Mobility restrictions and overloaded health services during the COVID-19 pandemic compromised services dedicated to the prevention and care of HIV and other sexually transmitted infections (STI). In this study, we present client's responses to standardized questionnaires applied during the COVID-19 pandemic period as part of the strategy to measure impacts on social and sexual vulnerability, access to STI prevention services, and access to STI care.
MethodsThe questionnaires included variables on sociodemographics, behavior, risk perception, prevention attitudes, barriers to service-based HIV rapid test, reasons for taking an HIV self-test, and access to health services for STI diagnosis and treatment. We explored demographic variables associated with income reduction, reduced access to HIV/STI testing/treatment and increased vulnerability to HIV/STI.
Results847 participants responded to the study questionnaire between May 2020 and January 2021. Most were young, cisgender male, and 63% self-reported as men who have sex with men. Income reductions were reported by 50%, with 30% reporting a decline over 50% of total income. An increase in heavy episodic drinking (>5 doses) was reported by 18%; 7% reported more sexual partners and 6% reported using condoms less often. Difficulties in obtaining HIV tests, tests for other STI and treatment for STI were reported by 5%, 6% and 6%, respectively. Lower schooling was significantly associated with income reduction (p = 0.004) and with reduced access to HIV/STI testing or STI treatment (p = 0.024); employment status was associated with income reduction (p < 0.001) and increased vulnerability to HIV/STI (p = 0.027). Having access to an expedite test result, avoiding physical attendance in health units during the pandemic, and undertaking the test with privacy with a trusted person were reported as motivators for HIV self-test.
ConclusionsOur findings are relevant to promote service improvements tailored to subgroups more likely to struggle with detrimental effects during and after the COVID-19 pandemic.
The worldwide spread of COVID-19, declared a pandemic by the World Health Organization (WHO) on March 2020,1 was initially reported in Brazil on February 2020, with national community transmission identified since March 2020 by the Ministry of Health.2 Since May 2020, Brazil has been standing out as one of the three most affected countries in the world.3
The COVID-19 pandemic has had detrimental effects on global healthcare systems/programs and on almost every aspect of human life.4 Mobility restrictions and overloaded health services caused by the pandemic may directly or indirectly impact the quality of care for other health conditions, including sexual health and epidemics such as HIV and other sexually transmitted infections (STI).5,6 In addition, the COVID-19 pandemic may affect people's sexual behavior and adherence to STI prevention strategies. Such changes may reflect on STI and HIV prevention, diagnosis, and treatment, negatively impacting these epidemics7-10. Social determinants of health may also contribute to the disproportionate effect of COVID-19 among vulnerable populations not only on health, but also on economic aspects,11,12 since working and living conditions as well as income influence the risk of SARS-CoV-2 infection and/or transmission.13-15
Aids Healthcare Foundation (AHF) is a nonprofit organization that has been providing HIV testing, prevention, and care in 44 countries for more than 30 years.16 The Men's Clinic managed by AHF in the city of Recife, Brazil, is in continuous operation since May 2018, focusing on STI and HIV diagnosis and care for the male population.17 Most clients in the clinic are self-identified cisgender men, and a minority as transgender men; assistance can be provided for women in exceptional cases, such as recent HIV diagnosis. Given its location in central Recife, free of charge care, differentiated working hours, and comprehensive, targeted care for populations at greater vulnerability to HIV and STIs, the service offers unique opportunities for the implementation of new care strategies, expanding access to sexual health care. During the first two years of operation, the clinic provided more than 14,000 first consultations, representing an innovative initiative in the region. In order to mitigate the negative impacts of COVID-19, the Men's Clinic has implemented telemedicine, universal flu symptoms screening for clients attending in-person consultations, and expedited care for urgent conditions, including immediate syndromic treatment for symptomatic STIs. In addition, the service made available for the first-time HIV self-tests (HIVST) as to improve access to diagnosis during the pandemic period.
