This study aimed to analyze the pattern of surgical chemoprophylaxis, surgical site infection rate, and to check rationality of surgical chemoprophylaxis based on Kunin's criteria.
Materials and methodsA prospective, observational study was performed on patients undergoing surgery, in a tertiary care teaching hospital. Data were collected in a pro-forma which included the patients’ details, prescriptions from date of admission to discharge or any other outcome and operative notes. Surgical site infection as defined by Centre for Disease Control criteria was recorded. Rationality was assessed based on Kunin's criteria.
ResultsTotal 220 patients were enrolled over a period of one year. Mean hospital stay was 8.67±5.17 days. A total of 2294 drugs were prescribed out of which 840 (36.61%) were antimicrobials. Mean duration for pre-operative intravenous antimicrobial therapy was 0.75±0.45 day and for post-operative intravenous antimicrobial therapy was 3.33±2.24 days while post-operative oral antimicrobial therapy was 4.58±3.34 days. Third generation cephalosporins were prescribed most frequently 64.74% and 64.40% pre-operatively and post-operatively respectively. Antimicrobial prescribing was inappropriate in 52.28%. Total of 19 patients developed surgical site infection. Surgical site infection rate was significantly higher (13.04%) in patients receiving inappropriate chemoprophylaxis (p<0.01). Surgical site infection adds 9.98 days of hospital stay (p<0.0001) and 3.57 extra drugs (p<0.0001) compared to group without surgical site infection.
ConclusionInappropriate use of antimicrobials is highly prevalent in surgical chemoprophylaxis leading to higher surgical site infection rate. Adoption of international standard and formulation of locally feasible guidelines can help overcome this situation.
As Sir Alexander Fleming predicted in his Nobel Lecture, “Antimicrobials, since their introduction have been pivotal in the prevention and treatment of infections. However, the increasing use of antimicrobials has led to a situation of appropriate and inappropriate use.”1A surgical site infection (SSI)2 is an infection that occurs after surgery in the part of the body where the surgery took place. Surgical site infections remain among the main causes of post-operative morbidity, prolonging hospitalization and increasing the cost of medical treatment in surgical units.3–4 Antimicrobials play an important role in preventing and treating surgical site infections. Surgical chemoprophylaxis is an important measure before any surgery to prevent SSI. Various guidelines5–8 are available for the use of antimicrobials for surgical chemoprophylaxis. However it is observed that they are not always followed.9,10 This has led to a worldwide emergence of antimicrobial resistance, a major public health problem and has significant impact on treatment and outcomes. To produce the desired effect, antimicrobials have to be safe, efficacious and have to be used rationally. Several studies have evaluated pattern of use of antimicrobials as surgical chemoprophylaxis, but there are very limited studies in recent years on evaluation of rationality. Kunin's criteria are rationality based evaluation of use of antimicrobials. This methodology is based on local prescribing patterns and allows for individual evaluation of each prescription as opposed to developing general criteria/categories of infections and appropriate antimicrobial use to evaluate the quality of prescribing by audits. In the past, the classification was mainly based on the authority of infectious diseases specialists who performed the evaluation.11 Several studies have reported SSI rate or pattern of surgical chemoprophylaxis but have not correlated SSI rates with pattern of surgical chemoprophylaxis.12–17
This study was undertaken to evaluate the pattern and rationality of antimicrobial drug prescribing by surgeons in perioperative patients using Kunin's criteria.11 SSI rate was calculated and difference among patients with appropriate and inappropriate surgical chemoprophylaxis was also analyzed. The aim of this study was to evaluate the current pattern of surgical chemoprophylaxis among patients undergoing surgical procedures in a tertiary care hospital and its impact on SSI rate.
Objectives of study- 1.
To assess the current pattern of surgical chemoprophylaxis and its rationality assessment based on Kunin's criteria11 and Scottish Intercollegiate Guidelines Network (SIGN)6 core indicators for auditing antimicrobial use in surgical chemoprophylaxis.
- 2.
