0.02 for positive CRP) (Table 4). No bacteria were isolated from blood cultures in these cases.
Comparison of the laboratory findings between the studied groups.
| Variable | E. histolyticaGroup I (n=120) | RVGroup II (n=113) | Non-E. histolytica, non RVGroup III (n=367) | Odds ratio(95% CI) | p values | |||
|---|---|---|---|---|---|---|---|---|
| Leukocytosis for age | ||||||||
| (Number, %) | 68 | 56.7 | 7 | 6.2 | 32 | 8.7 | OR 1=19.8 (8.05–50.9) | p1<0.001* |
| OR 2=13.69 (7.69–23.64) | p2<0.001* | |||||||
| p3=0.78 | ||||||||
| Neutrophilic leukocytosis for age | 63/68 | 5/7 | 14/32 | OR 1=5.04 (0.52–44.8) | p1=0.06 | |||
| OR 2=16.2 (4 .46–60.92) | p2<0.001* | |||||||
| p3=0.18 | ||||||||
| Positive CRP | ||||||||
| (Number, %) | 60 | 50 | 13 | 11.5 | 73 | 20 | OR 1=7.69 (3.73–16.12) | p1<0.001* |
| OR 2=4.03 (2.53-6.41) | p2=0.02* | |||||||
| p3=0.52 | ||||||||
p1 group I versus group II; p2 group I versus group III; p3 group II versus group III; OR 1=group I versus group II; OR 2=group I versus group III.
No septic or other complications or mortality occurred in all our E. histolytica cases apart from a 7-year-old Pakistani boy who developed confirmed acute amebic appendicitis on the 3rd day of his admission when fever, vomiting and loose motions were improved but abdominal pain was persistent and localizing to the right iliac fossa with rebound tenderness and guarding. His laboratory investigations revealed hemoglobin of 12.8g/dL, total leukocyte count of 16.600/mm3 with neutrophils 84%, and platelets count of 459.000/mm3. CRP was positive at 60mg/dL. Stool examination showed trophozoites of E. histolytica along with mucus, pus, and blood. Amoebic colitis was confirmed by the presence of E. histolytica antigen in stools. Follow-up abdominal ultrasound documented the appearance of free peritoneal fluid and acute appendicitis was suspected. At laparotomy, an inflamed appendix without any perforation was found, but no other abnormalities. Histological sections of the surgical specimen showed changes typical of acute suppurative appendicitis. Microscopic examination revealed mucosal ulceration with multiple round-to-oval trophozoites of E. histolytica infiltrating the ulcerated mucosa. Many of the trophozoites were hematophagous or with erythrophagocytosis characteristic for E. histolytica. Thus, a diagnosis of acute amoebic appendicitis was made.20
E. histolytica cases showed favorable response to our protocol of treatment that included a combination of metronidazole infusion with or without intravenous 3rd generation cephalosporine (ceftriaxone), with regression and/or disappearance of symptoms within a mean duration of 3 days and confirmed by negative stool examination for E. histolytica trophozoites.
DiscussionIn this study, admitted cases of GE at our two main hospitals, during the period of the study of one year, were found to be 738 cases out of 1325 (55.7%) total pediatric cases admitted during the same period. So, they represented a major sector of admitted cases (even more than the cases admitted for respiratory illnesses). This showed that GE was a common public health problem in this locality.
