In March 2020, telemedicine and HIV self-testing were adopted by Brazilian Public Health services to minimize disruptions in pre-exposure prophylaxis (PrEP) access and delivery during the COVID-19 pandemic. To understand the acceptability of PrEP teleconsultation and HIV self-testing, we conducted a web-based study during social distancing period (April–May, 2020) among men who have sex with men and transgender/non-binary individuals using social media. Out of the 2375 HIV negative respondents, 680 reported PrEP use and were included in this analysis. Median age was 33 years (IQR: 28–40), 98% cisgender men, 56% white, 74% high education, and 68% middle/high income. Willingness to use HIVST was 79% and 32% received an HIV self-testing during social distancing period. The majority reported preference for PrEP/HIV self-testing home delivery instead of collecting at the service. PrEP teleconsultation was experienced by 21% and most reported feeling satisfied with the procedures. High acceptability of PrEP teleconsultation was reported by 70%. In ordinal logistic model, having higher education was associated with high aceptability of PrEP teleconsultation (aOR:1.62; 95%CI: 1.07–2.45). Our results point out that PrEP teleconsultation and PrEP/HIV self-testing home delivery could be implemented by PrEP services in Brazil to avoid PrEP shortage during the COVID-19 pandemic and thereafter as an option to increase retention and adherence.
The number of cases of the novel coronavirus (SARS-CoV-2) disease 2019, or “COVID-19”, continues to rise in Brazil. From February 26, 2020 to December 12, 2020 there have been more than 6,781,799 confirmed cases and almost 180,000 deaths in the country.1 Social distancing and community containment measures have been adopted in the country since March 2020 to avoid the spread of COVID-19. As such, health services offering PrEP in Brazil implemented a new framework to minimize disruptions in access and adherence to PrEP.
Worldwide, telemedicine procedures have been implemented and integrated within health systems to fight the COVID-19 pandemic.2,3 We have previously described telemedicine procedures for PrEP delivery adopted at Instituto Nacional de Infectologia Evandro Chagas, Fundação Oswaldo Cruz (INI-Fiocruz) in Rio de Janeiro, Brazil which included teleconsultation and provision of HIV self-testing (HIVST).4 To understand the acceptability of PrEP teleconsultation and HIVST, we conducted a cross-sectional web-based study during social distancing period (April 16 to May 31, 2020), recruiting gay, bisexuals and other men who have sex with men (MSM) and transgender/non-binary (TGNB) individuals using a geosocial networking (GSN) app for sexual encounters (Hornet) and social media (Facebook and WhatsApp).
Individuals who met the eligibility criteria (age ≥18 years, MSM and TGNB individuals, Brazilian resident) and acknowledged to participate after reading the informed consent were directed to the online questionnaire programmed on SurveyGizmo®. Self-identifying heterosexual cisgender men and cisgender women were excluded from the study. Details of study design and methodology are described elsewhere.5 The survey instrument consisted of questions on demographics, sex during social distancing period, daily oral PrEP use, teleconsultation and HIVST. For this analysis, we included individuals reporting HIV negative status and receiving PrEP through the Brazilian Public Health System (SUS). The INI-Fiocruz institutional review board (#CAAE 82021918.0.0000.5262) reviewed and approved this study. No identification of participants was collected and no incentives were provided.
Variables collected were: age at the time of the survey (categorized in three brackets: 18 to 24; 25 to 35 and >35 years); gender in cisgender men vs. transgender/non-binary; race (categorized in White, Black, Pardo or Mixed-black); education (categorized in low [≤12 years or completed secondary school or less] and high [>12 years or more than secondary school]). We also collected data on family monthly income, grouped into the following strata considering Brazilian minimum wage (MW) in 2020 (R$1045 or US$180): low (up to 2 MW), middle (>2–6 MW), and high (>6 MW). Region was defined according to the Brazilian administrative division: North (7 states), Northeast (9 states), Central-west (3 states and Federal District), South (3 states), and Southeast (4 states). Participants were asked if they had sexual partners during social distancing period (sex abstinence, sex only with steady partners and sex with casual partners). Those reporting sex with casual partners were asked about condomless receptive anal sex. Participants were prompted to respond whether they continued using daily oral PrEP during this period.