In this cross-sectional study, we describe clients’ responses to questionnaires applied at the Men's Clinic during the COVID-19 pandemic period as part of a strategy to understand and mitigate the potential negative impacts on STI and HIV care. The COVID-19 impact assessment questionnaire included demographics, data on vulnerability and prevention attitudes, impact of COVID-19 on income, access to social support payment and access to STI testing and care. We explored associations between sociodemographic variables (age, schooling and employment) and variables depicting COVID-19 impact on income, increased vulnerability to STI and access to HIV and other STI testing and treatment. A second questionnaire was applied to clients who retrieved HIVST in the clinic, including demographics, barriers to the use of service-based HIV rapid test, and reasons for taking an HIVST.
MethodsParticipants and settingClients aged 18 years and older attending the Men's Clinic in person were invited to respond the COVID-19 impact assessment questionnaire. Clients who requested an HIVST were invited to a separate questionnaire addressing barriers to the use of service-based HIV rapid test, and reasons for taking an HIVST. Responses were collected by a trained healthcare provider, who informed clients that participation was voluntary and confidential.
Ethical aspectsThis study was approved by the Ethics Committee at Complexo Hospitalar HUOC/PROCAPE (approval number 34779220.9.0000.5192) with exemption of informed consent for data collected in the COVID-19 impact assessment questionnaire, retrospectively assessed for this study. For the questionnaire applied to clients requesting HIVST, all participants provided consent for participation.
Statistical analysisCharacteristics of study participants were presented using descriptive statistics. We described the frequency and percentage of responses in each question regarding the impacts of COVID-19 and HIVST. Associations between demographic variables and the detrimental effects of COVID-19 on income, vulnerability to STI and access to STI testing and treatment were analyzed using chi-square tests. We used Stata 15.1 for all analyses with a two-tailed significance level of 0.05.
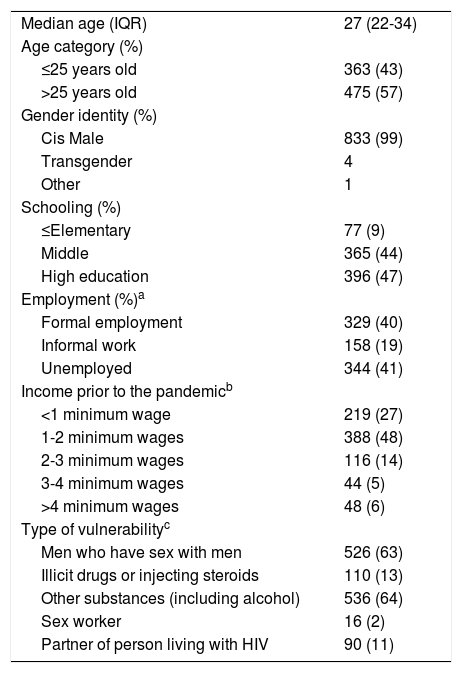
ResultsBetween May 2020 and January 2021, 847 clients were invited to answer the COVID-19 impact assessment questionnaire. After the exclusion of four individuals who did not provide consent and five female clients, the final sample comprised 838 participants. Sociodemographics and vulnerability characteristics are presented in Table 1. Participants were mostly young (median age 27; 43% aged ≤25 years old) and 99% self-identified as cisgender males. Although most participants had middle school education or higher, 41% were unemployed and 75% reported a monthly income ≤2 Brazilian minimum wages, corresponding to ≤400 US dollars. Use of psychoactive substances (including alcohol) and having sex with men were the most frequently reported vulnerability categories.
