Mucormycosis or black fungus infection is a less common disease but highly fatal infection, infecting the immunocompromised individuals. The site of predilection of the fungus is found to be lungs and brain in addition to its sequestration in sinusoidal spaces. Presently with the ongoing COVID 19 pandemic, the prevalence of this infection is found to be high in the Indian population. The fungus establishes itself by affecting the compromised immune system of an individual and thereby making the individual susceptible to other diseases/infection. The reasons attributed to the sudden upsurge are steroidal therapeutics abuse, tocilizumab therapy and diabetes mellitus.To avert the cytokine storm, the medical health workers are necessitated to include steroid drugs in COVID 19 treatment protocol however inclusion of these drugs in patients who do essentially require steroids can have their immune system debilitated and permit the invasion of this fungus. According to International Diabetes Federation (IDF), 77 million Indians are known to be diabetic, cautioning the physicians to be vigilante of the impending black fungus infection in the event of COVID19 affliction in such individuals. There is causal relationship between anti-hyperglycemic drugs and weakened immune system and opportunity for the fungus invasion. This review attempts to explain the inter-relatedness of COVID19 infection, its treatment and eventual black fungus infection risk.
Human Corona Viruses (HCoV) are the type of viruses that cause infections mainly in gastrointestinal and respiratory systems. The first discovered human corona viruses were HCoV‐229E and HCoV‐OC43 from the nasal cavities of human patients who were suffering from common cold, in 1960s.1 Other human coronaviruses include SARS‐CoV (in 2003), HCoV NL63 (in 2004), HKU1 (in 2005), MERS‐CoV (in 2012), and the latest one SARS‐CoV‐2 (in 2019) resulting in coronavirus disease (COVID-19).2 Globally, there have been 173,674,509 confirmed cases of COVID-19, including 3,744,408 deaths reported as on June 09, 2021. As of June 10, 2021 there were 1,167,952 active cases in India while 27,655,493 people had recovered from the disease.3 While the national COVID-19 recovery rate dropped to 94.77%, the case fatality rate was down to 1.23% according to the MoHFW.
In the year 2021, multiple challenges have been faced while treating Covid-19 infections, including Mucormycosis (black fungus). Mucormycosis is an opportunistic fungal infection that belongs to the zygomycete family and is ubiquitous in the environment. The major route of infection is via inhalations of spores of Rhizopus oryzae a common cause of rhino-orbital-cerebral form of infections, which spread to the paranasal sinuses and lungs. These moulds are generally found in soil, plants, manure, decaying fruits and vegetables. Mucormycosis is a rare but severe and eventually fatal fungal infection that usually affects patients with altered immunity. In general, these fungi are non-pathogenic in immune competent patients but in the case of patients immune compromised by either steroids or any other co-morbidities like diabetes, solid cancers, malignant and hematologic disorders may become life-threatening. Other risk factors including organ transplantation and high levels of iron in serum may increase the risk of black fungus mortality.4
In covid-19 patients, especially those who need oxygen support, the immune system may become weak due to inflammatory storm or usage of steroids. This may pave the way for opportunistic infections including mucormycosis. The common symptoms of this infection include discoloration of the nose and tongue, redness in the eyes, blurred vision, difficulty in breathing, chest pain, cough, fever, headache, black lesion inside the mouth, and vomiting. Diagnosis is usually made by clinical suspicion and histopathological examination. As per recent reports in India, the number of people dying from black fungus is steadily increasing and experts are referring to it as 'pandemic within COVID-19 pandemic'.
In India more cases were noticed in the second wave of Covid-19 than in the first wave with increased mortality rate. The major complications faced with mucormycosis in the second wave were reduced oxygen levels, difficulty in breath and other respiratory tract associated problems like pneumonia and Acute Respiratory Distress Syndrome. At present in India, the patient who underwent long oxygen supportive therapy are more prone to be infected with mucormycosis.
