A 37-year-old man with AIDS presented with altered mental status four weeks after stopping his medications for Mycobacterium avium-intracellulare (MAI). He had low CD4 cell count and severe hypercalcemia. Bone marrow biopsy revealed bone marrow infiltration by granulomas positive for acid-fast bacilli and cultures grew MAI. His hypercalcemia continued to worsen with the initiation of MAI therapy but we were able to treat it successfully with pamidronate and calcitonin.
Hypercalcemia above 14mg/dL is often attributed to malignancy, but patients with HIV warrant further investigation into opportunistic infections such as Mycobacterium avium-intracellulare (MAI). Although previous reports discussed the association between MAI and hypercalcemia, the onset and clinical course of hypercalcemia is not known. We present a case of hypercalcemia with MAI that worsened with the initiation of anti-mycobacterial therapy and a review of the literature of the onset of hypercalcemia in relation with MAI diagnosis and explore potential triggers.
Case presentationA 37-year-old man with AIDS on highly active antiretroviral therapy (HAART) and chronic therapy for Mycobacterium avium-intracellulare (MAI) presented with altered mental status four weeks after stopping his medications. His family reported progressive confusion and weight loss. He did not have any recent history of sick contacts, travel, animal exposure, nor illicit drug use. On physical examination, his temperature was 38.1°C, blood pressure 130/50, heart rate 118, respiratory rate 16 with O2 saturation 95% on room temperature. He was somnolent and cachectic.
Laboratory work-up showed normocytic anemia with a hemoglobin of 8g/dL, leukopenia 0.9/μL thrombocytopenia 60/μL, CD4 count 7/mm3, creatinine 1.4mg/dL, corrected calcium 12mg/dL (ref 8.4–10.4mg/dL), ionized calcium 1.6mmol/L (ref 1.15–1.27mmol/L), phosphorus 2mg/dL (ref 2.3–5.6), and albumin 1.8g/dL (ref 3.5–5 d/dL). His 25-hydroxycalciferol level was low 9ng/ml (ref 30–100), PTH was suppressed 6pg/mL (ref 11–80pg/mL) and PTH-related peptide was undetectable.
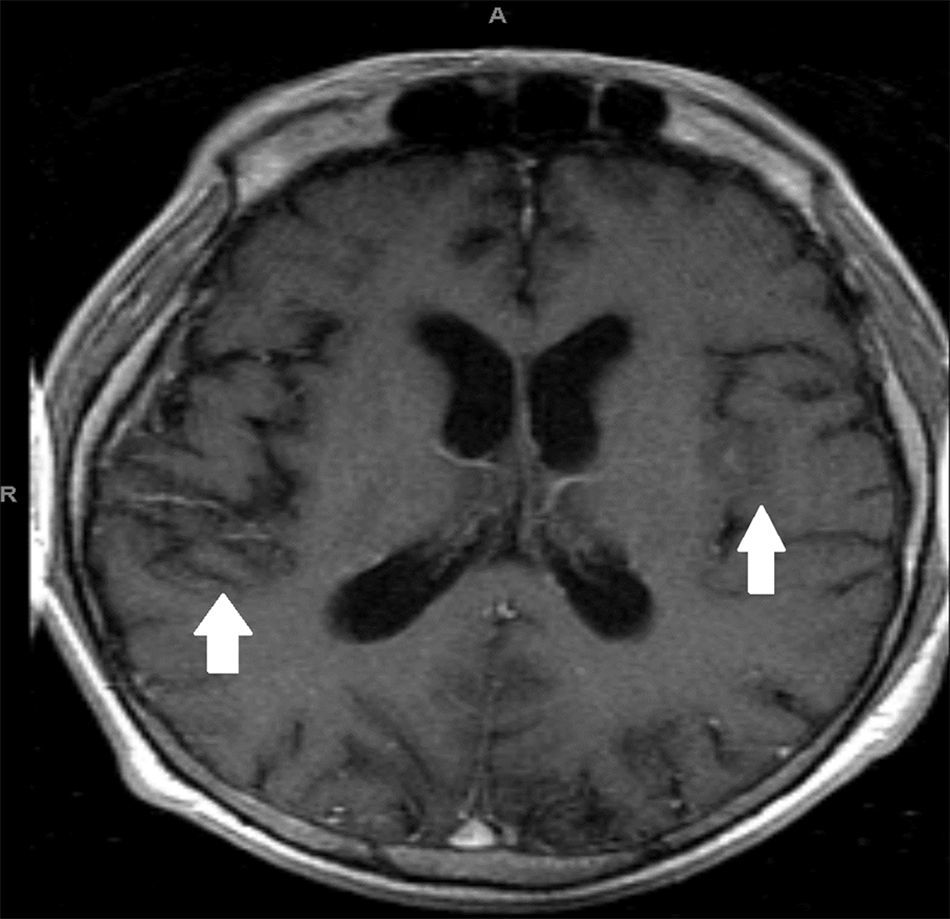
Magnetic resonance imaging (MRI) of the brain showed scattered areas of abnormal parenchymal signal intensity likely from tuberculous meningoencephalitis (Fig. 1). Computed tomography (CT) of the chest, abdomen and pelvis revealed necrotic mesenteric lymph nodes and splenomegaly.
Serum protein electrophoresis and skeletal survey were negative. Bone marrow biopsy revealed bone marrow infiltration by granulomas positive for acid-fast bacilli and cultures grew MAI. His hypercalcemia was treated with intravenous fluids and he was started on clarithromycin, rifampin and ethambutol for MAI. His serum calcium trended up from 12mg/dL on admission to 14mg/dL by hospital day six so he was started on calcitonin and pamidronate with normalization of serum calcium and improvement in the patient's mental status within 24h.
