Men who have sex with men (MSM) account for the highest prevalence of HIV in Brazil. HIV testing allows to implement preventive measures, reduces transmission, morbidity, and mortality.
MethodsWe conducted a cross-sectional study to evaluate HIV testing during lifetime, factors associated with the decision to test, knowledge about HIV transmission, and use of condoms between MSM from the city of Natal, northeast Brazil.
ResultsOut of 99 participants, 62.6% had been tested for HIV during lifetime, 46.2% in the last year. The most frequent reported reason to be tested for HIV infection was curiosity (35.5%). Correct knowledge about HIV was observed in only 9.2% of participants. In multivariate analysis, age (PR 0.95; 95%CI, 0.91–0.99; p=0.041) and previous syphilis test (PR 4.21; 95%CI, 1.52–11.70; p=0.006) were associated with HIV testing.
ConclusionsThe frequency of HIV testing among MSM from Natal is rather low, especially in younger MSM, and knowledge about HIV transmission is inappropriate.
The overall prevalence of HIV infection in Brazil is estimated at 0.4%, but the epidemic is highly concentrated in vulnerable populations, with 5.3% prevalence among sex workers and 19.8% in men who have sex with men (MSM) according to the last reports.1 The higher risk of HIV infection among MSM may be partly explained by the practices and behaviors associated with anal sex and the gut tropism of HIV.2,3 Besides that, behavioral vulnerabilities act together increasing the chances of HIV infection between MSM, such as no condom use, practice of transactional sex, use of drugs during sex, and sex with casual partners.4
In 2015, the Joint United Nations Program on HIV/AIDS (UNAIDS) proposed that by 2020, 90% of people living with HIV should be aware of their HIV status, as the first part of 90-90-90 strategy to end AIDS epidemic.5 Early detection of HIV allows initiating care for proper treatment, which impacts in morbidity, mortality, and reduces further transmission.2 In Brazil, HIV testing is recommended for all pregnant women and patients with diagnosis of tuberculosis, visceral leishmaniasis, or sexually transmitted infections.6 Studies estimated that the delay between infection and first CD4 count in Brazil was 4.3 years, showing that a large proportion of individuals still started treatment late in the country.7 In Northeast Brazil 8800 new cases of AIDS are detected per year and in Natal the mean CD4 count at diagnosis is 269cells/mm3, pointing to late diagnosis of HIV.1
Although the group of MSM accounts for the highest prevalence of HIV in the country, there is no specific recommendation for HIV testing in this population in Brazil.6 Data available from developed countries show that the proportion of MSM never testing for HIV is generally below 30%.8,9 Since few studies evaluated HIV testing among MSM in Brazil, especially in Northeast region, our study aimed to access the rate and factors associated with HIV testing among MSM from Natal city, Northeast Brazil.
Materials and methodsStudy designThis is a cross-sectional study, conducted in the city of Natal, between August 2011 and December 2012. The primary objective was to evaluate previous HIV testing among MSM from Natal during lifetime. Based on previous studies we anticipate that younger age and lower education would be associated with lack of testing,10,11
Study sampleParticipants were MSM aged 18 years old or more, residing or working in Natal. They were recruited using respondent-driven sampling (RDS) approach initially.12 Six MSM were selected as initial seeds, chosen through focus group. The focus group was conducted with 15 MSM representatives of artistic scene, student activism and social movement from Natal, the initial seeds were selected considering demographic characteristics, like age and socioeconomic status, and network size. Each seed was allowed to recruit three participants, using study coupons pre-printed with the study center phone number and location. Staff screened subjects in the study site for the following eligibility criteria: age over 18 years, living or working in the city of Natal, and having engaged in anal intercourse with another man in the previous year. Each included participant received three coupons to invite more people for the study.