Demographics and vulnerability characteristics of study participants.
| Median age (IQR) | 27 (22-34) |
| Age category (%) | |
| ≤25 years old | 363 (43) |
| >25 years old | 475 (57) |
| Gender identity (%) | |
| Cis Male | 833 (99) |
| Transgender | 4 |
| Other | 1 |
| Schooling (%) | |
| ≤Elementary | 77 (9) |
| Middle | 365 (44) |
| High education | 396 (47) |
| Employment (%)a | |
| Formal employment | 329 (40) |
| Informal work | 158 (19) |
| Unemployed | 344 (41) |
| Income prior to the pandemicb | |
| <1 minimum wage | 219 (27) |
| 1-2 minimum wages | 388 (48) |
| 2-3 minimum wages | 116 (14) |
| 3-4 minimum wages | 44 (5) |
| >4 minimum wages | 48 (6) |
| Type of vulnerabilityc | |
| Men who have sex with men | 526 (63) |
| Illicit drugs or injecting steroids | 110 (13) |
| Other substances (including alcohol) | 536 (64) |
| Sex worker | 16 (2) |
| Partner of person living with HIV | 90 (11) |
Brazilian minimum wage currently corresponds to approximately 197 US dollars.
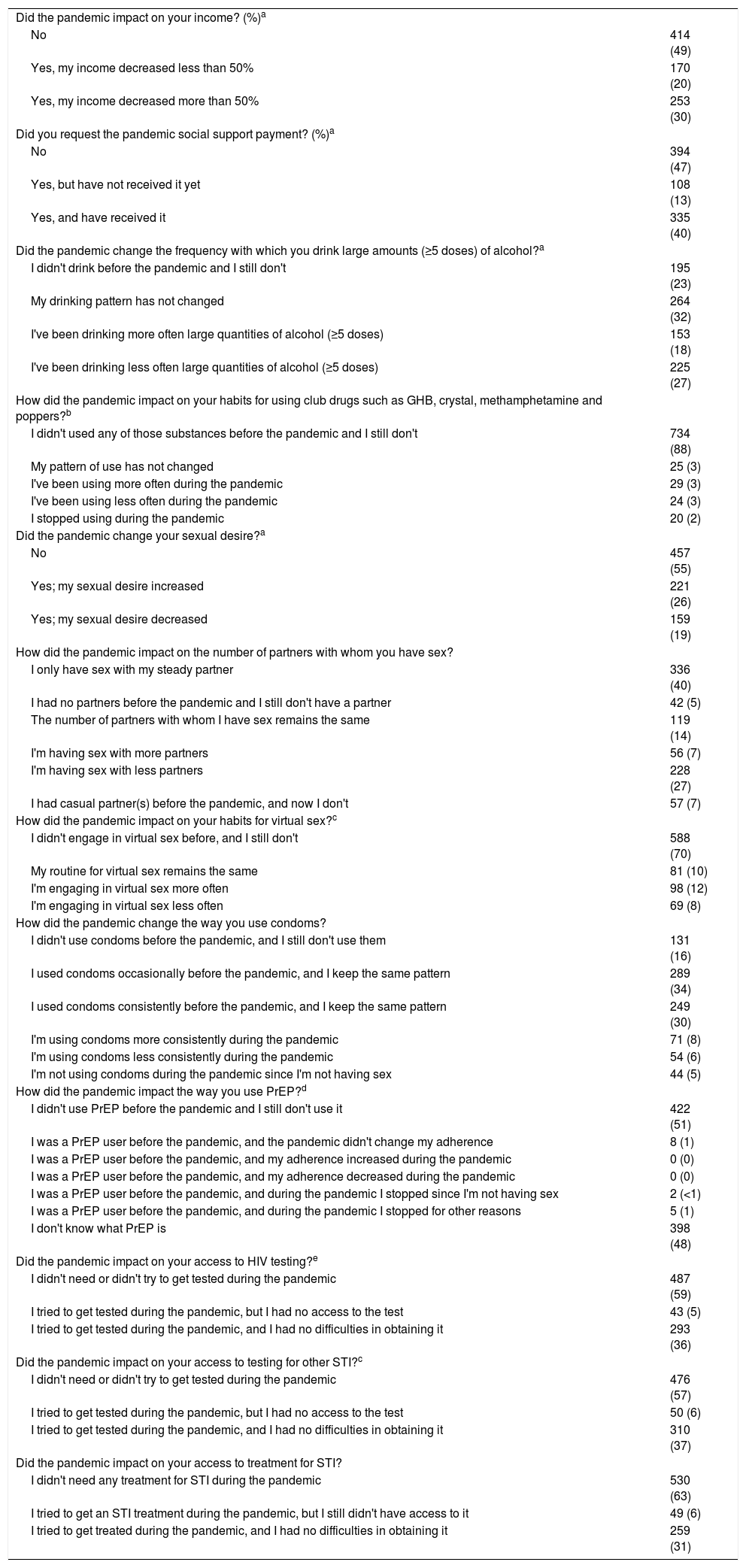
We addressed the impact of COVID-19 on income, prevention attitudes and access to testing and treatment of STI using close-ended questions as described in Table 2. Income reductions were reported by 50%, with 30% of participants reporting a decline of more than 50% of total income. The social support payment, offered during the pandemic period by the Brazilian government, had been received or requested by 53%. An increase in heavy episodic drinking (>5 doses) was reported by 18%. Very few participants reported using club drugs, and only 3% reported using more often during the pandemic. Sexual desire was described as increased by 26%; 7% reported more sexual partners and 6% reported using condoms less often; more frequent engagement in virtual sex was reported by 12%. Difficulties in obtaining HIV tests, tests for other STI and treatment for STI were reported by 5%, 6% and 6%, respectively. Finally, 7% withdrew HIV Pre-Exposure Prophylaxis (PrEP) during the pandemic, either for lack of sexual exposure or for other reasons; strikingly, 48% of participants reported not knowing what PrEP was.
Impact of COVID-19 on income, prevention attitudes and access to healthcare.
| Did the pandemic impact on your income? (%)a | |
| No | 414 (49) |
| Yes, my income decreased less than 50% | 170 (20) |
| Yes, my income decreased more than 50% | 253 (30) |
| Did you request the pandemic social support payment? (%)a | |
| No | 394 (47) |
| Yes, but have not received it yet | 108 (13) |
| Yes, and have received it | 335 (40) |
