Hepatitis C is an important health problem. In Brazil, 1–2 million people are infected. Despite this expressive number, and the availability of very successful treatment, many patients remained undiagnosed mainly because of the asymptomatic nature of the infection.
ObjectivesTo describe epidemiological characteristics of HCV-infected patients seen at referral centers in Brazil, the source of referral, and the time spanned to reach a reference center, in order to improve the identification of undiagnosed patients.
MethodsMulticenter observational, cross-sectional study carried out in 15 centers of Brazil, between January/2016 and June/2017. Data of patients with a confirmed diagnosis (anti-HCV and HCV-RNA) were collected by interview using standard questionnaires and by review of charts.
ResultsTwo thousand patients were included; 55.1% were male, mean age 58±11 years. Only 14.9% had higher education and 84.2% received up to five monthly minimum Brazilian wages (approximately US$260.00/month). The time between diagnosis and beginning of follow-up was 22.9 months. The most common reasons for testing were check-up (33.2%) and blood donation (19%). General practitioners diagnosed most of the patients (30.1%). Fibrosis stage was mainly evaluated by liver biopsy (61.5%) and 31.3% of the patients were cirrhotic at diagnosis.
ConclusionsThis multicenter Brazilian study showed that the mean time to reach a referral center for treatment was almost two years. Primary care physicians diagnoses most hepatitis C cases in the country. Population campaigns and medical education should be encouraged to intensify screening of asymptomatic individuals, considering the efficiency of check-ups in identifying new patients.
Infection with hepatitis C virus (HCV) is an important public health problem since it is a leading cause of chronic liver disease in the world. Progression to chronic infection occurs in most HCV infected individuals, which can result in liver cirrhosis and hepatocellular carcinoma.1 In 2010, more than 0.5 million deaths worldwide were attributed to hepatitis C.2
The global prevalence of chronic HCV infection is estimated at 1.0% (95% uncertainty interval 0.8–1.1), corresponding to 71.1 million (62.5–79.4) viremic patients worldwide.3 The prevalence of HCV infection varies from 0.1 to 15% according to the region studied and in Latin American is estimated around 1.23%.4
HCV is mainly transmitted by parenteral route. In the past, blood and blood products were the main source of parenteral transmission of HCV. However, the introduction of serological tests for anti-HCV detection in 1992 has almost eliminated this route of transmission.1 Currently, the main source of parenteral transmission is the use of intravenous drugs, especially in developed countries. Intravenous drug use is also becoming an important source of infection in developing countries, accounting for 40% or more of infected individuals. Other parenteral sources such as tattoos, acupuncture, manicure, and piercing are considered unapparent routes of transmission.1 Non-parenteral transmission such as sexual and vertical transmission is uncommon. However, sexual transmission has been observed in Brazil between 2007 and 2016 in patients coinfected with HIV, corresponding to 9.8% (149,537) of cases.5
In Brazil, about two million people are estimated to be infected with HCV.6 In a population-based study conducted in the capital cities of the five regions of Brazil, the overall prevalence of anti-HCV was 1.3%. However, this number increased to 1.6% in patients aged 20 to 69 years.7 In the group of patients with positive HCV-RNA and anti-HCV, 64.1% of cases occurred in the Southeast, 24.5% in the South, 5.5% in the Northeast, 3.3% in the Midwest, and 2.5% in the North region. Recent data showed that the total detection rate of the disease has increased from 7/100.000 people in 2003 to 15.5/100.000 people in 2016. Using data from 1999 to present, 182,389 cases of hepatitis C were confirmed, most of them (58.5%) in men and in patients older than 60 years (18.8%).5
Despite the large number of HCV-infected individuals in Brazil, few patients have been treated so far. It is estimated that only about 5% of patients received treatment for chronic hepatitis C,6 with most infected patients having not yet been identified. Since the disease remains asymptomatic for long periods of time, patients rarely have access to diagnosis. This could be due to many socio-economic factors such as: low educational level, financial constraints, and transportion. Thus, these factors also make initiatives targeting patients complex and inefficient.
The aims of the present study were to describe the epidemiological characteristics of patients with chronic hepatitis C seen at referral centers in Brazil, to identify the source of referral, and the time spanned before reaching a reference center. This information will help elaborating better strategies to identify undiagnosed patients.
Patients and methodsThis was a multicenter hospital-based, cross-sectional study conducted from January 2016 through June 2017 aiming at documenting the characteristics of patients with a primary diagnosis of hepatitis C in Brazil.
