To compare the prognostic value of the pneumonia severity index and the severity score for community-acquired pneumonia (CURB-65) in predicting mortality and the need for ICU admission of patients with community-acquired pneumonia referred to our emergency department.
Materials and methodsThis prospective study was performed on patients with community-acquired pneumonia admitted to the emergency department of Imam Hossein Medical Center, Tehran, Iran. A questionnaire with demographic information, clinical signs and symptoms, laboratory and radiographic findings was completed for each patient. The information required for calculating the pneumonia severity index and CURB-65 were extracted from the medical records. The patients’ clinical outcome was also recorded within a month after admission.
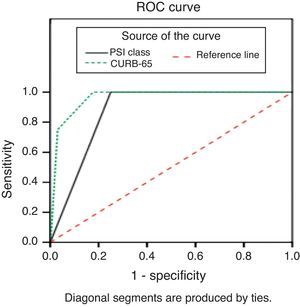
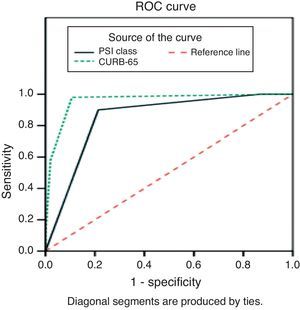
ResultsWe studied 200 patients with community-acquired pneumonia (122 men, 78 women). The sensitivity and specificity of CURB-65 in predicting mortality were 100% and 82.3%, respectively. As for pneumonia severity index, the rates were 100% and 75%, respectively. The sensitivity and specificity rates of CURB-65 and pneumonia severity index in predicting mortality and need for ICU admission were 96.7% and 89.3%, and 90% and 78.7%, respectively.
ConclusionCURB-65 seems to be the preferred method to predict mortality and need for ICU admission in patients with community-acquired pneumonia. Despite their comparable specificity and sensitivity, CURB-65 is much easier to implement.
Community acquired pneumonia is a common disease with a lifetime prevalence of 20–30% in developing and 3–4% in developed countries.1 The mortality rate among hospitalized patients diagnosed with the condition has been reported to range from 4% to 21% in different settings.1 The rate is reported to be higher, even as high as 50%, among patients admitted to ICU.2
The condition imposes a heavy burden on the healthcare system in terms of its high cost both for diagnosing and treating the condition as well as for the hospital and ICU stay.3 This heavy cost points out the importance of predicting the need for hospitalization (ICU or ward) as well as the outcome of these patients.2
One of the earliest studies of outcome in community acquired pneumonia was conducted in 1982 by the British Thoracic Society. In this study 453 adult patients were evaluated in 25 medical centers. Patients who had two of the three risk factors were described as being 21 times more likely to die because of their condition. Based on these findings, the British Thoracic Society devised the BTS1 scoring system which has shown a high predictive value compared to other indices in this regard.4,5
In 1997, Fine et al. devised the pneumonia severity index (PSI) method based on their study of more than 50,000 outpatients and also hospitalized patients diagnosed with community acquired pneumonia. This scoring system, which divided the patients into five main categories based on their 30-day prognosis prediction, also showed acceptable predictive values.6
The main concern while designing PSI was the management of outpatients at high risk of dying from the disease. The predictive value of PSI in these patients was later confirmed by several other studies.5–7 The main shortcoming of PSI was the fact that age was not a predictive component in this index. Later on, PSI scoring system was recommended by the Infectious Diseases Society of America as a predicting tool for patients with community acquired pneumonia.6
The severity score for the community acquired (CURB-65) and the PSI are two of the most prominent methods in this regard.2,3,8–12 The efficacy of these two clinical prediction rules (CPRs), however, had never been compared in Iran or in any other regional countries.
Considering the high prevalence of community acquired pneumonia in Iran, the present study was designed to compare the prognostic value of these two CPRs in our emergency department (ED) as a model representing EDs in developing countries.
Patients and methodsStudy designThis observational comparative study was conducted on patients diagnosed with community acquired pneumonia, referred to the ED of Imam Hossein Medical Center in 2009. Imam Hossein hospital is a teaching general hospital where more than 70,000 patients are seen in its ED annually. The ethical board committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran, approved this study.
Study populationPatients aged 18 years or more diagnosed with community acquired pneumonia on the grounds of their clinical and paraclinical findings by the emergency and/or infectious disease residents and/or specialists were enrolled in the study. Those whose diagnosis changed during the course of treatment were excluded.
Study protocolA questionnaire including the demographic data, clinical, paraclinical and imaging findings of the patients was completed for each patient. PSI and CURB-65 scores were calculated for each patient. The CURB-65 is a 5-item index while PSI uses 20 items to predict the patient's outcome. An emergency medicine resident was responsible for filling out the questionnaires.
The need for ICU stay as well as the risk of dying was compared according to the calculated PSI and CURB-65 CPRs. The outcome of patients was also recorded within a month after their admission at the hospital.