Participants responded to questions about awareness, previous use and willingness to use HIVST. Willingness to use HIVST was definied as reporting “very likely” or “likely” to use HIVST. Those reporting previous use of HIVST were asked if they felt confortable using it (5-point Likert scale: very confortable to very unconfortable). PrEP users were prompted to respond if they experienced teleconsultation and whether they felt satisfied (5-point Likert scale: very satisfied to very unsatisfied). Respondents were also asked about their reliable information sources for questions/concerns about PrEP and HIVST and if they would prefer receiving PrEP refills at home instead of collecting them at the PrEP facility.
Acceptability of PrEP teleconsultation was assessed among respondents who have never experienced teleconsultation using the question: “How would you feel about taking a PrEP teleconsultation?” Possible response options varied from 1 (very comfortable) to 5 (very uncomfortable), with an additional option “I don’t have a mobile phone”. We considered high acceptability of PrEP teleconsultation if respondent reported “very comfortable” or “comfortable”. We used ordinal logistic regression model to assess the factors associated with high acceptability of PrEP teleconsultation; those reporting not having a mobile phone were removed from the model.
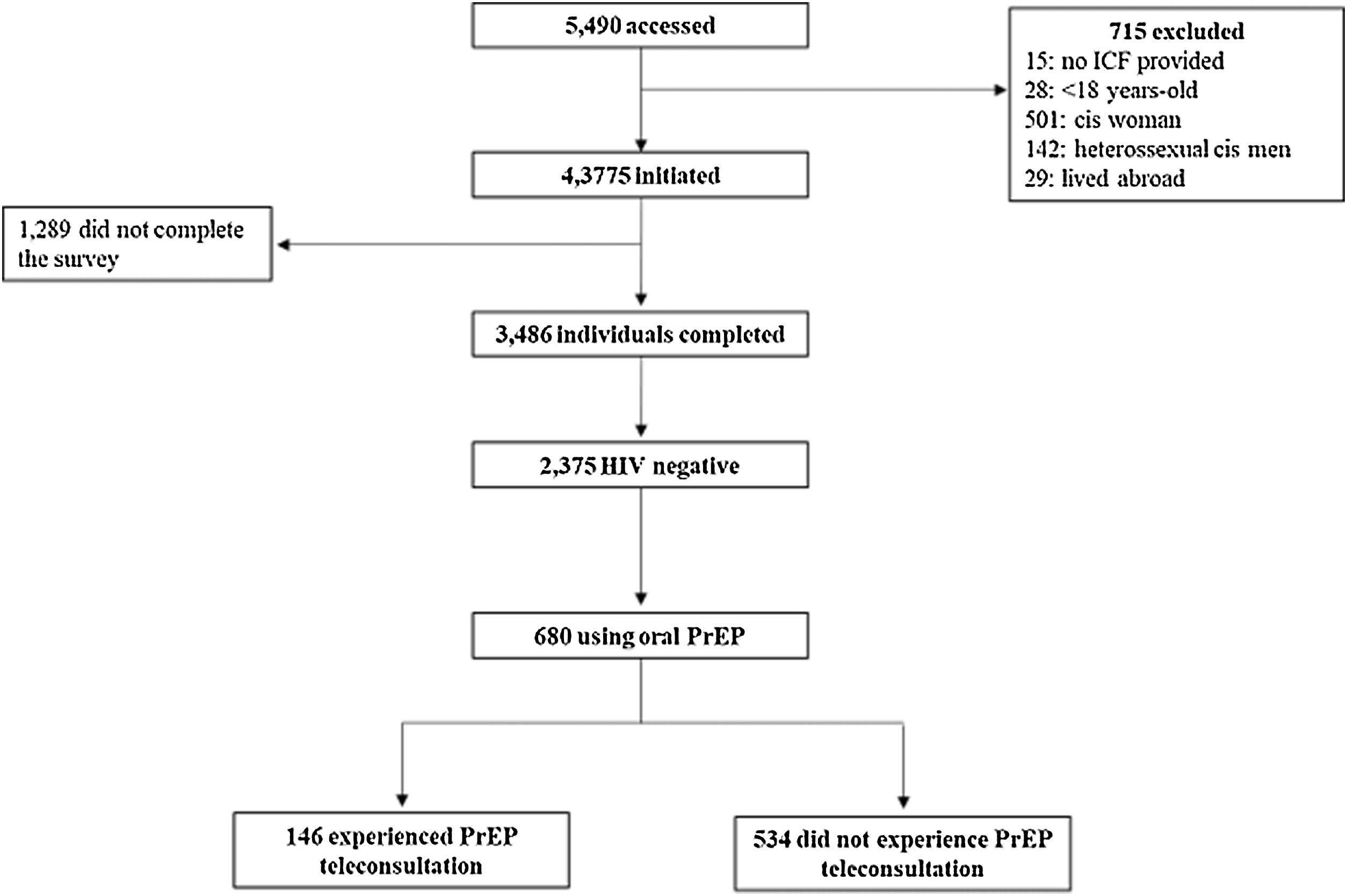
A total of 5490 individuals accessed the questionnaire; 715 (13.0%) did not meet inclusion criteria or did not consent, and 3486 (63.5%) completed it (Fig. 1). Of these, 2375 respondents self-reported HIV negative status, 30.9% (n=680) were on oral PrEP before social distancing recommendations through the Public Health System (SUS) [PrEP SUS (342/680; 50.3%) and the ImPrEP study (338/680; 49.7%)] and were included in this analysis.