To evaluate surgical site infection rate and difference in SSI rate if any between appropriate and inappropriate prescriptions.
Two hundred and twenty prescriptions of patients admitted in the General Surgery wards of a tertiary teaching hospital were collected prospectively between June 2010 and May 2011. The study protocol, pro-forma, and other documents like patient information sheet and informed consent form in English and local vernacular language were approved by Institutional Ethics Committee. All patients undergoing surgery irrespective of their age and gender were included. Patients who were not willing to give information were excluded from the study. Case records of enrolled patients, admitted for any operative procedures were recorded in the pro-forma containing demographic details, chief complaints, diagnosis, details of operative procedures and drug details during the hospital stay. Class of operation was decided in consultation with operating surgeons and was based on US National Research Council group criteria.18 SSI rate was calculated as defined by CDC,2 rationality assessment was done according to the Kunin's criteria11 shown in Table 1 based on CDC 1999 Guidelines5 as reference standard and also surgical audit based on SIGN guideline criteria.6 The analysis was done based on CDC guidelines because of unavailability of national or local guidelines. The generic names of drugs, generic contents of each formulation were obtained from the patient's pharmacy bills. Drugs and formulations which were not mentioned in the bills were obtained from local pharmacy stores and commercial publications like Indian Drug Review 2010 and 2011.
Kunin's criteria11 for rationality assessment of antimicrobial prescriptions.
| Category I: Agree with the use of antimicrobial therapy/prophylaxis, the program is appropriateCategory II: Agree with the use of antimicrobial therapy/prophylaxis, but a potentially fatal bacterial infection cannot be ruled out or prophylaxis is probably appropriate, advantages derived remain controversialCategory III: Agree with the use of antimicrobial therapy/prophylaxis, but a different (usually less expensive or toxic) antimicrobial is preferredCategory IV: Agree with the use of antimicrobial therapy/prophylaxis, but a modified dose is recommendedCategory V: Disagree with the use of antimicrobial therapy/prophylaxis, administration is preferredCategory VI: data cannot be judged because of missing information |
Data were analyzed by using SPSS 20.0 demo version®. Fisher's exact test (two tailed) was used to determine the significance of SSI positive rates among different variables and unpaired t-test was used to determine the difference between the inappropriate and appropriate prescription groups. Value of p<0.05 was considered as statistically significant.
ResultsA total of 220 patients were enrolled in the study of which 141 (64.1%) were males. The age ranges from 13 to 78 years; with mean age 38.88±14.18 (mean±S.D.). About 90% (197) underwent elective surgeries the rest being emergency surgeries. Most of the operative procedures were open 207 (94%) and the rest were laparoscopic. General anesthesia was used in 8 patients and in the rest either spinal or local anesthesia was used. Herniorrhaphy (27.3%) and appendectomy (20.5%) remained the most frequently performed operative procedures. Class I, i.e., clean surgeries 105 (47.73%) were most frequent, followed by class II, i.e., clean-contaminated 53 (24.09%), class III-contaminated 38 (17.27%), and class IV-dirty 24 (10.91%) as shown in Table 2. Mean hospital stay was 8.67±5.17 days (mean±S.D.).
All the patients undergoing operative procedures received single intravenous dose of antimicrobial 30min before the surgery, followed by post-operative intravenous therapy and further oral therapy with antimicrobial. Mean duration for pre-operative intravenous antimicrobial therapy was 0.75±0.45 days. Mean duration of post-operative intravenous antimicrobial therapy was 3.33±2.24 while post-operative oral antimicrobial therapy was 4.58±3.34 days. None of the operative procedures exceeded more than 4h duration.
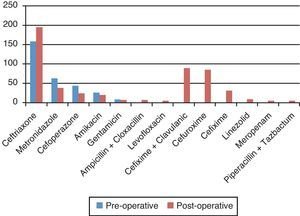
A total of 2294 drugs were prescribed out of which 840 (36.61%) were antimicrobials. Ceftriaxone was the most frequently used antimicrobial pre-operatively (50.64%) and post-operatively (36.93%) as shown in Fig. 1.
