Organizing pneumonia emerges as a late phase complication of COVID-19. Corticosteroids are standard therapy for organizing pneumonia, but the question of whether an approach with high dose corticosteroids would be beneficial for patients with organizing pneumonia secondary to COVID-19 remains to be answered.
Herein we report a series of three patients, one male and two females, mean age 58.3 years old, admitted for COVID-19 with severe pulmonary disease requiring ventilatory support. The patients underwent chest computed tomography scans due to maintained hypoxemia, which showed a pattern compatible with organizing pneumonia. The patients were treated with a high dose of corticosteroids (prednisone 1 mg/kg PO), showing marked clinical improvement, and decreasing oxygen flow ratio demand. They were discharged after a mean period of 6.3 days of hospitalization.
Our report suggests that patients with COVID-19 with organizing pneumonia might benefit from high dose corticosteroids as an adjuvant therapy.
In patients suffering from COVID-19, lung involvement is most commonly characterized by ground-glass opacification with or without consolidative abnormalities, consistent with viral pneumonia.1 Additionally, the pattern of organizing pneumonia (OP) on computed tomography (CT) scan of the chest has been reported, mostly as a late phase complication. Main tomographic findings include ground-glass opacities, consolidation, reticulation, and parenchymal distortion.2–4
OP consists of granulation tissue and proliferation of fibroblasts within the lung parenchyma. It is histologically defined as an intra-alveolar organized exudate composed of myofibroblasts and connective tissue with variable interstitial inflammation.5 Viral infections are among the most common etiologies of secondary OP.3,6
Corticosteroids are the standard therapy for OP, and patients usually experience pronounced clinical response within a few days.5 The question of whether an approach with a high dose of corticosteroids would be beneficial for patients with OP secondary to COVID-19 remains to be answered. Herein we report a series of three cases with OP that responded dramatically to corticosteroids. To the best of our knowledge, this is the first report to analyze this issue.
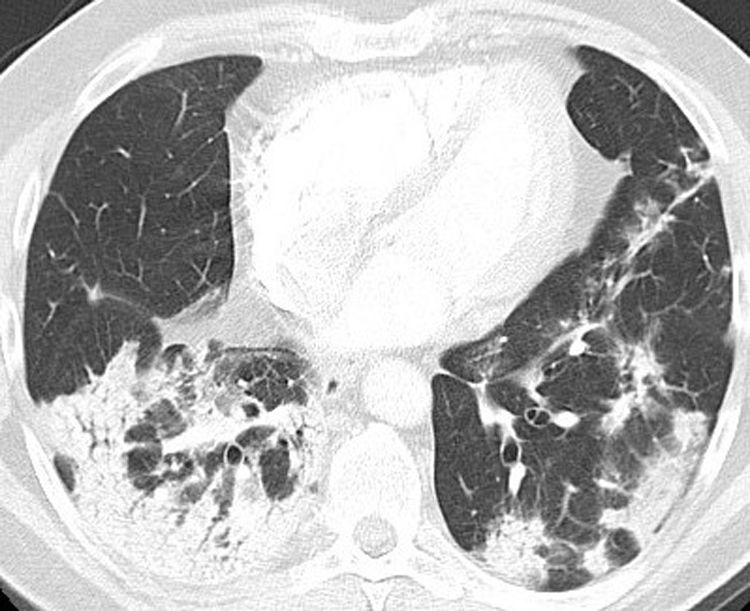
Case reportsPatient 152-year-old white male. His prior medical record was unremarkable. He had a positive RT-PCR for SARS-CoV-2 on the 11th day of symptoms. Prior to admission, he had used azithromycin and amoxicillin-clavulanate. A chest X-ray (CXR) upon admission showed a slight infiltrate on the right lower lobe. On day 1 of hospitalization, he was started on a daily dose of dexamethasone at 6 mg PO. Four days later, continuous positive airway pressure (CPAP) was also started. Throughout the following 10 days (on illness day 21), his P/F ratio on arterial blood gas trended upwards from 85 to 230 despite sustaining dyspnea, fever, leukocytosis, and high titers of C-reactive protein. He then underwent a CT scan, which revealed a pattern compatible with OP (Fig. 1). Soon after being started on prednisone at 1 mg/kg PO, CPAP was stopped, and oxygen support was switched to low-flow nasal cannula. He rapidly experienced significant improvement in both symptoms and laboratory tests. He was finally discharged on day 11 of prednisone use after a full recovery.
Pulmonary CT angiography to assess pulmonary embolism (PE) obtained on illness day 21. CT axial image (lung window) showed peripheral areas of consolidation in both lower lobes. Incipient architectural distortion is seen in central portions of the lungs. CT findings were suggestive of OP. PE was absent.