| Did the pandemic change the frequency with which you drink large amounts (≥5 doses) of alcohol?a | |
| I didn't drink before the pandemic and I still don't | 195 (23) |
| My drinking pattern has not changed | 264 (32) |
| I've been drinking more often large quantities of alcohol (≥5 doses) | 153 (18) |
| I've been drinking less often large quantities of alcohol (≥5 doses) | 225 (27) |
| How did the pandemic impact on your habits for using club drugs such as GHB, crystal, methamphetamine and poppers?b | |
| I didn't used any of those substances before the pandemic and I still don't | 734 (88) |
| My pattern of use has not changed | 25 (3) |
| I've been using more often during the pandemic | 29 (3) |
| I've been using less often during the pandemic | 24 (3) |
| I stopped using during the pandemic | 20 (2) |
| Did the pandemic change your sexual desire?a | |
| No | 457 (55) |
| Yes; my sexual desire increased | 221 (26) |
| Yes; my sexual desire decreased | 159 (19) |
| How did the pandemic impact on the number of partners with whom you have sex? | |
| I only have sex with my steady partner | 336 (40) |
| I had no partners before the pandemic and I still don't have a partner | 42 (5) |
| The number of partners with whom I have sex remains the same | 119 (14) |
| I'm having sex with more partners | 56 (7) |
| I'm having sex with less partners | 228 (27) |
| I had casual partner(s) before the pandemic, and now I don't | 57 (7) |
| How did the pandemic impact on your habits for virtual sex?c | |
| I didn't engage in virtual sex before, and I still don't | 588 (70) |
| My routine for virtual sex remains the same | 81 (10) |
| I'm engaging in virtual sex more often | 98 (12) |
| I'm engaging in virtual sex less often | 69 (8) |
| How did the pandemic change the way you use condoms? | |
| I didn't use condoms before the pandemic, and I still don't use them | 131 (16) |
| I used condoms occasionally before the pandemic, and I keep the same pattern | 289 (34) |
| I used condoms consistently before the pandemic, and I keep the same pattern | 249 (30) |
| I'm using condoms more consistently during the pandemic | 71 (8) |
| I'm using condoms less consistently during the pandemic | 54 (6) |
| I'm not using condoms during the pandemic since I'm not having sex | 44 (5) |
| How did the pandemic impact the way you use PrEP?d | |
| I didn't use PrEP before the pandemic and I still don't use it | 422 (51) |
| I was a PrEP user before the pandemic, and the pandemic didn't change my adherence | 8 (1) |