Participating centers: Universidade Federal de São Paulo (UNIFESP-EPM); Faculdade de Medicina, Universidade Federal do Rio de Janeiro (UFRJ); Hospital Universitário Gaffrée e Guinle, Universidade Federal do Estado do Rio de Janeiro (UNIRIO); Hospital das Clínicas, Universidade Estadual de Campinas (UNICAMP); Hospital das Clínicas de São Paulo (HC-FMUSP), Hospital das Clínicas de Porto Alegre – Núcleo de Investigação em Vacinas; Secretaria Municipal de Saúde de Curitiba; Hospital das Clínicas, Universidade Federal de Pernambuco (UFPE); Hospital São Rafael – Monte Tabor (BA); Hospital Universitário, Universidade Federal do Maranhão (UFMA); Hospital Universitário Walter Cantídio, Universidade Federal do Ceará (UFC), and Universidade Federal do Mato Grosso do Sul (UFMS).
The inclusion criteria were age older than 18 years, either sex, receiving follow-up at the participating referral centers, and being diagnosed with chronic hepatitis C (anti-HCV and HCV-RNA positive) for more than six months. Patients were retrieved from the outpatient departments of participating centers. Only patients who could provide informed consent were included. Patients who refused to provide written informed consent, patients with a psychiatric or neurocognitive condition that impaired the collection of reliable clinical data at the discretion of researchers were excluded.
To avoid selection bias, special attention was taken to ensure that all patients who met the eligibility criteria participated in the survey using a consecutive (non-probability) sample. All patients scheduled for medical appointment in the reference centers were invited to participate during the period of study. The centers competitively included consecutive patients until reaching the target of 2000 patients.
Initially, trained researchers interviewed the patients to collect information, using a standard questionnaire on sex, age, place of birth, origin, educational level, marital status, profession, and socioeconomic status. Additional data regarding the diagnosis of chronic hepatitis C such as reason for the first anti-HCV test, site where the test was performed, center to which the patient was referred, waiting time to first appointment, and waiting time to first treatment were collected. After the interview, results of liver biopsy or elastography, fibrosis stage, genotype, and comorbidities were obtained from the chart (this item does not apply in case this was the first visit of the patient.
Since this was an observational epidemiological study, no treatment instructions were given and there was no interference in local routine procedures.
Statistical analysisA detailed statistical analysis plan was elaborated before the beginning of the study. For summary statistics, quantitative variables are expressed as mean and standard deviation in the presence of a normal distribution, or as median and interquartile range in the presence of an skewed distribution. Qualitative variables are reported as absolute (number of patients) and relative (percentage) frequencies.
The outcomes are described by the overall percentage considering all centers and by the percentage in each center and are expressed as proportions and their respective 95% confidence intervals. In the case of wide variability, a mean value weighted by the variance in each center was generated.
A two-tailed level of significance of alpha=0.05 was used in all tests. Sample size calculation assuming an absolute sampling error of 2%, alpha of 5% and statistical power of 90% revealed that at least 2005 patients needed to be included. The distribution of estimated number of patients to be included by region was based on the population size in each region of Brazil.
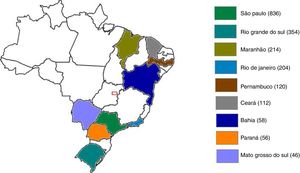
ResultsA total of 2000 patients were included over the study period. Patients were distributed in three different regions of the country: South (20.5%), Southeast (52%) and Northeast/Midwest (27.5%). Figure 1 and Table 1 show the number of patients per state of Brazil and Table 2 summarizes the general characteristics of the sample.
Number of patients with hepatitis C in each state of Brazil included in the study.
| State | n (%) |
|---|---|
| São Paulo | 836 (41.8%) |
| Rio Grande do Sul | 354 (17.7%) |
| Maranhão | 214 (10.7%) |
| Rio de Janeiro | 204 (10.2%) |
| Pernambuco | 120 (6.0%) |
| Ceará | 112 (5.6%) |
| Bahia | 58 (2.9%) |
| Paraná | 56 (2.8%) |
| Mato Grosso do Sul | 46 (2.3%) |
| Total | 2000 (100%) |
Characteristics of the patients included in the study (n=2000).
