The recognition of the causal association between Zika virus (ZIKV) infection during pregnancy and congenital abnormalities including microcephaly underlines the importance of preventing this disease in pregnant women (PW) and women of childbearing age (WCA). Although Brazil and other Latin American countries reported a significant reduction in the number of ZIKV infections in recent years, epidemic waves can recur in settings with previous outbreaks as conditions for transmission remain optimal and susceptible populations are continuously replenished.
MethodsIn this cross-sectional study, we enrolled 64 PW and 260 non-pregnant WCA attending routine medical appointments in two primary care units in Sao Paulo, Brazil, and assessed knowledge and attitudes about ZIKV infection and prevention.
ResultsMost women reported knowing that ZIKV is transmitted through the bite of Aedes mosquitos, and most knew that acute symptoms are similar to those seen in Dengue infection. Furthermore, most participants correctly described that ZIKV infection during pregnancy may cause detrimental outcomes for the newborn. However, most ignored that ZIKV infection can be asymptomatic, and only 15% knew about the risk of ZIKV sexual transmission. We found no statistically significant differences between PW and WCA regarding knowledge about ZIKV sexual transmission. Knowledge about ZIKV sexual transmission was significantly associated with education; among participants with ≤12 schooling years, only 9.0% (95%CI 3.4-18.5%) correctly answered that ZIKV can be sexually transmitted, compared to 12.9% (95%CI 8.2-18.8%) among participants with 12-14 schooling years, and to 24.4% (95%CI 15.9-34.9%) of participants with ≥15 schooling years (p = 0.015). Education remained independently associated with knowledge about sexual transmission of ZIKV in a multivariate logistic regression model adjusted for age, race and pregnancy status (p = 0.022).
ConclusionOur findings underscore the urgent need of educational and family planning programs that may help prevent detrimental outcomes of ZIKV infection in an endemic area of Brazil.
Since 2016, Brazilian and international scientific groups have been dedicating intense efforts to understand Zika virus (ZIKV) infection.1 This interest has been raised following a massive epidemic wave in Latin America and the detection of a significant increase in the number of newborns with microcephaly and other congenital malformations causally associated with ZIKV infection during pregnancy. Brazil was the first country to identify an increase in microcephaly cases, and the causal association with ZIKV infection was supported by studies showing that the virus was present in damaged fetal neural tissues; moreover, ZIKV was shown to have a neurotoxic effect in both in vitro and animal models.2-4
As seen with other viruses belonging to the Flavivirus family, ZIKV is transmitted through the bite of Aedes mosquitos, and Aedes aegypti seems to be the main vector for the disease in the Americas.5 Blood transfusions can also be a potential source of ZIKV infection.6,7 Sexual intercourse is another non-vectorial mode of ZIKV transmission, particularly from a male infected partner8,9; viral RNA has been shown to persist in the semen of a few patients for several months after symptoms onset, with potential transmissibility lasting 6-7 weeks.10
The first Brazilian cases of ZIKV infection were detected in 2015 in the Northeast region of the country, with subsequent expansion to states in the Central-West and Southeast regions.2 In the state of Sao Paulo, ZIKV outbreaks were more significant in rural and countryside cities and in coastal cities.11 After the peak case-detection in 2016, Brazil and other Latin American countries reported an important reduction in the number of ZIKV infections.12 However, new epidemic waves can recur in settings with previous outbreaks as conditions for transmission remain optimal and susceptible populations are continuously replenished. Furthermore, the World Health Organization highlighted in a recent report that approximately 61 countries with no reports of ZIKV occurrence have local conditions for the spread of the virus, with naturally occurring competent vectors, ideal climate settings and vulnerable populations. This report also discusses the importance of providing family planning strategies and travel orientation in countries with ZIKV occurrence.13 Since ZIKV still lacks effective antiviral treatments or vaccines, health services and public health institutions should be prepared to respond to new disease outbreaks.14 One essential way of being prepared is supporting vulnerable populations such as women of childbearing age (WCA) with knowledge about the disease and how to prevent it.15
In this study we enrolled pregnant women (PW) and non-pregnant WCA in two primary care units in Sao Paulo, Brazil, and assessed knowledge and attitudes about ZIKV infection and prevention. We also explored if the recent ZIKV outbreak had an impact on family planning issues in this population.