Data analysisData were analyzed using SPSS ver 13. Results were expressed as mean±SD. Student's t-test was used for statistical comparisons. Sensitivity, specificity, and relative risks were calculated for each study outcome using standard formulas.
ResultsTwo hundred patients with community-acquired pneumonia were enrolled (122 males, 78 females). Their mean age was 68±18 years, ranging from 18 to 68 years.
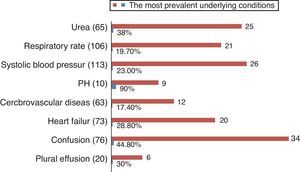
Among these patients 148 (74%) were hospitalized in different hospital wards and 52 (26%) were admitted to ICU. The most common cause of the condition in males under the age of 50 was injection drug abuse and high blood glucose (Fig. 1). In females of the same age, however, viral diseases (influenza) and high blood glucose were the prevailing causes. The most common underlying condition in the whole population was heart failure.
Overall, 36 patients died (18%) during the study period; of those, six had been hospitalized in different wards and the remaining 30 were admitted to ICUs. Thirty patients died in hospital, whereas six died in the 30-day follow-up period after discharge.
The average hospital length of stay for patients with community-acquired pneumonia categorized as classes 1 and 2 based on the PSI scoring system was two days, three days for class 3, five days for class 4, and 10.5 days for class 5. For CURB-65, these values were two days for classes 1 and 2, 14.5 days for class 3, and nine days for higher classes.
Heart failure and age were both significantly associated with mortality (p<0.05). Among clinical and paraclinical findings, having cardiovascular disease as the underlying condition, low blood pH and high urea levels, and decreased consciousness level were statistically correlated with mortality (p<0.05).
The distribution of patient's outcome based on their PSI and CURB-65 scores is shown in Tables 1 and 2.
All 36 deaths occurred in patients with PSI levels of 5 and higher. There was 12% discordance between decisions on the need for hospitalization or the type of ward the patient was to be admitted when using CURB-65. As for PSI, the rate was high as 27.5%. The highest discordance rate was reported in patients categorized as class three and higher using CURB-65. Six of the 14 patients who were admitted in a ward, instead of ICU, died.
Based on PSI scoring system, the majority of discordances were reported in patients categorized as classes 3–5, with the highest occurring with patients of class 5. Among the 30 patients who should have been admitted to ICU but were hospitalized in a ward, there were six deaths during the study period.
Sensitivity, specificity, positive and negative predictive values, and diagnostic accuracy of CURB-65 in predicting mortality were 100%, 82.3%, 55.4%, 100% and 85.5%, respectively. The same rates for PSI were 100%, 75%, 46.8%, 100% and 79.5%, respectively (Table 3). Table 4 shows the efficacy of the two tools in forecasting ICU admission (Table 4).
Sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy of PSI and CURB 65 methods in forecasting mortality.
| Class | Sensitivity | Specificity | PPV | NPV | DA |
|---|---|---|---|---|---|
| PSI | |||||
| II | 100 (90.4, 100) | 2.4 (0.9, 6.1) | 18.4 (13.6, 24.4) | 100 (51.0, 100) | 20 (15.1, 26.1) |
| III | 100 (90.4, 100) | 4.3 (2.1, 8.5) | 18.7 (13.8, 24.7) | 100 (64.6, 100) | 21.5 (16.4, 27.7) |
| IV | 100 (90.4, 100) | 12.2 (8.0, 18.1) | 20 (14.8, 26.4) | 100 (83.4, 100) | 28.0 (22.2, 34.6) |
| V | 100 (90.4, 100) | 75 (67.9, 81.0) | 46.8 (36.0, 57.8) | 100 (98.0, 100) | 79.5 (73.4, 84.5) |
| CURB-65 | |||||
| I | 100 (90.4, 100) | 0.6 (0.1, 3.4) | 18.1 (13.4, 24.0) | 100 (20.6, 100) | 18.5 (13.7, 24.5) |
| II | 100 (90.4, 100) | 5.5 (2.9, 10.1) | 18.9 (13.9, 25.0) | 100 (70.1, 100) | 22.5 (17.3, 28.8) |
| III | 100 (90.4, 100) | 82.3 (75.8, 87.4) | 55.4 (43.4, 66.8) | 100 (97.2, 100) | 85.5 (80.0, 89.7) |
| IV | 75 (58.9, 86.3) | 97.0 (93.1, 98.7) | 84.4 (68.3, 93.4) | 94.6 (90.1, 97.2) | 93.0 (88.6, 95.8) |
| V | 11.1 (4.4, 25.3) | 99.4 (96.6, 99.9) | 80 (37.6, 96.4) | 83.6 (77.8, 88.1) | 83.5 (77.7, 88) |
Sensitivity, specificity, positive value, negative predictive value and diagnostic accuracy and their relative 95% CI of PSI and CURB-65 methods in forecasting ICU admission.