Cases admitted with confirmed E. histolytica (120) constituted 20% of total admitted GE cases which was even more than the percentage of admitted cases of GE due to RV (113 cases, 18.8%). The confirmation for E. histolytica infection was mainly based on the results of E. histolytica antigen detection test which proved to have better sensitivity (>90%) and specificity for detection of E. histolytica infection than traditional microscopic examination of stool samples.1,14 Moreover, these hospitalized E. histolytica cases had symptoms of GE, while E. dispar is usually non-pathogenic and associated with asymptomatic infection.1
The increased prevalence of E. histolytica among inpatient cases (20%), which was higher than the previously recorded prevalence of 8.3% in the same locality10 as well as other infectious agents of GE, might be related to the type of domestic water supply as 100% of E. histolytica cases used water from wells for drinking and tap water from home tanks for other purposes and this was associated with a higher risk to have E. histolytica than to have RV (OR 1: 2.14, 95% CI: 0.75–16.75). This risk factor was proved to be the sole factor significantly associated with high prevalence rates of E. histolytica infection of 9.2% in our locality in southwest region of Saudi Arabia compared to other endemic areas. Those who used desalinated water for drinking had the lowest degree of exposure to the risk of infection.21
Demographic factors such as age under one year in E. histolytica group compared to group III (OR 2: 1.48), male gender (OR 1: 1.32, OR 2: 1.1), and residence at south Jeddah (OR 1: 1.18, OR 2: 1.46) demonstrated small risk to have E. histolytica infection when E. histolytica group was compared to either group II (OR 1) or group III (OR 2). However, Saudi nationality was significantly more common among E. histolytica cases than the other 2 groups (p1=0.021, and p2=0.016, respectively), and Saudi nationality was associated with more risk to acquire E. histolytica (OR 1: 3.25 OR 2: 3.05).
Considerable number of infants under one year had E. histolytica (44/120, 36.7%), and this was considered as unusual presentation because transmission of E. histolytica is frequently associated with contaminated food and water, so young infants are not expected to develop amebiasis very often.7 However, the percentage of cases under one year of age was significantly higher in RV group than in E. histolytica group and non-E. histolytica, non-RV group and significantly lower median age was found in RV group compared to both E. histolytica group and non-E. histolytica, non-RV group. This was not strange for RV infection as RV is estimated to cause more than 125 million cases of diarrhea annually in children younger than 5 years of age and disease tends to be most severe requiring hospitalization in patients 3–24 months of age22 as found in our RV cases.
The percentage of male cases of E. histolytica (74/120, 61.7%) was higher than the percentage of male cases in the other 2 groups and male gender was associated with relatively higher risk to have E. histolytica infection (OR 1: 1.32, OR 2: 1.1). This was also observed in other studies where asymptomatic E. histolytica infection was equally distributed between the genders with higher proportion of men with invasive amebiasis that was related to male susceptibility to invasive disease in one study,23 and infection of E. histolytica was more prevalent in male hosts (22.36%) compared to female hosts (20.9%) in another study.24
Considering the clinical manifestations associated with cases of E. histolytica infection, infants less than 1 year presented with significantly more intolerance to oral feeding, frequent, loose motions, and dehydration as causes for hospital admission than children above one year of age who had more significant presentation with abdominal pain than infants. These may be explained by more liability of infants who had frequent diarrhea and oral feeding intolerance to consequently progress into dehydration, which is usually common in young infants than in children. The more common association of abdominal pain with older children might be due to their more age-related developmental maturity to express their feelings better than young infants who may just have non-specific crying. Considerable numbers of both infants below and above 1 year (63.6% and 64.5%, respectively) had unexpectedly high-grade fever that was usually documented in only 1/3 of patients in previous literatures.1
Regarding the laboratory findings in our E. histolytica cases, it was surprising that 50% or more of these cases had leukocytosis for age, neutrophilic leukocytosis for age, and positive CRP which were significantly higher in E. histolytica cases compared to the other 2 groups. These laboratory findings together with clinical manifestations such as high-grade fever and toxic state have been described usually with amebic liver abscess, the commonest form of invasive amebiasis,1,25,26 and rarely with severe amebic colitis in young children when the colon was found to be necrotic with several perforations leading to peritonitis.27,28 Only one E. histolytica case with clinical and laboratory features of invasive amebiasis was complicated by confirmed amebic appendicitis. However, abdominal ultrasound could not demonstrate any amebic liver abscess at the time of presentation as this may need much more time to form sizeable well-visualized abscess particularly if early adequate treatment for invasive amebiasis was not given unlike what happened in our cases. In addition, the possibility of concomitant bacteremia associated with severe amebiasis and intestinal mucosal injury (with or without perforation) allowing invasion of enteric bacteria was excluded by failure to recover any bacterial organism from the blood stream unless a low bacteremic-like state could not be detected by a single routine blood culture method.