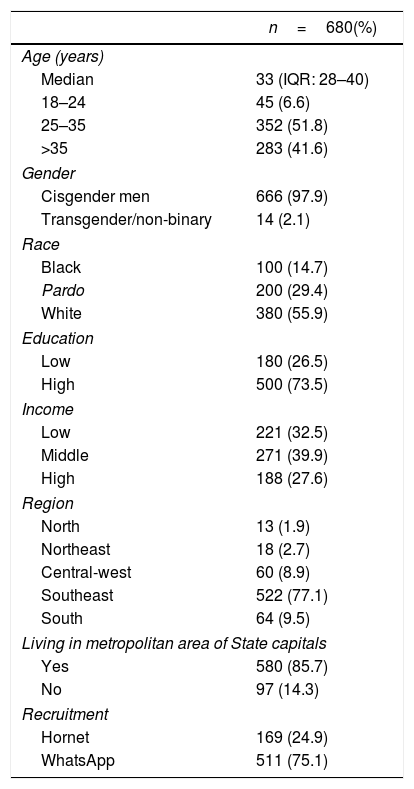
Median age was 33 years (IQR: 28–40), most were cisgender men (666; 97.9%), self-identified as gay (635; 93.4%) and had high education (500; 73.5%) (Table 1). More than half were white (380; 55.9%) and 67.5% (n = 459) declared middle/high income. Most of respondents were recruited on WhatsApp (511; 75.1%), reported living in Southeast Brazil (522; 77.1%) and in metropolitan areas of State Capitals (580; 85.7%).
Participants characteristics. Brazil, 2020.
| n=680(%) | |
|---|---|
| Age (years) | |
| Median | 33 (IQR: 28–40) |
| 18–24 | 45 (6.6) |
| 25–35 | 352 (51.8) |
| >35 | 283 (41.6) |
| Gender | |
| Cisgender men | 666 (97.9) |
| Transgender/non-binary | 14 (2.1) |
| Race | |
| Black | 100 (14.7) |
| Pardo | 200 (29.4) |
| White | 380 (55.9) |
| Education | |
| Low | 180 (26.5) |
| High | 500 (73.5) |
| Income | |
| Low | 221 (32.5) |
| Middle | 271 (39.9) |
| High | 188 (27.6) |
| Region | |
| North | 13 (1.9) |
| Northeast | 18 (2.7) |
| Central-west | 60 (8.9) |
| Southeast | 522 (77.1) |
| South | 64 (9.5) |
| Living in metropolitan area of State capitals | |
| Yes | 580 (85.7) |
| No | 97 (14.3) |
| Recruitment | |
| Hornet | 169 (24.9) |
| 511 (75.1) | |
Sexual abstinence was reported by 33.1% (225/680) during social distancing period; 20.9% (142/680) reported having sex only with steady partners and 46.0% had sex with casual partners (313/680). Among these, 55.3% (173/313) reported condomless receptive anal sex. Most of respondents maintained daily oral PrEP during social distancing (69.0%; 469/680).
Three quarters of study participants were aware of HIVST (488/680; 75.1%) but only 27.2% (n=185) had previously used it. Among these, the majority (163/185; 88.1%) felt comfortable using it. Willingness to use HIVST among those who never used HIVST was 79.0% (391/495). Only 32.1% (218/680) of all participants received an HIVST during social distancing period.