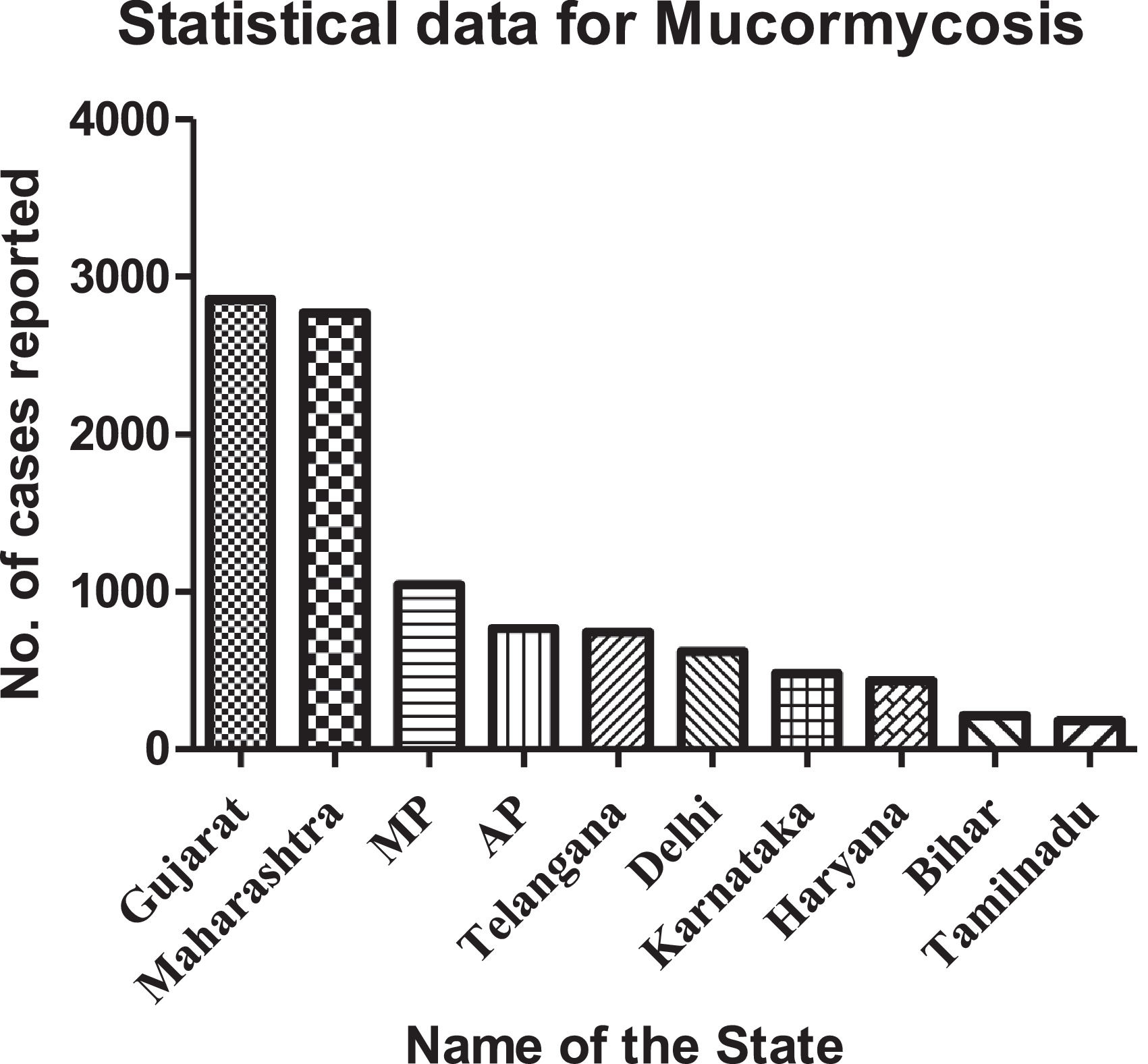
During the second wave of Covid-19 pandemic the very first case of mucormycosis or black fungus infection was reported at Gujarat in a 15-year-old boy who recovered successfully from Covid-19 and got discharged. Later on the cases were reported in more than 18 states of India.5 Auraiya district in Uttar Pradesh has reported the first death caused by mucormycosis. The highest death rate was recorded in Rajasthan. India has recorded more than 12,000 cases of mucormycosis, and over 300 deaths were recorded in the past few months.5 Most of the cases are reported from Gujarat, Maharashtra, Rajasthan, Karnataka, Andhra Pradesh, Haryana and Telangana as per the latest government reoprts.6 Ten states in India reported large number of mucormycosis cases; those are graphically represented in Fig. 1.