| Class | Sensitivity | Specificity | PPV | NPV | DA |
|---|---|---|---|---|---|
| PSI | |||||
| II | 100 (92.9, 100) | 2.7 (1.0, 6.7) | 25.5 (19.9, 32.0) | 100 (51.0, 100) | 27.0 (21.3, 33.5) |
| III | 100 (92.9, 100) | 4.7 (2.3, 9.3) | 25.9 (20.2, 32.5) | 100 (64.6, 100) | 28.5 (22.7, 35.1) |
| IV | 100 (92.9, 100) | 13.3 (8.8, 19.7) | 27.8 (21.8, 34.7) | 100 (83.9, 100) | 35 (28.7, 41.8) |
| V | 90 (78.6, 95.7) | 78.7 (71.4, 84.5) | 58.4 (47.3, 68.8) | 95.9 (90.8, 98.3) | 81.5 (75.5, 86.3) |
| CURB-65 | |||||
| I | 100 (88.7, 100) | 0.7 (0.1, 3.7) | 16.8 (12.0, 22.9) | 100 (20.7, 100) | 17.2 (12.4, 23.4) |
| II | 100 (88.7, 100) | 6 (3.2, 11.0) | 17.5 (12.6, 23.9) | 100 (70.1, 100) | 21.7 (16.3, 28.4) |
| III | 96.7 (83.3, 99.4) | 89.3 (83.4, 93.3) | 64.4 (49.8, 76.8) | 99.3 (95.3, 99.9) | 90.6 (85.4, 94.0) |
| IV | 30 (16.7, 47.9) | 98.0 (94.3, 99.3) | 75.0 (46.8, 91.1) | 87.5 (81.7, 91.7) | 86.7 (80.9, 90.9) |
| V | 16.7 (7.3, 33.6) | 100 (97.5, 100) | 100 (56.6, 100) | 85.7 (79.8, 90.1) | 86.1 (80.3, 90.4) |
Receiver operating characteristic (ROC) curves for the prediction of mortality and need for ICU admission using PSI and CURB-65 are shown in Figs. 2 and 3, respectively. CURB-65 showed a better predictive value in foreseeing both the need for ICU admission and mortality than PSI.
DiscussionAlthough there are strong similarities between these two methods at first glance, important differences make them unique. PSI uses a long list of predicting factors and its implementation needs various clinical and paraclinical information while CURB-65 is designed to be as simple as possible using a limited set of information.
Based on the nature of these two tools, their predictive value largely depends on the environment in which they are implemented. In a hospital setting in developing countries like Iran with scarce resources, simple methods such as CURB-65 are preferred as they put less pressure on the country.
In line with previous studies, both PSI and CURB-65 showed high negative predictive value and low positive predictive value in predicting mortality and the need for ICU admission.6,7 In our results, however, CURB-65 had better accuracy in predicting mortality and the need for ICU admission among patients with community-acquired pneumonia. While CURB-65 had a high sensitivity in predicting mortality and need for ICU admission, PSI was shown to have a high specificity in this regard. Both indices can therefore be used even in low risk patients as a guide for early discharge.
According to other studies, the mortality risk and the need for ICU admission were higher as the scores increased in both PSI and CURB-65.4,7 Our study, similarly, revealed that the mortality increased with age, presence of underlying heart failure, high blood levels of urea, pH lower than 7.35, and decreased consciousness level. The most common underlying condition in this study was heart failure, which had a statistically significant relation with mortality, whereas decreased consciousness level was associated with higher mortality. Musher et al. in a study on 170 patients with community-acquired pneumonia found heart conditions namely CHF in 33 (19.7%) of the patients.13 Corroborating our results, Lichman et al. reported that 6.8% of their patients had severe heart diseases.14
In a study by Man et al. on 1016 patients with community-acquired pneumonia, authors compared the outcome of patients categorized as level 4 and 5 using CURB-65 and PSI methods. Their results indicated that being level 5 by CURB-65 had the best predictive value for patients with community-acquired pneumonia admitted to the ED.15 In line with our results, Shah et al. reported both PSI and CURB-65 to have equal sensitivity to predict death from community-acquired pneumonia, adding that PSI was more sensitive in predicting ICU admission than CURB-65.1 This may be because CURB-65 model does not consider decompensated co-morbidity due to community-acquired pneumonia and results in limited application in the elderly.16 In another study PSI was reported to have the highest sensitivity followed by CURB-65 in predicting mortality. For predicting ICU admission, however, other indices such as modified ATS, SMART-COP and IDSA/ATS were reported to perform better than PSI and CURB-65,17 as these indices were originally designed to assess ICU admission rather than mortality. Therefore, a poor performance could be found if applied in predicting mortality.
LimitationConsidering the limited number of ICU beds in our hospital, it is possible that certain patients were admitted to different wards due to unavailability of ICU beds. Not having an available ICU bed may have affected the physician's decision on whether the patient needed ICU admission.
ConclusionThe severity score for community-acquired pneumonia seems to be the preferred method to predict the need for ICU admission and the prognosis of patients seen at EDs. Despite having comparable specificity and sensitivity with PSI, CURB-65 is much easier to be implemented.
Conflict of interestAll authors declare to have no conflict of interest.