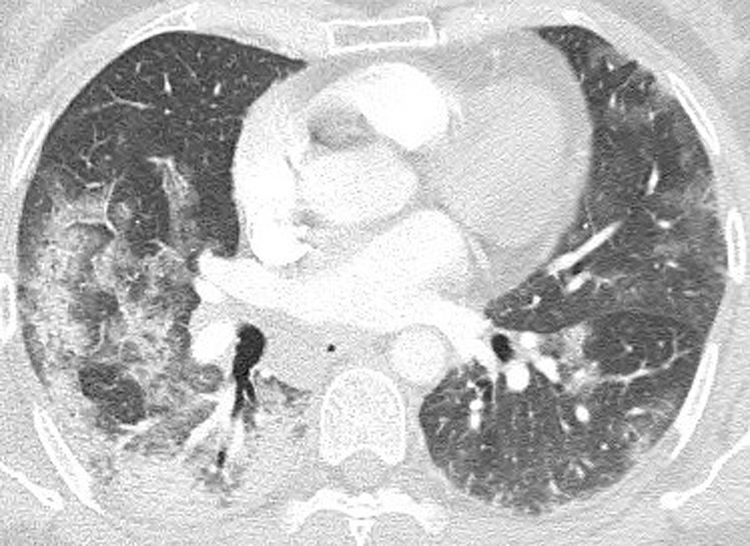
60-year-old white woman who was a former smoker. She presented to the hospital with a 5-day onset of low-grade fever, cough, dyspnea, and odynophagia; she had been using amoxicillin-clavulanate for the previous 4 days and tested positive for SARS-CoV-2 at admission. At the emergency department, she was started on cefepime later switched to meropenem due to clinical and laboratory deterioration. On admission, a CXR showed scarce bilateral opacities. Dexamethasone was started on day 1 of hospitalization, and CPAP was started on day 10 (when her P/F ratio on arterial blood gas was 61.6). Since her clinical status showed little improvement, she underwent a CT scan on day 14, exhibiting signs of OP (Fig. 2). Prednisone was started on the following day at 1 mg/kg PO, and in less than 48 h, she tolerated a tapering off of ventilatory support. She was discharged, breathing on room air, after four days of a high dose corticosteroid.
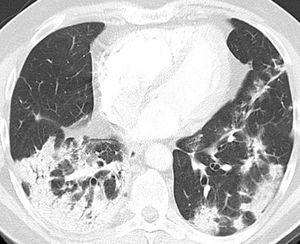
Patient 363-year-old white female with an unremarkable prior medical history. She presented on day 14 of her illness with shortness of breath. Her P/F ratio was 150 on arterial blood gas, and high-flow oxygen support was started through a reservoir mask. A CPAP was installed on the following day, and dexamethasone was prescribed. She completed a course of both azithromycin and amoxicillin-clavulanate. No clinical improvement was noted, and the patient received a CT scan. The CT scan revealed a pattern of OP (Fig. 3), and corticosteroids were started at 1 mg/kg PO daily. After three doses, the patient was ventilating on low-flow nasal cannula. She improved considerably and had no dyspnea on exertion (Table 1).
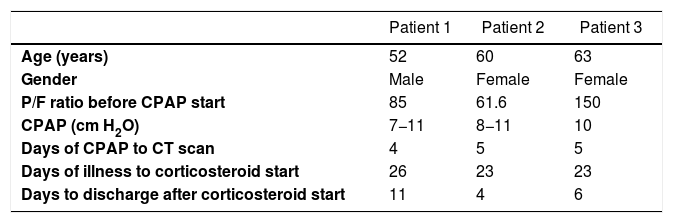
Main clinical and laboratory characteristics.
| Patient 1 | Patient 2 | Patient 3 | |
|---|---|---|---|
| Age (years) | 52 | 60 | 63 |
| Gender | Male | Female | Female |
| P/F ratio before CPAP start | 85 | 61.6 | 150 |
| CPAP (cm H2O) | 7−11 | 8−11 | 10 |
| Days of CPAP to CT scan | 4 | 5 | 5 |
| Days of illness to corticosteroid start | 26 | 23 | 23 |
| Days to discharge after corticosteroid start | 11 | 4 | 6 |
P/F: partial pressure of oxygen (pO2)/ fraction of inspired oxygen (FiO2).
CPAP: continuous positive airway pressure.
Our clinical scenarios encompassed patients diagnosed with the novel coronavirus and in need of oxygen support. All of them received a 10-day course of dexamethasone, broad-spectrum antibiotics, and continuous positive airway pressure. Notwithstanding, little progress had been made in their clinical status. For further evaluation of other reasons why these patients were not improving, CT scans of the chest were ordered. A similar pattern of OP was observed in each of the CT scans. All patients received prednisone at 1 mg/kg PO and experienced rapid improvement: they were weaned off ventilatory support and discharged within a few days.
In patients with SARS-CoV-2 showing clinical deterioration despite optimized therapy and ventilatory support, or experiencing worsening symptoms after initial improvement, CT scans might be useful for ruling out complications such as pulmonary embolism, secondary pneumonia, or OP. In this series, patients presented with an average of 24 days (23–26 days) from symptom onset to having a CT scan, and remained on CPAP for an average of 4.6 days (4–5 days) before imaging was performed. Once prednisone was initiated, their mean length of stay was of 7 days (6–11 days). This time frame might pose an attractive strategy if additional imaging investigation should be considered for such patients.
Secondary OP has been reported in various viral infections, such as H1N1, H7N9, and the Middle East respiratory syndrome coronavirus infection (MERS). Glucocorticoids in moderate to high doses are the mainstays for treating severe cases of OP, and often result in rapid clinical and radiological improvement.7–9 Clinical response within the first days of corticoid therapy is described as dramatic; prolonged treatment is usually not necessary.5
Clinical improvement was seen in all cases reported, suggesting that patients experiencing OP secondary to SARS-CoV-2 might benefit from high doses of corticosteroid, regardless of previous dexamethasone use. Nonetheless, there are no current large-scale epidemiological data assessing this condition as a complication of SARS-CoV-2 infection, including incidence, clinical course, treatment, or clinical outcomes.
We suggest that further evaluation with thoracic imaging is warranted for inpatients with COVID-19 showing little or no progress despite optimized therapy because these patients might benefit from early diagnosis and appropriate, specific management. The features of OP found through imaging should prompt the use of high-dose corticosteroids, even following a 10-day course of dexamethasone.
Disclosure statementThe authors have no conflicts of interest to declare.
Funding sourcesThe authors did not receive any grants or fellowships supporting the writing of the paper.