ProceduresThe study was conducted at a health care facility inside the university. The study questionnaire consisted of objective questions to be self-administered and based on a behavioral instrument used previously with this population in Brazil.13 Participants responded to the questions in a private office. Questions included socioeconomic and demographic characteristics, history of HIV testing, reasons to do the test, use of condom in the last sexual relation, HIV status of sexual partners, transactional sex, previous syphilis test, knowledge of places were HIV testing is free, and adequate knowledge about HIV prevention, according to United Nations General Assembly Special Session on HIV/AIDS (UNGASS) indicator, defined as the percentage of respondents giving correct answers to all the following five questions14:
Can having sex with only one faithful, uninfected partner reduce the risk of HIV transmission? (yes);
Can using condoms reduce the risk of HIV transmission? (yes);
Can a healthy-looking person have HIV? (yes)
Can a person get HIV by using public toilets? (no)
Can a person get HIV by sharing a meal with someone who is infected? (no)
A rapid test for HIV using hole blood was offered for the participants at study site (Rapid Check HIV-1/2 and/or Bio-Manguinhos HIV-1/2), with pre- and post-test counseling and the result was given immediately, according to Brazilian guidelines.15
Statistical analysisSample size was calculated to be 95 subjects, assuming a prevalence of 60% for previous HIV testing during lifetime, 95% confidence and a 10% error, based on previous data from Adam et al. for 10 countries in Latin America.16 Descriptive analysis included central tendency measures calculated for continuous variables and proportions were calculated for categorical variables. The association between previous HIV testing and explanatory variables was assessed by univariate analysis using Pearson's Chi-square or Fischer exact test when appropriate. For continuous variables, Student's “t” test was performed. Associations with a p-value less than 0.05 were considered significant. In order to verify the adjusted effect, Poisson Regression Modeling with robust variance were performed, including those variables with p-values less than 0.2. Data were analyzed using SPSS (Statistical Package Software for Social Science) version 20.0.
EthicsThe study was approved by the Ethic Research Committee of Federal University of Rio Grande do Norte (number 136/11). All participants signed a written informed consent.
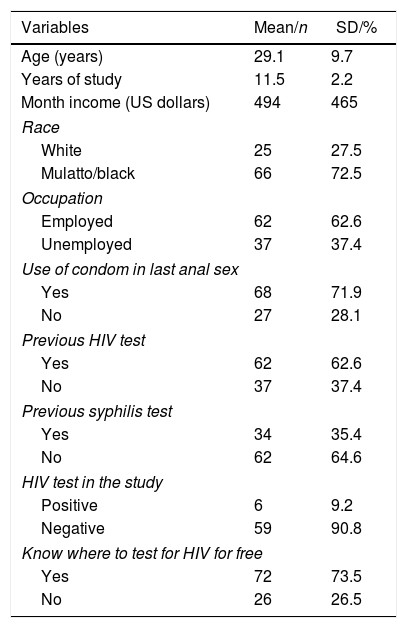
ResultsBy November 2012, 70 subjects were included using RDS, despite many efforts of the study team to improve recruitment, including increase in the hours of operation of the study site and adding six more seeds. As our planed sample was 95 MSM, we decided to include a venue-based sample of additional 31 subjects recruited during the gay pride event in Natal city in December 2012. From 101 participants, two were excluded because they answered less than 70% of the questionnaire, totaling a sample of 99 subjects. Sociodemographic characteristics of participants are shown in Table 1. The mean age was 29.1 years (SD 9.7 years), 73.3% identified themselves as mulatto or black, mean monthly income was 494 US dollars (SD 465 dollars), and 61.5% were employed. Participants had a mean of 11.5 years of schooling (SD 2.2 years).
Sociodemographic characteristics of 99 MSM from Natal.