However, these laboratory findings together with previously described severe clinical manifestations indicated the aggressive nature of E. histolytica infection in our cases and that an early invasive amebic disease might have been evolving unless adequate early diagnosis and treatment of E. histolytica infection was done.
Although the high percentages of severe manifestations indicating the invasive nature of E. histolytica in our cases can be attributed to the fact that we were dealing with only severe E. histolytica cases that required admission and not outpatient E. histolytica cases, the strikingly high percentages of E. histolytica infection in infants under one year as well as the encountered laboratory indicators of severe E. histolytica invasive disease were more common than expected or previously reported in literatures and even more severe than our hospitalized cases with GE due to enteropathogens other than E. histolytica. The possibility that a more virulent strain of E. histolytica was responsible for such serious manifestations in our cases need to be investigated as Petri29 suggested that genetically distinct strains of E. histolytica might exist but evidence was too preliminary to judge if some strains were more virulent than others. This aggressive presentation in our E. histolytica cases may also need further evaluation to reveal the possible underlying immunologic mechanism that might be responsible for such severe E. histolytica cases.
The most important risk factor to acquire E. histolytica infection was found to be related to breastfeeding practice with significantly higher percentage of inadequate breastfeeding among E. histolytica cases, especially infants under one year compared to the other 2 groups and OR 1=8.82 (95% CI: 4.48–15.7), OR 2=8.67 (95% CI: 4.84–15.7). This can be explained by the fact that colostrum and mature human milk have significant lethal effect on E. histolytica and protect against its infection in breast-fed children.30 This lethal effect is accomplished by bile salt-stimulated lipase in human milk, which kills G. lamblia and E. histolytica.31 Moreover, an important observation of inadequate exclusive breastfeeding and the common practice of bottle feeding among our cases of E. histolytica still persisted as documented in several studies conducted in different regions of Saudi Arabia, including our locality, Jeddah, in the western region of the kingdom. These studies were alarming for an extremely low prevalence of exclusive breastfeeding in Saudi population which was very far from compliance with even the most conservative World Health Organization recommendations of exclusive breastfeeding for 4–6 months. Partial breastfeeding was the trend for feeding in the first 6 months of life, which was accompanied by a rapid decline in lactation duration. The single most common reason cited for the early introduction of bottle feeding was that breast milk was insufficient. Because of this tendency, many mothers practice mixed feeding.32–37 Therefore, the high prevalence of E. histolytica in infants less than one year in this study was mostly related to the absence of a main protective factor which is breastfeeding.
Limitations of the studyThis study included only 2 main hospitals at south Jeddah; it would have been better if it could include more hospitals in various regions of Jeddah city to be a multicenter study. However, the numbers of included patients admitted to our hospitals represented a quite sufficient representative sample of the population in our locality. A study of the immunological factors and genetic analysis of the isolated E. histolytica would have been of value to explain the possible underlying mechanisms of severity of E. histolytica infection in Saudi infants and children.
ConclusionsE. histolytica had high prevalence and unusual presentation by affecting high proportion of infants under 1 year, severe clinical manifestations, and laboratory findings that were known to be usually encountered in invasive amebiasis as significant leukocytosis, neutrophilic leukocytosis for age, and positive CRP were found among more than 50% of admitted Saudi infants and children with E. histolytica infection in our locality. E. histolytica can be a re-emerging serious infection when it finds favorable environmental and host factors’ conditions mainly attributed to inadequate breast feeding in this study. This may occur at any other area of the world with the same risk factors, so we must be ready to this re-emerging danger with effective and more powerful preventive measures. It may be the time now for the need to E. histolytica vaccine to guard against this severe E. histolytica infection.
RecommendationsThis study raised the need for targeted breastfeeding education. Health care providers should be encouraged to continuously educate Saudi women on the benefits of breastfeeding. There may be a need to revise the media campaign for promoting breastfeeding.
Improved water supplies should be used, including protection of community wells and domestic storage tanks, together with mandatory inspection measures during transportation and distribution of commercial water to reduce the rate of infection with E. histolytica as well as other infectious agents of GE in this locality.
Conflict of interestThe authors have no conflict of interest to declare.