| I was a PrEP user before the pandemic, and my adherence increased during the pandemic | 0 (0) |
| I was a PrEP user before the pandemic, and my adherence decreased during the pandemic | 0 (0) |
| I was a PrEP user before the pandemic, and during the pandemic I stopped since I'm not having sex | 2 (<1) |
| I was a PrEP user before the pandemic, and during the pandemic I stopped for other reasons | 5 (1) |
| I don't know what PrEP is | 398 (48) |
| Did the pandemic impact on your access to HIV testing?e | |
| I didn't need or didn't try to get tested during the pandemic | 487 (59) |
| I tried to get tested during the pandemic, but I had no access to the test | 43 (5) |
| I tried to get tested during the pandemic, and I had no difficulties in obtaining it | 293 (36) |
| Did the pandemic impact on your access to testing for other STI?c | |
| I didn't need or didn't try to get tested during the pandemic | 476 (57) |
| I tried to get tested during the pandemic, but I had no access to the test | 50 (6) |
| I tried to get tested during the pandemic, and I had no difficulties in obtaining it | 310 (37) |
| Did the pandemic impact on your access to treatment for STI? | |
| I didn't need any treatment for STI during the pandemic | 530 (63) |
| I tried to get an STI treatment during the pandemic, but I still didn't have access to it | 49 (6) |
| I tried to get treated during the pandemic, and I had no difficulties in obtaining it | 259 (31) |
STI, sexually transmitted infections; GHB, gamma-hydroxybutyrate.
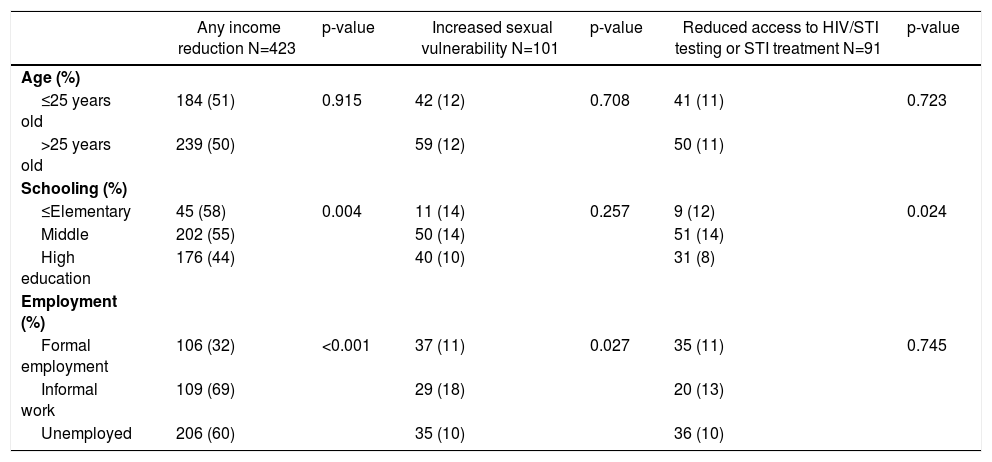
We explored if age category, schooling and employment were associated with COVID-19 impact on income, HIV vulnerability and access to HIV and other STI testing and treatment. For this analysis, we generated binary outcome variables for income reduction (no vs. any decrease), HIV/STI vulnerability (participants reporting increased number of sexual partners and/or using condoms less consistently during the pandemic vs. others), and access to HIV/STI testing and STI treatment (participants declaring to have tried but couldn't get tested/treated vs. others). Results are presented in Table 3. Lower level of schooling was significantly associated with income reduction (p = 0.004) and with reduced access to HIV/STI testing or STI treatment (p = 0.024); employment status was associated with income reduction (p < 0.001) and increased vulnerability to HIV/STI (p = 0.027). Interestingly, there was no statistically significant associations between employment status and access to HIV/STI testing or STI treatment.