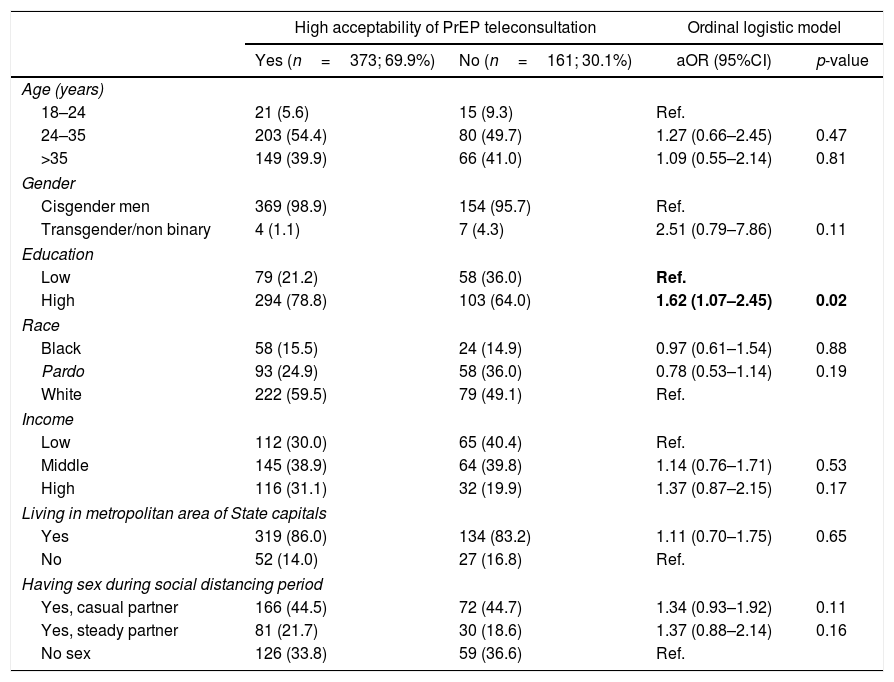
PrEP teleconsultation was experienced by 21.5% of PrEP users (146/680) and 89.0% (130/146) reported feeling satisfied with these new procedures. Among those not experiencing teleconsultation (n=534), high acceptability of teleconsultation was reported by 69.9% (373/534); 19.9% (106/534) informed being neutral, 9.2% (49/534) very uncomfortable or uncomfortable and 1.1% (6/534) reported not having a mobile phone. Main reasons for being uncomfortable with teleconsultation were: preference for face-to-face meeting with a physician (71.4%; 35/49), no privacy for teleconsulatation (20.4%, 10/49), unstable telephone/internet connection (4.1%; 2/49) and other reasons (4.1%; 2/49). In ordinal logistic model, having higher education was associated with high acceptability of PrEP teleconsultation [adjusted odds ratio (aOR):1.62; 95% confidence interval (CI):1.07–2.45] when adjusted by age, gender, race, income, living in metropolitan area of state capitals and having sex during social distancing period (Table 2).
Factors associated with high acceptability of PrEP teleconsultation. Brazil, 2020. n=534.
| High acceptability of PrEP teleconsultation | Ordinal logistic model | |||
|---|---|---|---|---|
| Yes (n=373; 69.9%) | No (n=161; 30.1%) | aOR (95%CI) | p-value | |
| Age (years) | ||||
| 18–24 | 21 (5.6) | 15 (9.3) | Ref. | |
| 24–35 | 203 (54.4) | 80 (49.7) | 1.27 (0.66–2.45) | 0.47 |
| >35 | 149 (39.9) | 66 (41.0) | 1.09 (0.55–2.14) | 0.81 |
| Gender | ||||
| Cisgender men | 369 (98.9) | 154 (95.7) | Ref. | |
| Transgender/non binary | 4 (1.1) | 7 (4.3) | 2.51 (0.79–7.86) | 0.11 |
| Education | ||||
| Low | 79 (21.2) | 58 (36.0) | Ref. | |
| High | 294 (78.8) | 103 (64.0) | 1.62 (1.07–2.45) | 0.02 |
| Race | ||||
| Black | 58 (15.5) | 24 (14.9) | 0.97 (0.61–1.54) | 0.88 |
| Pardo | 93 (24.9) | 58 (36.0) | 0.78 (0.53–1.14) | 0.19 |
| White | 222 (59.5) | 79 (49.1) | Ref. | |
| Income | ||||
| Low | 112 (30.0) | 65 (40.4) | Ref. | |
| Middle | 145 (38.9) | 64 (39.8) | 1.14 (0.76–1.71) | 0.53 |
| High | 116 (31.1) | 32 (19.9) | 1.37 (0.87–2.15) | 0.17 |
| Living in metropolitan area of State capitals | ||||
| Yes | 319 (86.0) | 134 (83.2) | 1.11 (0.70–1.75) | 0.65 |
| No | 52 (14.0) | 27 (16.8) | Ref. | |
| Having sex during social distancing period | ||||
| Yes, casual partner | 166 (44.5) | 72 (44.7) | 1.34 (0.93–1.92) | 0.11 |
| Yes, steady partner | 81 (21.7) | 30 (18.6) | 1.37 (0.88–2.14) | 0.16 |
| No sex | 126 (33.8) | 59 (36.6) | Ref. | |
Bold indicates statistical significance (p < .05).