Out of 220 patients, 28 had suspected SSI. Nineteen patients out of 28 had microbiologically confirmed SSI, Escherichia coli (9) and Staphylococcus aureus (7) being the common pathogens. SSI rate was highest in class IV (41.66%) followed by in class III (7,69%), II (7,54%), and was least in class I (1.92%). SSI rate was significantly higher in patients who presented with diabetes mellitus (p<0.0001) and hypertension (p=0.0048) as shown in Table 3. SSI positive rate in 61 hernia patients was 2 (1.63%) while in 45 appendectomy patients the rate was 1 (2.22%). In these patients E. coli was the most common isolate. Mean age of SSI positive patients was found significantly higher as compared to SSI negative patients (p<0.001) which is depicted in Table 3. Patients with age above 40 years showed significant higher SSI positive rate as compared to patients less than 40 years. There was no significant difference for SSI rate between gender, types of anesthesia and between open and laproscopic surgery, while emergency surgery showed significantly higher SSI rate in comparison with elective surgery (p=0.0073). Mean hospital stay for SSI negative patients was 7.81±4.1 and that for SSI positive patient was 17.79±6.41, which shows a significant increase in mean hospital stay by 9.98 days (p<0.0001). Patients with hospital stay greater than a week had significantly higher rate (p<0.0001) of SSI positivity. Mean drugs prescribed in SSI negative were 7.43±1.74 and that in SSI positive patient was 11±2 yielding a significant (p<0.0001) increase of 3.57 drugs.
Surgical site infection (SSI) rates2 and variables.
| SSI negative (n=201) | SSI positive (n=19) | Total (n=220) | p valuea | |
|---|---|---|---|---|
| Mean age | 37.71±13.44 | 51.26±16.21 | 38.88±14.19 | <0.0001 |
| ≤40 years | 134 | 6 | 140 | 0.0047 |
| >40 years | 67 | 13 | 80 | |
| Gender | ||||
| Male | 131 | 10 | 141 | 0.32 |
| Female | 70 | 9 | 79 | |
| Days of hospital stay | 7.81±4.1 | 17.79±6.41 | 8.67±5.17 | <0.0001 |
| ≤7 days | 118 | 1 | 119 | |
| >7 days | 83 | 18 | 101 | |
| No. of drugs given | 7.43±1.74 | 11±2 | 10.42±3.37 | <0.0001 |
| Type of anesthesia | ||||
| General | 15 | 3 | 18 | 0.193 |
| Other SA and LA | 186 | 16 | 202 | |
| Mode of operation | ||||
| Elective | 184 | 13 | 197 | 0.0073 |
| Emergency | 17 | 6 | 23 | |
| Open | 188 | 19 | 207 | 0.60 |
| Laproscopic | 13 | 0 | 13 | |
| Co-morbid conditionsb | ||||
| Diabetes mellitus | 2 | 9 | 11 | <0.0001 |
| Hypertension | 10 | 5 | 15 | 0.0048 |
Using Fischer's exact two tailed test and unpaired t-test.
Antimicrobial prescriptions were categorized as appropriate (I and II) – 105(47.7%) and inappropriate (III, IV, and V) – 115 (52.3%) based on Kunin's criteria11 as shown in Table 4. SSI rate was significantly higher (p<0.05), in inappropriate group (13.04%) in comparison with appropriate group (3.8%) as shown in Table 4. Out of 61 hernia patients, 19 prescriptions were inappropriate out of which 2 patients had SSI (p=0.0934). Out of 45 appendectomy patients 35 prescriptions were inappropriate and one patient has SSI (p=1). Rate of SSIs in patients who receive inappropriate prophylaxis (as defined by CDC guideline5) compared with rate of this infection in patients who receive appropriate prophylaxis, expressed as a ratio was found to be 3.43. Table 5 depicts the process measures and outcome measures according to SIGN guidelines.6
Appropriateness of surgical prophylaxis based on Kunin's criteria11 and surgical site infection rate (n=220).
| Appropriate therapy | ||||
|---|---|---|---|---|
| Category I | Category II | Subtotal | SSI positive | SSI negative |
| 2(0.91%) | 103(46.81%) | 105(47.72%) | 4 | 101 |
| Inappropriate therapy | |||||
|---|---|---|---|---|---|
| Category III | Category IV | Category V | Subtotal | SSI positive | SSI negative |
| 108(49.09%) | 0(0%) | 7(3.19%) | 115(52.28%) | 15 | 100 |
Fishers exact test, p=0.0165, significant.