MethodsStudy design, population and settingIn this cross-sectional study, we enrolled PW and non-pregnant WCA attending routine medical appointments at two primary care units, both in central areas of Sao Paulo city, Brazil. Consenting women aged 18-45 years old living in Sao Paulo city were considered eligible; we excluded women with current or past ZIKV infection and those who had infertility due to any cause.
Study proceduresAfter obtaining informed consent for participation from each woman, a trained study investigator administered the study questionnaire that included questions on knowledge about ZIKV infection, knowledge and attitudes towards prevention strategies, and the impact of the recent ZIKV outbreak on family planning. Pregnancy status at the time of interview was self-reported. Responses were registered in a standardized electronic form using REDCap platform.16
Ethical aspectsAll participants provided informed consent upon inclusion in the study. We collected no participant-identifiable information, and all study forms were kept in locked cabinets or password-secured electronic folders in accordance with Good Clinical Practice recommendations. The study has been approved by the Ethics committee at University of Sao Paulo Medical School (approval reference number 2.358.114) as well as local ethics committees at each primary care unit. As a benefit from participation, the study investigator offered to review all questionnaire answers and clarify any remaining uncertainties; a printed booklet produced by the Brazilian Ministry of Health containing information on ZIKV was also offered to all participants at the end of study participation.17
Statistical analysisData was analyzed using descriptive statistics. Comparisons between PW and WCA were preformed using chi-squared tests or Fisher's exact test for categorical variables, and t-tests or Wilcoxon Rank-sum tests for numerical variables, as appropriate. A multivariate logistic regression model was used to explore independent predictors of knowledge about ZIKV sexual transmission. We used Stata 15.1 (StataCorp. College Station, TX: StataCorp LP), with a two-tailed significance level of 0.05 for all analyses.
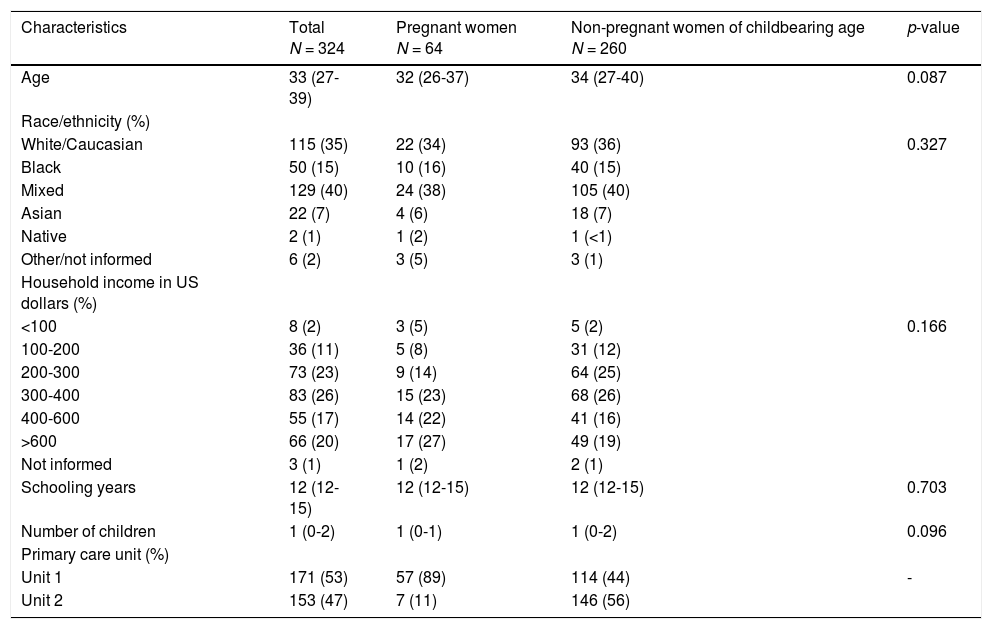
ResultsBetween December 2017 and July 2018, 409 PW and WCA were invited to participate in the study; of those, 85 were excluded (21 refused or withdrew participation; 4 lived in other cities; 37 were older than 45 or younger then 18 years old and 23 were excluded due to infertility related to past/current ZIKV infection). Among 324 women included in the study, 64 (20%) were pregnant. Demographic characteristics of study participants, overall and according to pregnancy status, are presented in Table 1. PW and non-pregnant WCA were similar regarding age, race/ethnicity, income, and education.