According to literature, it is clear that animals/humans with decreased number of phagocytes or having impaired phagocytic function are at higher risk of black fungus infection. Therefore, patients with severe neutropenia are at increased risk of developing the infection.7 In contrast, as HIV/AIDS patients do not seem to be at increased risk for developing black fungus infection, it suggests that neutrophils play a key role in the inhibition of fungal spore proliferation, but not necessarily T lymphocytes. In the condition of diabetic ketoacidosis, phagocytes are dysfunctional and have impaired chemotaxis and defective intracellular killing by both oxidative and non-oxidative mechanisms. The pulmonary alveolar macrophages harvested from lungs of immunocompetent mice are able to inhibit the germination of fungal spores. But the same pulmonary alveolar macrophages isolated from immunosuppressed mice are unable to inhibit the fungal spore germination in in-vitro and in-vivo experiments.8 The mechanisms by which phagocytes turn dysfunctional by diabetes mellitus and corticosteroids need to be determined.8 One of the essential elements for cell growth and development is iron. Therefore, pathogens use some processes for obtaining iron from the host. Transferrin, ferritin, and lactoferrin are the carrier proteins to which the excess iron is bound in hosts and avoids toxic effect of free iron by reducing the excess free iron levels in serum. This is the unique host defense mechanism against bacteria, virus and even fungus especially mucorales because they cannot grow in normal serum unless iron is added exogenously.
To treat severe mucormycosis infection, the patient should be strictly monitored by a team of health specialists including microbiologists, internal medicine specialists, neurologists, ENT specialists, ophthalmologists, dentists, surgeons, etc. In India the first line drug being used for treating mucormycosis is liposomal amphotericin-B and approximately 20 vials of this antifungal injection may be required to treat a single infected person. In India, the current price for each vial is around Rs.5000-6000, according to reports. The second line drug is Posaconazole. Doctors are warning that all these medicines should only be taken under strict medical supervision.
In few cases surgical removal of infected tissues may be required. At the hospital MGM Health care located at Chennai, Tamilnadu a person diagnosed with black fungus in the right naso-orbital region involving sinuses was saved by a surgery performed with the help of multiple angled high-definition endoscopes. Of a total of 700 cases reported in Jaipur over 200 patients underwent jaw removal surgery.
Abuse of steroidsWHO strongly recommends corticosteroids to be given orally or intravenously for the treatment of patients with severe and critical COVID-19 once daily for 7-10 days and advised to not to be given for the patients with non-severe COVID-19. Steroids are an admirable treatment, if used judiciously and in the appropriate condition. Experts believe that the improper use of corticosteroids (i.e. dexamethasone, hydrocortisone or prednisone) in Covid-19 patients is the primary reason for black fungus infection. Even though steroids are very good agents to reduce many types of inflammations like rheumatoid arthritis and pulmonary diseases such as asthma and chronic obstructive pulmonary disease, the chronic usage or over dose of steroids will suppress the body's immune response and make the patient more prone to other infections like mucormycosis or black fungus infection in India.
Improper usage of oxygen cylindersAnother probable reason for the surge in post-COVID mucormycosis is the unhygienic delivery of oxygen or low-quality tubing system to these patients at the hospital ICUs, the oxygen cylinders with unclean masks or using contaminated/tap water in humidifiers and prolonged usage of same mask for more than two patients.9
Worsening of diabetesDiabetes mellitus is a chronic life treating metabolic disorder and is the 6th leading cause of death in India. The incidence of diabetes in India has increased dramatically over the past 40 years. Around 77 million people have been diagnosed with diabetes in India, over 90% type-2 diabetes mellitus (T2DM). T2DM is caused by insufficient insulin secretion by pancreatic β-cells and/or the inability of insulin-sensitive tissues to respond appropriately to insulin. T2DM may increase risk of developing black fungus infection in post-COVID-19 patients with more than 8 in 10 black fungus cases diagnosed in patients with diabetes. Diabetics usually have lower immune responsiveness which is further impaired by hypoglycemic agents. Extensive care should be taken in Covid-19 patients with the history of diabetes mellitus.
Tocilizumab therapyCOVID-19 infection induces a dose-dependent production of IL-6 pro-inflammatory cytokine from bronchial epithelial cells. To control the levels of IL-6 in these particular patients, tocilizumab, an FDA approved drug, has been prescribed along with dexamethasone. Tocilizumab is a recombinant humanized anti-IL-6 receptor monoclonal antibody. Chronic usage of this therapy to control inflamation triggered by severe acute respiratory syndrome-associated corona virus (SARS-CoV) weakens the patient's immune response. In this way tocilizumab increases the risk of mucormycosis in post-COVID-19 patients.
ConclusionCOVID-19 disease is shaking the world as did the Spanish flu in 1918 (caused by the H1N1 influenza-A virus). It had very fast dissemination over the globe, but with an appreciable recovery rate. In 70–80% of COVID-19 patients the severity of the infection is mild-moderate and recover without any other complications. However, in the remaining patients the infection is rather severe and the respiratory system may collapse. Those patients require external oxygen supply, corticosteroid administration and regular monitoring of blood glucose levels. The improper use or chronic usage of this treatment measures may lead to the development of other infections like black fungus infection and even white and yellow fungal infections.
Nil.