The patient's calcium levels remained within normal range but his clinical condition deteriorated as he developed severe sepsis, disseminated intravascular coagulation (DIC), and respiratory failure requiring endotracheal intubation and mechanical ventilation secondary to hospital-acquired pneumonia. A follow-up brain CT showed worsening in the size of the lesions secondary to hemorrhage in the setting of DIC. After extubation, he was found to have major cognitive deficits with being oriented only to self. At the time of discharge, his hypercalcemia, sepsis, and DIC have all resolved, however, his cognitive impairment persisted.
DiscussionBetween 1981 and 1987, 5.5% of AIDS cases reported to the Centers for Disease Control (CDC) had non-tuberculous mycobacterial infection, with MAI being the culprit in 96% of cases.1 The incidence of opportunistic infections decreased with the advent of HAART and a more recent study from 1994 to 2007 suggested that the rate of Mycobacterium avium complex infection is 2.5 per 1000 person-years in individuals with AIDS.2 The mechanism of hypercalcemia in granulomatous disease is thought to be related to vitamin D dysregulation but this does not always correlate with vitamin D metabolite levels.3
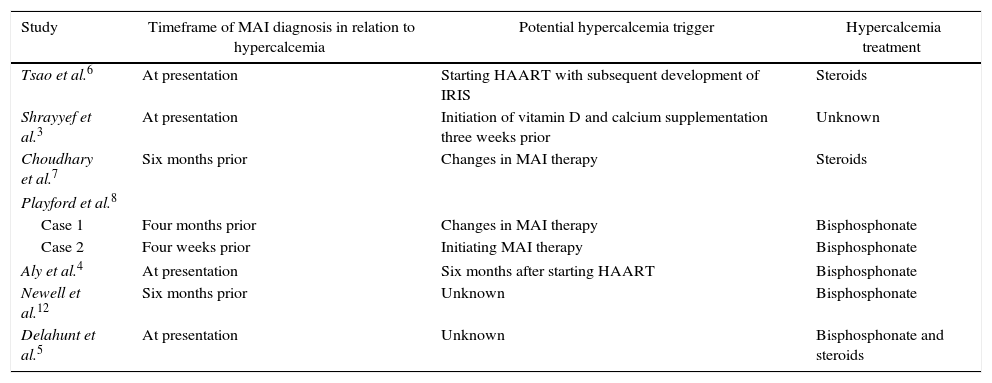
A review of the literature yielded only eight cases of MAI-associated hypercalcemia (Table 1). Three of these cases presented with hypercalcemia at the time of diagnosis of MAI3–5; Tsao et al. described hypercalcemia presenting as part of the spectrum of immune reconstitution inflammatory syndrome (IRIS) against MAI.6 Four reports described hypercalcemia in patients who were undergoing treatment for MAI, soon after starting or changing antimicrobial therapy.7,8 One patient was diagnosed three weeks after initiating treatment for vitamin D deficiency.3 Our patient presented with hypercalcemia at the time of diagnosis, which worsened within days of restarting MAI therapy. In all these cases, no association between the development of hypercalcemia and organ involvement or choice of anti-MAI therapy was observed.
Previous reports of MAI-associated hypercalcemia.
| Study | Timeframe of MAI diagnosis in relation to hypercalcemia | Potential hypercalcemia trigger | Hypercalcemia treatment |
|---|---|---|---|
| Tsao et al.6 | At presentation | Starting HAART with subsequent development of IRIS | Steroids |
| Shrayyef et al.3 | At presentation | Initiation of vitamin D and calcium supplementation three weeks prior | Unknown |
| Choudhary et al.7 | Six months prior | Changes in MAI therapy | Steroids |
| Playford et al.8 | |||
| Case 1 | Four months prior | Changes in MAI therapy | Bisphosphonate |
| Case 2 | Four weeks prior | Initiating MAI therapy | Bisphosphonate |
| Aly et al.4 | At presentation | Six months after starting HAART | Bisphosphonate |
| Newell et al.12 | Six months prior | Unknown | Bisphosphonate |
| Delahunt et al.5 | At presentation | Unknown | Bisphosphonate and steroids |
The suggested treatment of hypercalcemia in granulomatous disease is steroids which are thought to downregulate calcitriol synthesis by macrophages.9 Given our concern for lymphoma as part of our differential diagnosis, we elected not to use steroids as they cause histopathological alterations on biopsy and delay in making the diagnosis.10 Our patient was treated with calcitonin and pamidronate. Bisphosphonates can be safely used for the treatment of osteoporosis in HIV patients,11 and Shrayef et al. previously used pamidronate successfully for the treatment of hypercalcemia with MAI.3
It is unknown if there is a genetic predisposition for some individuals with AIDS who are infected with MAI to develop hypercalcemia. Our review of the literature suggests that certain triggers may be implicated such as immune reconstitution after starting HAART, improved host defence mechanism after initiating or incurring change in anti-MAI therapy or dysregulated response to vitamin D treatment.
ConclusionsWhile hypercalcemia is a known complication of granulomatous disease, clinicians should be aware of the variability in presentation of hypercalcemia with MAI, whether as the first manifestation or a late presenter in the disease course. As we showed in this case, hypercalcemia may worsen within days of initiating anti-mycobacterial therapy. We suggest careful monitoring of serum calcium levels upon diagnosis of MAI infection and after initiation of mycobacterial therapy or vitamin D supplementation. Pamidronate and calcitonin are acceptable treatment alternatives to steroids for hypercalemia treatment.
Conflicts of interestThe authors declare no conflicts of interest.