| n (%) | |
|---|---|
| Sex | |
| Male | 1102 (55.1%) |
| Female | 898 (44.9%) |
| Ethnicity | |
| White | 1293 (64.6%) |
| Brown | 480 (24.0%) |
| Black | 203 (10.2%) |
| Yellow | 6 (0.3%) |
| Not informed | 18 (0.9%) |
| Age mean±SD (years) | 58±10.9 |
| Marital status | |
| Married | 1113 (55.6%) |
| Single | 447 (22.4%) |
| Divorced | 240 (12%) |
| Widowed | 200 (10%) |
| Educational level | |
| Incomplete elementary school | 631 (31.6%) |
| Complete high school | 526 (26.3%) |
| Complete elementary school | 312 (15.6%) |
| Complete higher education | 255 (12.8%) |
| Incomplete high school | 120 (6%) |
| Incomplete higher education | 91 (4.5%) |
| Postgraduation | 41 (2.1%) |
| Illiterate | 23 (1.1%) |
| Monthly household income | |
| ≤5 minimum wages | 1685 (84.25%) |
| 5–10 minimum wages | 238 (11.9%) |
| >10 minimum wages | 77 (3.85%) |
Minimum wage in Brazil: $246 US dollars/month.
The mean time between diagnosis of the infection and the beginning of follow-up at a referral center was 22.9±48.1 months. This interval varied significantly across the different regions: 36.6±46.7 months in the South, 21.6±47.7 months in the Southeast, and 15.2±47.7 months in the Northeast/Midwest (p<0.001). On the other hand, in the South and Southeast regions patients were diagnosed at a younger age compared to patients from the Northeast/Midwest (p<0.001). These data are shown in Table 3.
Age of patients at diagnosis of hepatitis C and time spam between diagnosis and follow-up at a referral center according to microregions of Brazil.
| Northeast/Midwest (n=550) | Southeast (n=1040) | South (n=408) | Total (n=1998) | p-value | |
|---|---|---|---|---|---|
| Age at hepatitis C detection (years) | 50.4±12.3 | 46.7±12.9 | 47.5±11.2 | 47.9±12.5 | 0.033 |
| Time between diagnosis and follow-up (months) | 15.2±47.7 | 21.6±47.7 | 36.6±46.7 | 22.9±48.1 | <0.001 |
Values are mean±standard deviation.
The reason for being tested and the specialty of the physician who requested the test are given in Table 4. General practitioners were found to play a leading role in the diagnosis of infection, being responsible for the detection of almost one-third of cases. This pathway of detection was more common in the Northest/Midwest and South regions (38.9% and 43% of cases, respectively) than in the Southeast (26%, p<0.001).
Aspects related to chronic hepatitis C diagnosis.
| Reason for diagnostic testing | n (%) |
|---|---|
| Check-up | 663 (33.2%) |
| Blood donation | 379 (19%) |
| Investigation of altered liver test | 329 (16.5%) |
| Preoperative | 75 (3.8%) |
| Detection campaign | 61 (3.1%) |
| Relative with hepatitis C | 54 (2.7%) |
| Periodic examination at work | 48 (2.4%) |
| Prenatal | 31 (1.6%) |
| Unknown reason | 13 (0.7%) |
| Other | 345 (17.3%) |
| Physician who made the diagnosis | |
| General practitioner | 468 (30.1%) |
| Gastroenterologist | 236 (15.2%) |
| Anesthesiologist | 129 (8.3%) |
| Gynecologist and obstetrician | 94 (6%) |
| Hematologist | 91 (5.8%) |
| Hepatologist | 90 (5.8%) |
| Surgeon | 38 (2.4%) |
| Other | 411 (26.4%) |
In men, the diagnosis was commonly made by routine test (check-up) (33.7%) and blood donation (24.4%), while women were more frequently diagnosed during check-up (44.4%) or investigation of altered ALT (17.4%) (p<0.001).
The most frequently genotype was 1b (32.8%), followed by genotypes 1a (25.4%), 3 (20.8%), 1 indeterminate subtype (15.5%), and 2 (2.4%). Regarding fibrosis stage at diagnosis, there was a predominance of cirrhotic patients (31.3%). Stages F0/F1 were observed in 29.1% of cases, F2 in 19.1%, and F3 in 18.6%. Fibrosis score was mainly evaluated by liver biopsy (61.5%), followed by liver elastography (24.5%), and a clinical diagnosis of cirrhosis (13.9%).
The main associated comorbidities were hypertension (35.4%), diabetes mellitus (20.2%), and HIV coinfection (6.5%).