The majority of respondents (593/680; 87.2%) reported preferring PrEP/HIVST home delivered instead of collecting them at the service. Most of participants reported recurring to physicians (65.3%; 444/680) to address concerns about PrEP or HIVST during social distancing period, followed by internet search (104/680; 15.3%), other health professionals (71/680; 10.4%), peer-educators (15/680; 2.2%), friends (6/680; 1.2%), and others (38/680; 5.6%).
Awareness and acceptability of HIVST among PrEP users was high and increased when comparing to previous online surveys conducted among Brazilian MSM even though our sample was restricted to PrEP users.6–9 Secondary analysis using data from these surveys indicate that Brazilian MSM willing to use HIVST were also willing to use PrEP.6,9 Moreover, a pilot study using an online platform for HIVST delivery was highly feasible and acceptable among MSM from Curitiba, Brazil.10 Our findings corroborate prior literature on indicating that HIVST could be incorporated to PrEP programs, including home delivery.
PrEP teleconsultation was highly evaluated by those previously experiencing it, and acceptability was high. These results indicate that PrEP teleconsultation could be maintained during COVID-19 pandemic, and continued thereafter as an option to increase retention to service and PrEP adherence. In addition, teleconsultation and HIVST/PrEP home delivery could increase access to MSM and TGNB individuals facing stigma, adherence concerns, and medical distrust. A pilot initiation program for PrEP delivery in the United States showed that teleconsultation increased access to young black MSM, as it eliminated barriers inherent in traditional clinic-based models.11 Conversely, results from our ordinal logistic model indicate that acceptability of PrEP teleconsultation was higher among those with higher education, indicating that face-to-face consultation may not be completely replaced. Brazil faces huge social and educational disparities that may become even more profound during and after the COVID-19 pandemic. Thus, we reinforce that PrEP services should train their staff considering the heterogeneity of our population, creating innovative and stigma-free services.
This study has limitations. First, web-based studies are not probabilistic sampling strategies, precluding the generalization of the findings to all Brazilian MSM and TGNB using PrEP. Moreover, our findings are based on those who have access to cellphones and who use GSN apps or social media. Nevertheless, recent data show that 79% of Brazilians have access to internet connection12 and 85% have mobile phones.13 All collected data were self-reported by participants and may be subject to bias, although individuals tend to be more honest through web-based surveys, reducing social desirability bias.14
In conclusion, telemedicine procedures for PrEP delivery including HIVST showed to be highly acceptable among PrEP users as well as PrEP/HIVST home delivery. These results point out that such technologies could be an option to be implemented by Public Health Services in Brazil to avoid PrEP access shortage during the COVID-19 pandemic and thereafter as an option to increase retention to service and PrEP adherence. Conversely, teleconsultation may not substitute face-to-face visits with a physician among MSM and TGNB with lower education or who do not have a private space for teleconsulation.
This project was made possible, thanks to Unitaid's funding and support. Unitaid accelerates access to innovative health products and lays the foundations for their scale-up by countries and partners. Unitaid is a hosted partnership of the WHO. TST acknowledges funding from the National Council of Technological (CNPq, #28/2018). BG acknowledges funding from the National Council of Technological and Scientific Development and the Research Funding Agency of the State of Rio de Janeiro (Programa Cientista do Nosso Estado; Edital N.° 03/2018).