Demographic characteristics of study participants, overall and according to pregnancy status.
Numeric variables are presented as medians and interquartile ranges
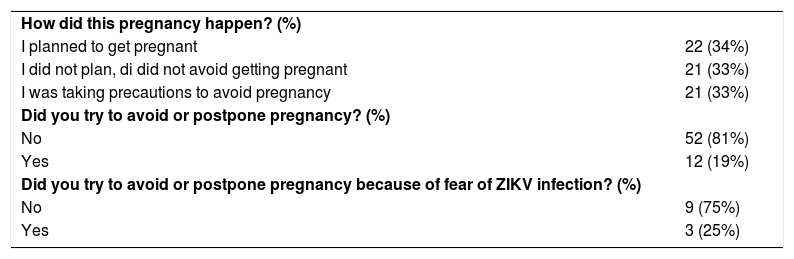
Out of 64 PW enrolled in the study, 22 (34%) reported they had planned to get pregnant; 21 (33%) said they were neither planning nor avoiding pregnancy; and 21 (33%) said they got pregnant despite taking precautions to avoid pregnancy. Only three out of 12 women who reported trying to postpone pregnancy attributed it to fear of ZIKV infection (Table 2).
Family planning aspects among 64 pregnant women enrolled in the study.
ZIKV: Zika virus
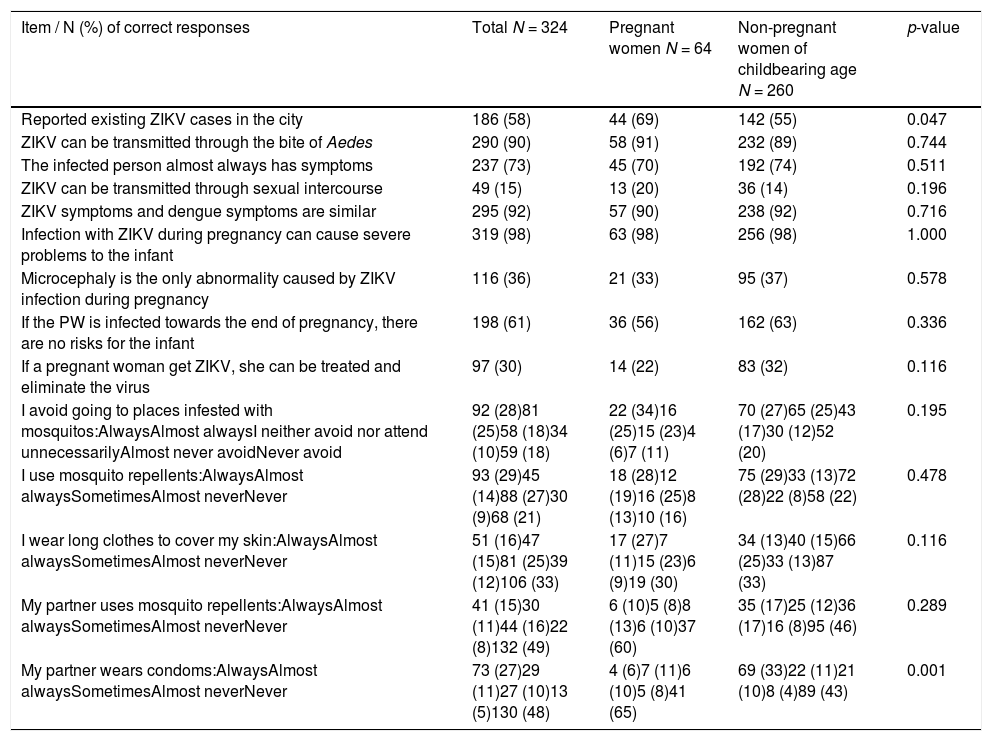
Table 3 presents participants’ knowledge and attitudes towards ZIKV infection. Most women reported knowing that ZIKV is transmitted through the bite of Aedes mosquitos, and most knew that acute symptoms are similar to those seen in Dengue infection. Furthermore, most participants correctly described that ZIKV infection during pregnancy may cause detrimental outcomes for the newborn. However, most ignored that ZIKV infection can be asymptomatic, and only 49 (15%) knew about the risk of ZIKV sexual transmission. Surprisingly, we found no statistically significant differences between PW and WCA in the knowledge and attitudes towards ZIKV infection, except for higher knowledge about ZIKV cases in the city (p = 0.047) and lower condom use by the sexual partner (p = 0.001) among PW.