Core indicators for surgical audit based on SIGN guidelines.6
| (a)Process measures | ||
| 1 | Was prophylaxis given for an operation included in local guidelines? | No local guideline available |
| 2 | If prophylaxis was given for an operation not included in local guidelines, was a clinical justification for prophylaxis recorded in the case notes? | Justification was not recorded in the case note |
| 3 | Was the first dosage of prophylaxis given within 30min of the start of surgery? | Yes |
| 4 | Were the choice, dosage and route of administration consistent with local guidelines for that procedure? | Consistent without guideline |
| 5 | Was the prescription written in the “once-only” section of the drug prescription chart? | Not applicable |
| 6 | Was the duration of prophylaxis greater then 24h? | Yes |
| (b)Outcome measures | ||
| 1 | Surgical site infection rate=number of SSIs occurring postoperatively/total number of operative procedures | 19/220=0.0864 (8.64%) |
| 2 | Rate of SSIs occurring postoperatively in patients who receive inappropriate prophylaxis (as defined in guideline) compared with rate of this infection in patients who receive appropriate prophylaxis, expressed as a ratio | 13.04/3.8=3.43 |
| 3 | Rate of Clostridium difficile infections occurring postoperatively in patients who receive inappropriate prophylaxis (as defined in guideline) compared with rate of this infection in patients who receive appropriate prophylaxis, expressed as a ratio | No culture recorded Clostridium difficile infection |
This study was aimed to evaluate the current prescribing pattern along with rationality, its impact on SSI rate and on hospital stay and number of extra drugs needed. Previous study from Pakistan12 reported 55.7% males lower compared to ours 64%, mean age of the patients was 35±17 years, and somewhat less compared to our study, i.e., 38.8%.
In our study SSI rate was 8.64% which was similar to previous studies.13 In our study E. coli was most commonly isolated pathogen, followed by S. aureus which is in accordance with previous Indian study.19 SSI rate for two most commonly performed surgeries herniorrhaphy and appendectomy is comparable to an earlier study carried out in India14 and a worldwide meta analysis study.20 There is no significant difference in SSI rate between genders, this finding is similar to a previous study reported in Iran in 2006.21 SSI rate increases with age above 40 years, which was statistically significant at p<0.0001 and was similar to study reported from India.22 SSI rate among patients receiving general anesthesia in our study was 16.67% as compared to other modes (7.92%), which is in accordance with previous study done in UK.23 SSI rate was higher in emergency surgery than in elective and is comparable to another Indian study.14 In our study SSI rate was significantly higher in diabetic and hypertensive patients which was also seen in a previous Indian study.22 In our study there was no difference in SSI rate between laproscopic and open surgery. A study by Jawien et al.15 reported less SSI rate in laproscopic surgery than in open surgery. SSI led to significantly extended hospital stay (9.98 days) which is similar to a European study (1998)24 which reported 9.8 days.