Associations between sociodemographic variables and Covid-19 impact on income, HIV vulnerability and access to HIV and other STI testing and treatment.
STI, sexually transmitted infections.
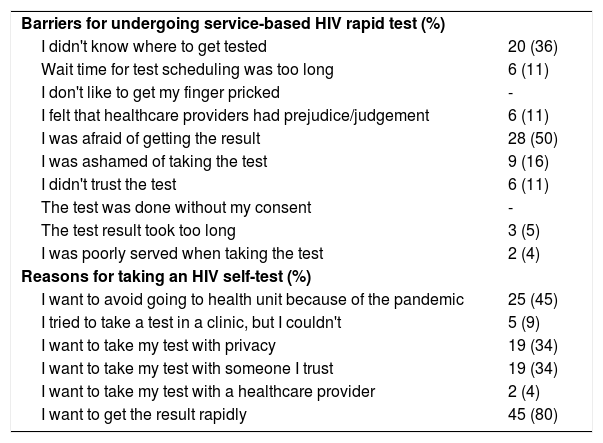
A total of 56 clients who retrieved HIVST in the clinic between August 2020 and January 2021 responded to the study questionnaire at the moment they obtained the test; of those, 31 (55%) responded to the study questions after performing the test. All respondents were male, with a median age of 26 years old (range 18-53), and all reported that they had already been tested for HIV in the past. Most (95%) requested more than on HIVST kit; reasons for requesting additional tests included the need for repeating the test (75%) and offering the test to a friend (64%) or a partner (43%). Barriers reported for undergoing a service-based HIV rapid test and reasons for making the HIVST are described in Table 4. Fear of getting the test result and not knowing where to be tested were reported as barriers for service-based tests by 50% and 36% respectively. Getting a quick test result, avoiding physical attendance in the health unit during the pandemic, and undertaking the test with privacy and in the company of a trusted person were reported as motivators for HIVST.
Barriers previously observed for undergoing and HIV rapid test and reasons for requesting the HIV self-test
Among participants who responded to the questionnaire after taking HIVST, only one had a positive result. We asked if clients experienced any difficulties such as fear of doing the test incorrectly; fear of the finger prick; insufficient volume of blood; difficulties in understanding test instructions; or difficulties interpreting test result. None of these problems were reported.
DiscussionIn this cross-sectional study, we found that the COVID-19 pandemic had a detrimental effect on income and HIV/STI vulnerability for a large proportion of clients of the Men's Clinic, whereas access to HIV and other STI testing and treatment was less often impacted. We found that lower level of schooling was associated with both income reduction and reduced access to HIV/STI testing or STI treatment, and unemployment/informal work was associated with income reduction (p < 0.001). Interestingly, participants reporting informal work were more likely to report increased vulnerability to HIV/STI than those who had formal jobs or those who were unemployed. In addition, our findings also suggest that HIVST is a powerful strategy to overcome barriers for service-based testing during the pandemic, or even in non-pandemic times, as several advantages have been pointed out by study participants.