Knowledge and attitudes concerning ZIKV infection among study participants, overall and according to pregnancy status.
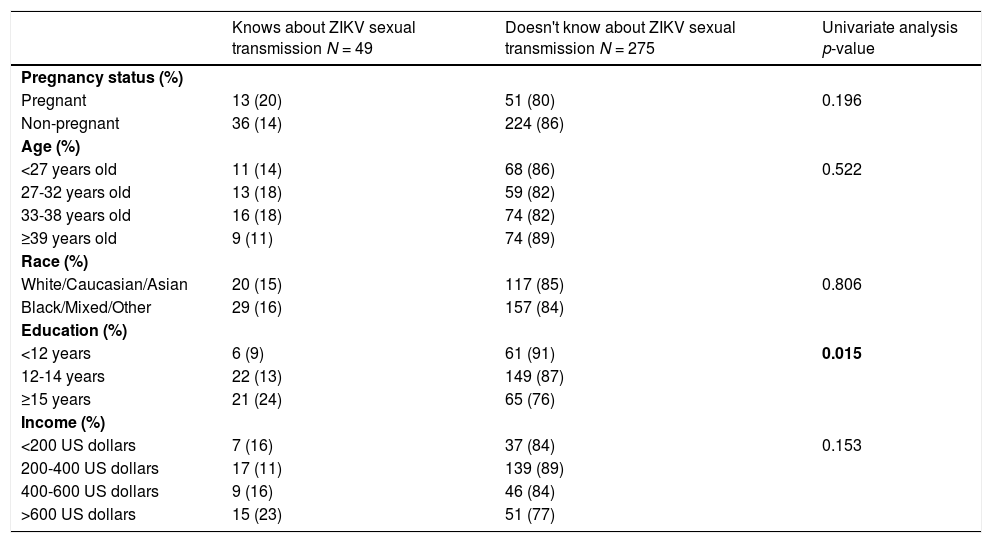
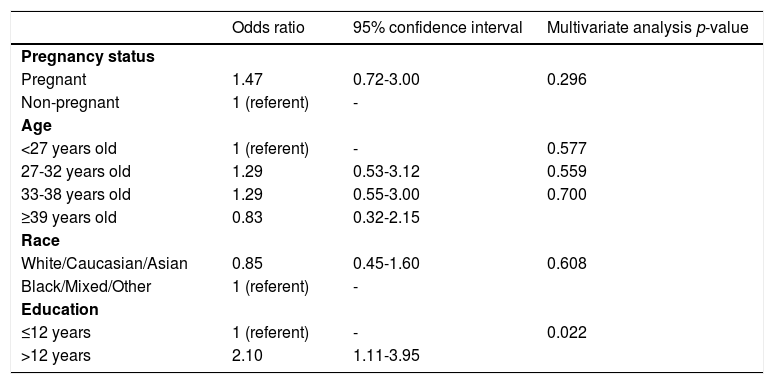
Given the strikingly low percentage of knowledge about ZIKV sexual transmission among women of childbearing age regardless of pregnancy status, we further explored if age category, race, education and income were associated with this finding. We found a statistically significant association between education and knowledge about ZIKV sexual transmission; among participants with ≤12 schooling years, only 9% (95% CI 3-19%) correctly answered that ZIKV can be sexually transmitted; this percentage was 13% (95% CI 8-19%) among participants with 12-14 schooling years, and 24% (95% CI 16-35%) among participants with ≥15 schooling years (p = 0.015; Table 4). Age category, race, and income were not significantly associated with knowledge about ZIKV sexual transmission in univariate analysis (Table 4). In a multivariate logistic regression model adjusted for age, race and pregnancy status, education remained independently associated with knowledge about sexual transmission of ZIKV; participants with >12 schooling years had 2.10 times the odds of reporting this knowledge compared to those with ≤12 schooling years (95% CI 1.11-3.95; p = 0.022; Table 5).