DiscussionCurrently, the greatest challenge in fighting chronic hepatitis C is to diagnose asymptomatic patients and provide treatment with the now available highly safe and effective drugs. Within this context, understanding where already diagnosed patients come from and the bottlenecks they face while seeking treatment will help developing effective strategies to eradicate this infection in the future, as determined by the goals of the World Health Organization.7
In the present study, most patients with chronic hepatitis C were from the state of São Paulo. The prevalence of HCV-infected patients was similar in the studied geographical regions,8 but the higher number of inclusions in the state of São Paulo was expected since São Paulo is the most populous state of the country (more than 44 million inhabitants) and has the largest referral network. Observation of the sample permitted to trace a profile of HCV-infected patients attending public referral services: male, white, older than 50 years, and low socioeconomic status. These were the most commonly observed characteristics, which may guide primary care physicians in their daily practice since considering chronic hepatitis C as a possible diagnosis, the first step to prevent the disease from going unnoticed. Regarding age, investigation of anti-HCV in people older than 45 years (the so-called baby boomers) has been found to be effective in most countries in identifying undiagnosed patients.9
The study also demonstrated an important role of primary care physicians who were the main professionals responsible for the identification of new patients – 30% of the patients were diagnosed by a general practitioner. Check-up was the main reason for testing in one-third of asymptomatic patients. The role of primary care physicians was more important in the Northeast/Midwest and South regions when compared to the Southeast region, economically more developed than the others. In effect, other studies reinforce the importance of primary care physicians in identifying new patients.10,11
Considering that initial disease screening is relatively simple (investigation of blood anti-HCV antibodies with a serological test), the large proportion (80%) of infected patients that had not been diagnosed is alarming.12 Problems with medical training, low educational level of the population, difficult access to skilled health services or simply the lack of these services are some of the possible explanations for this finding. In fact, about half the patients of this sample with a diagnosis of chronic hepatitis C had only elementary school. In addition to this low educational level, these patients had a low monthly income, limiting the opportunity to access health services.
Another important finding of this study was the long interval between diagnosis of the disease and beginning of follow-up at a referral center, 22.9 months. This time span of almost two years could make the difference between a disease with favorable evolution and easy treatment and the development of cirrhosis, with subsequent liver failure or hepatocellular carcinoma that could need a liver transplant or progress to death. Longer periods before HCV diagnosis also enhance the chance of transmission within the community. A significantly shorter interval (15.2 months) was observed in the Northeast/Midwest and the reason for this finding is not completely clear. Despite smaller number of referral centers, the referral pattern of patients maybe more expeditious in these regions as there are fewer patients and access is probably less bureaucratic. In addition to clinical suspicion of the disease and confirmatory diagnosis, speeding up bureaucracy and procedures for patient referral as well as more health care providers are key factors for improving health care. As a consequence of this scenario more than 31% of the patients had cirrhosis at diagnosis. In an American study, only 12% of newly diagnosed after 2012 patients had advanced fibrosis demonstrating the efficacy of implementating routine HCV testing in persons born between 1945 and 1965.13
With regard to public spending, undoubtedly, reducing the time span from diagnosis to ultimately start treatment of patients with chronic hepatitis C is less expensive than the management of complications or liver transplantation and subsequent follow-up.14
Check-up was the most common source of chronic hepatitis C testing. When stratified by sex, check-up continued to be the most common source in both, followed by blood donation in men and by the investigation of an altered liver test in women. Regarding blood donation, more than 70% of the diagnoses originating from this source were in men. This finding agrees with the international literature showing that 61% of blood donors are male.15 These data highlight the importance of including anti-HCV tests in routine check-up examinations, especially for patients older than 45 years. In women, gynecologists have an important role since they often act as primary care physicians for female patients.
This study has some limitations. Not all regions of the country were studied, since data from the North region were not available. Information regarding characteristics of patients was based on non-standardized records, but most of the information was homogeneous between centers, permitting adequate comparisons among the different regions of the country.
In summary, there are several important aspects in which health policies could improve the chronic hepatitis C scenario in Brazil. Increasing diagnostic suspicion by investing in educational programs for physicians, general health care professionals, and students could provide good long-term results. Information for the population educating about the disease, risks of transmission, possible complications, symptoms, and treatment is equally important. Detailed data identifying how already diagnosed patients reach the health system were still lacking in Brazil. The path these patients go through, where they are identified, and the time that elapsed from diagnosis to treatment at a health service are of vital importance to propose strategies for access to diagnosis and treatment of chronic hepatitis C in a country like Brazil, which is characterized by so many geographical and social inequalities.
Conflicts of interestThe authors declare no conflicts of interest.
The authors thank Gilead Sciences, Inc. for the financial support