In our study a single pre-operative dose of antimicrobial therapy was given before the operative procedure which is in accordance with the various standard guidelines and previous studies also showed that single dose prophylaxis is not associated with increased rate of SSI when compared to multiple dose regimens.25 In our study mean duration of pre-operative intravenous therapy was 0.75±0.45 days, followed by mean post-operative intravenous therapy for 3.33±2.24 and post-op oral therapy for 4.58±3.34 days. However timing of administration of first dose of antimicrobial pre-operatively was in compliance with the CDC guidelines.5 Mean duration of post-operative antimicrobial use was 7.88 days which is longer than reported by previous study from India, i.e., 5 days16 which may be due to differences in prevalent practices. All patients received antimicrobials, in both the pre-operative and post-operative period, and no antimicrobial was given in the intra-operative period. Most commonly used drug group for prophylaxis was third generation cephalosporins, followed by metronidazole, and penicillin group similar to an Indian study.17 In our study none of the patients received cefazolin as recommended by various guidelines.5–8
For surgical prophylaxis it is important to select an antimicrobial with narrowest antibacterial spectrum to reduce the emergence of resistance, secondly the antimicrobial antibiotic must be active against the most likely contaminating microorganisms for that type of surgery, the first-generation cephalosporins are excellent agents for skin and soft tissue infections owing to Streptococcus pyogenes and methicillin-susceptible S. aureus. Hence a single dose of cefazolin just before surgery is the preferred prophylaxis for procedures in which skin flora are the likely pathogens. For patients undergoing clean operative procedure for herniorrhaphy, a clean procedure a single dose of cefazolin 1g preoperatively and for appendectomy, a clean contaminated surgery single preoperative intravenous dose of either cefotetan or cefoxitin 1g is recommended.5–8 Therefore, it is recommended that the use of third generation cephalosporins such as ceftriaxone and cefotaxime be avoided in surgical prophylaxis as it may be required later if patient develops serious sepsis For herniorrhaphy use of cefazolin is appropriate, while in case of appendectomy third generation cephalosporins have been used as substitute for cefotetan and cefoxitin in our study as in India cefazolin is available while cefotetan and cefoxitin are not marketed.26 However this is not justified, as third generation cephalosporins have to be spared for therapeutic purpose. Better option would be an alternative like cefuroxime. Dirty and contaminated surgeries required broad spectrum antimicrobials coverage. Drugs like piperacillin, tazobactum, linezolid were used mainly after diagnosis of SSI for therapeutic purpose.
In our study 52% patients received inappropriate chemoprophylaxis according to Kunin's criteria.11 This finding is in accordance with earlier studies that showed 51.5%11 and 65.6%27 respectively. Most of the antimicrobials were broad spectrum, prescribed for longer duration which was unwarranted. Inappropriate prophylaxis was associated with higher culture positive (SSI positive) rates (13.04%) as compared to the appropriate prophylaxis (3.8%).
To our knowledge this study is first of its kind in India. Strength of this study was the assessment of rationality of chemoprophylaxis based on Kunin's criteria11 and SIGN guideline6 as well as comparison of SSI rate in patients receiving appropriate and inappropriate chemoprophylaxis. One of the limitations of our study is cross-sectional design of the study. Also there was no patient follow up after discharge up to 30 days which is required according to CDC definition of SSI and hence some cases of SSI after discharge from hospital may be missed. Patient post-discharge questionnaire was not used and further analysis based on quality of life could be done. Further studies with larger sample size can be planned including additional cost borne by the patient because of inappropriateness. In depth sub analysis into various types of surgeries and various drug regimens and infections can be done to select a proper and rational regimen for an individual surgery using other guidelines. Kunin's criteria11 is a preliminary evaluation of appropriateness, a further in-depth analysis of antimicrobial prescription can be done according to the Modified Kunin's criteria,25 Giessen score,28 and by SWABs score.29 Evaluation based on the combined scores from both the surgical wound judgment and prescription analysis can also be done.
ConclusionInappropriate chemoprophylaxis as evident in this study is associated with higher SSI rate leading to prolongation of hospital stay and increased number of drugs usage. Adoption of international standard and formulation of locally feasible guidelines can help overcome this situation. However this is a single center study and results of this study may not be generalized.
Conflict of interestThe authors have no conflict of interest to declare.
The authors would like to express their thanks to Dr. Pankaj R. Patel, Dean, Smt. NHL Medical College and Dr. M.H. Makwana, Superintendent, V.S. Hospital for permitting them to do this work in V.S. Hospital. The authors also express gratitude to surgery department for support.