Factors associated with knowledge about ZIKV sexual transmission in univariate analysis.
Factors associated with knowledge about ZIKV sexual transmission in multivariate analysis.
In this cross-sectional study, we addressed knowledge and attitudes about ZIKV infection among PW and non-pregnant WCA. We showed that the knowledge about transmission by mosquitos and the potential to cause congenital malformations when infection occurs during pregnancy was generally high. However, the knowledge about sexual transmission was very low among both PW and non-pregnant WCA. These findings are alarming, particularly in the context of the recent outbreak of ZIKV in Brazil, with ample repercussion in mass communication vehicles. Furthermore, during study design our group had initially hypothesized that PW would have higher levels of knowledge and better prevention attitudes compared to non-pregnant WCA, given multiple opportunities of learning during antenatal care consultations.18 We were surprised to see that PW and WCA had similar knowledge and prevention attitudes, except for the knowledge about ZIKV cases in the city and use of condoms by the sexual partner. This was expected, since contraception is certainly one of the main reasons for condom use among non-pregnant couples and will be less frequently adopted if the woman is already pregnant. However, it also emphasizes that prevention of ZIKV sexual transmission to PW may face significant challenges in endemic countries. Knowledge about ZIKV sexual transmission was reported by only 15% of participants in our study and was similarly low among PW and non-pregnant WCA. Education was significantly associated with knowledge about ZIKV sexual transmission in both univariate and multivariate analysis. Finally, we also found that a very small number of PW reported they had postponed pregnancy due to the ZIKV epidemic in our setting.
A few prior studies have explored knowledge, attitudes and practices of WCA towards ZIKV infection. Knowledge about ZIKV sexual transmission was assessed among PW and women attending antenatal care clinics, and was shown to be lacking in the majority of participants in a study conducted in the USA19; similarly, 74% of respondents in a study conducted in Trinidad and Tobago20 and 63% in a study conducted in Greece21 ignored that ZIKV could be transmitted through sexual intercourse. In a survey including male and female participants in the USA, only 27% identified abstinence or using condoms during intercourse as precautions for ZIKV infection in PW traveling to endemic areas.18 In a study published by Borges et al., who interviewed 526 women aged 18 to 49 years old in the Northeast of Brazil, awareness about the congenital syndrome associated with ZIKV infection during pregnancy was high, but only 50% of participants knew about the risk of sexual transmission. The higher proportion of women with knowledge about ZIKV sexual transmission compared with our sample may be partially explained by the fact that the Northeast of the country was the epicenter of the disease, and the study was conducted few months after the peak of ZIKV epidemic.22 However, this proportion is still not ideal, and further studies should be conducted to assess if this knowledge is retained years after the peak of the epidemic. In accordance with our findings, education and other social determinants have been associated with knowledge and attitudes about ZIKV in previous publications,21,23 suggesting that WCA in more vulnerable settings should be prioritized in public health policies and prevention strategies. Although vector transmission is undoubtedly the main route of infection for ZIKV, spread through sexual contact also contributes to the transmission chain24 and should be prevented particularly among pregnant women. Recommendations for abstinence and safer sex in high ZIKV transmission areas have been issued by Brazilian25 as well as international organizations.26,27
Our study has a few limitations. We restricted selection of participants to a convenience sample in two primary care units, both located in central, more affluent areas of Sao Paulo city. Therefore, our study sample comprised women with higher socioeconomic status than the average population in our setting. Women with no access to healthcare were not available for inclusion in our study. These limitations emphasize that the overall knowledge about ZIKV is probably even lower, reinforcing the urgent need for educational actions that may help prevent ZIKV detrimental outcomes.
Our study included PW and non-pregnant WCA between December 2017 and July 2018, over a year after the peak detection of ZIKV cases in the country. The improvements in epidemiological figures may had decreased the pressure for public health interventions supporting ZIKV prevention, particularly concerning PW and non-pregnant WCA. However, Brazil has optimal vector and climate conditions for a recurring outbreak, and actions supporting education and self-care should be intensified. Other countries with potential risk of future ZIKV outbreaks should also implement such strategies in order to avoid subsequent preventable outbreaks of congenital abnormalities.13