The Men's Clinic implemented a number of mitigation strategies during the COVID-19 pandemic period, including appointments via electronic tools, universal flu symptom screening for clients seen in person, immediate syndromic treatment for symptomatic STI and distribution of HIV self-tests for HIV diagnosis. Nevertheless, negative effects of the pandemic on patient care and social conditions were still expected. Detrimental effects of the COVID-19 pandemic on income have been reported in studies conducted in the general population and among patients living with HIV, leading to adverse social and mental health outcomes.18,19 Impairments to HIV testing and treatment, particularly for antiretroviral treatment (ART) initiation, have also been shown in studies conducted in Australia20 and South Africa.21 Medium and long-term consequences of service disruptions are expected and have been anticipated in mathematical modeling studies. In a study using data from Cameroon and Benin, a 6-month disruption in ART initiation and a 50% reduction in the provision of HIV prevention/treatment was projected to increase HIV incidence by 50% and HIV-related deaths by 20%.22 Similarly, a modeling study using Chinese data showed that the overall impact of COVID-10 on HIV incidence and HIV-related deaths depend on which services are disrupted and the intensity and duration of impairments.23
Although 27% of our participants reported a lower number of sexual partners, most reported unaltered patterns of sexual exposure, whereas 7% reported a larger number of sexual partners. These results are consistent with finding reported by Sousa et al. , who showed that engagement in casual sex is persistent among MSM during the period of physical distancing due to COVID-19.24 Engagement in virtual sex, a safe alternative for sex during the pandemic, was reported by 30% of our study participants, while only 12% reported engaging more often in this practice. This low percentage could be partially attributed to low income and poor access to internet in our sample. However, it is also likely that in-person sexual contact is largely preferred in a context of mild mobility restrictions such as those observed in Brazil.
Regarding the impact of COVID-19 on psychoactive substance use, 18% of our participants reported an increase in heavy episodic drinking (>5 doses) and 3% reported increase in club drugs use during COVID-19 pandemic. Similar patterns have been reported in a US sample of MSM.25 Increase in alcohol consumption during the COVID-19 pandemic has been reported in other studies.24 Interactions between psychoactive substance use and sexual risk behavior are complex, and it is widely accepted that acute intoxication with alcohol or other drugs is associated with increased likelihood of unprotected sex.26,27 It is also plausible to assume that risk behavior towards exposure to COVID-19 may be impacted by psychoactive substance use.
Of note, a high percentage of participants (53%) reported requesting social support payment during the pandemic. This is likely a consequence of low rates of formally employed participants, high levels of unemployment, low income and the ongoing economic crisis in Brazil and intensified over the course of the COVID-19 pandemic.28
We were surprised to see that PrEP was unknown to almost half of study respondents (48%) despite its free of charge availability in Brazil since December 2017,29 and despite sample recruitment in a health unit that offers HIV prevention counseling to highly vulnerable populations. Although PrEP has been shown to be a robust biomedical strategy to prevent HIV infection, real-life roll-out and implementation among vulnerable populations remain low.30-34
Our study had a few limitations. We were restricted to a small sample in the HIVST questionnaire, particularly in the post-HIVST subgroup. Participants included in the COVID-19 impact assessment questionnaire are representative of the target population for the Men's Clinic, and likely portray Brazilian people newly diagnosed with HIV and/or syphilis - male youths, gays and other men who have sex with men.35-38 However, our study failed to explore the impact of COVID-19 among women and other subgroups with high vulnerability.
Our results support the urgency to maintain both primary care facilities and other types of HIV/STI care services open and operating both online and in strategic places during pandemic.39,40 Barriers identified to access service-based HIV rapid test suggest important structural barriers that could be overcome using technologies such as HIVST. Public health strategies should be undertaken early, prioritizing the diagnosis, care, and treatment of HIV and other STI in order to avoid drawbacks in incidence rates and in complications due to late diagnosis or delay in STI/HIV treatment initiation.41,42 Finally, our findings emphasize the need to better understand the social determinants related to HIV/STI epidemics, highlighting the crisis generated by the COVID-19 pandemic. A deeper comprehension of socioeconomic factors that influence access to health services will contribute to improve strategies to enhance responses against HIV/STI and mitigate the impact of COVID-19. This study can also contribute to bring service improvements by reducing structural barriers and increasing access to HIV and STI prevention, diagnosis, and treatment during and after the COVID-19 pandemic.
We thank healthcare workers in Men's Clinic who committed tremendous efforts to keep assisting clients and provided data for this study.