| Variables | Mean/n | SD/% |
|---|---|---|
| Age (years) | 29.1 | 9.7 |
| Years of study | 11.5 | 2.2 |
| Month income (US dollars) | 494 | 465 |
| Race | ||
| White | 25 | 27.5 |
| Mulatto/black | 66 | 72.5 |
| Occupation | ||
| Employed | 62 | 62.6 |
| Unemployed | 37 | 37.4 |
| Use of condom in last anal sex | ||
| Yes | 68 | 71.9 |
| No | 27 | 28.1 |
| Previous HIV test | ||
| Yes | 62 | 62.6 |
| No | 37 | 37.4 |
| Previous syphilis test | ||
| Yes | 34 | 35.4 |
| No | 62 | 64.6 |
| HIV test in the study | ||
| Positive | 6 | 9.2 |
| Negative | 59 | 90.8 |
| Know where to test for HIV for free | ||
| Yes | 72 | 73.5 |
| No | 26 | 26.5 |
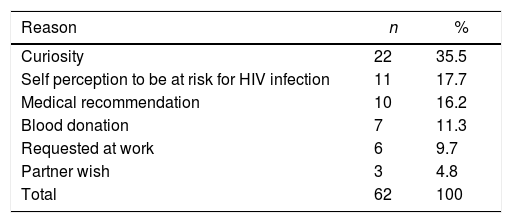
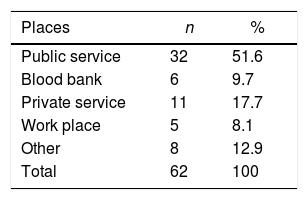
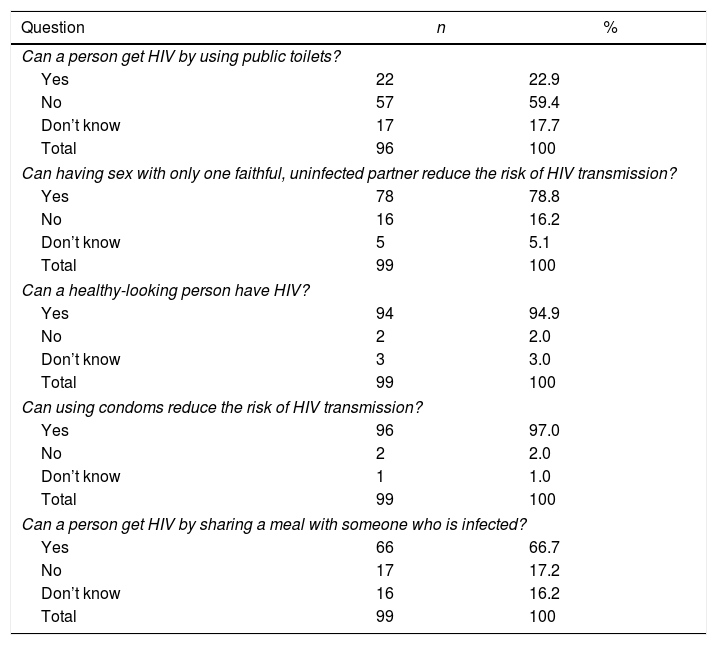
Out of 99 participants, 62.6% (CI 95% 52.5–71.7%) had been tested for HIV, 46.2% (CI 35.5–57%) in the last year. The most frequent reason to be tested was curiosity (35.5%), 17.7% because they perceived themselves to be at risk for HIV infection, and 16.2% were asked to be tested by a health professional (Table 2). The most frequent place for testing was public services mentioned by 52.4% (Table 3). Only 9.2% of participants had adequate knowledge about HIV transmission. The questions with the highest percentages of wrong answers were “Can a person get HIV by sharing a meal with someone who is infected?” (66.7% marked ‘yes’) and “Can a person get HIV by using public toilets?” (22.9% marked ‘yes’) [Table 4].
Knowledge about HIV by MSM from Natal city, Brazil, 2012.
| Question | n | % |
|---|---|---|
| Can a person get HIV by using public toilets? | ||
| Yes | 22 | 22.9 |
| No | 57 | 59.4 |
| Don’t know | 17 | 17.7 |
| Total | 96 | 100 |
| Can having sex with only one faithful, uninfected partner reduce the risk of HIV transmission? | ||
| Yes | 78 | 78.8 |
| No | 16 | 16.2 |
| Don’t know | 5 | 5.1 |
| Total | 99 | 100 |
| Can a healthy-looking person have HIV? | ||
| Yes | 94 | 94.9 |
| No | 2 | 2.0 |
| Don’t know | 3 | 3.0 |
| Total | 99 | 100 |
| Can using condoms reduce the risk of HIV transmission? | ||
| Yes | 96 | 97.0 |
| No | 2 | 2.0 |
| Don’t know | 1 | 1.0 |
| Total | 99 | 100 |
| Can a person get HIV by sharing a meal with someone who is infected? | ||
| Yes | 66 | 66.7 |
| No | 17 | 17.2 |
| Don’t know | 16 | 16.2 |
| Total | 99 | 100 |
Transactional sex was frequent, as 42% reported having received money in exchange for sex in the previous six months. Use of condom in the last anal intercourse was mentioned by 71.9%. Only 13.1% were aware of the HIV status of sexual partners. Of the 63 MSM who agreed to perform an HIV test, six turned out positive (9.5%) [Table 1].
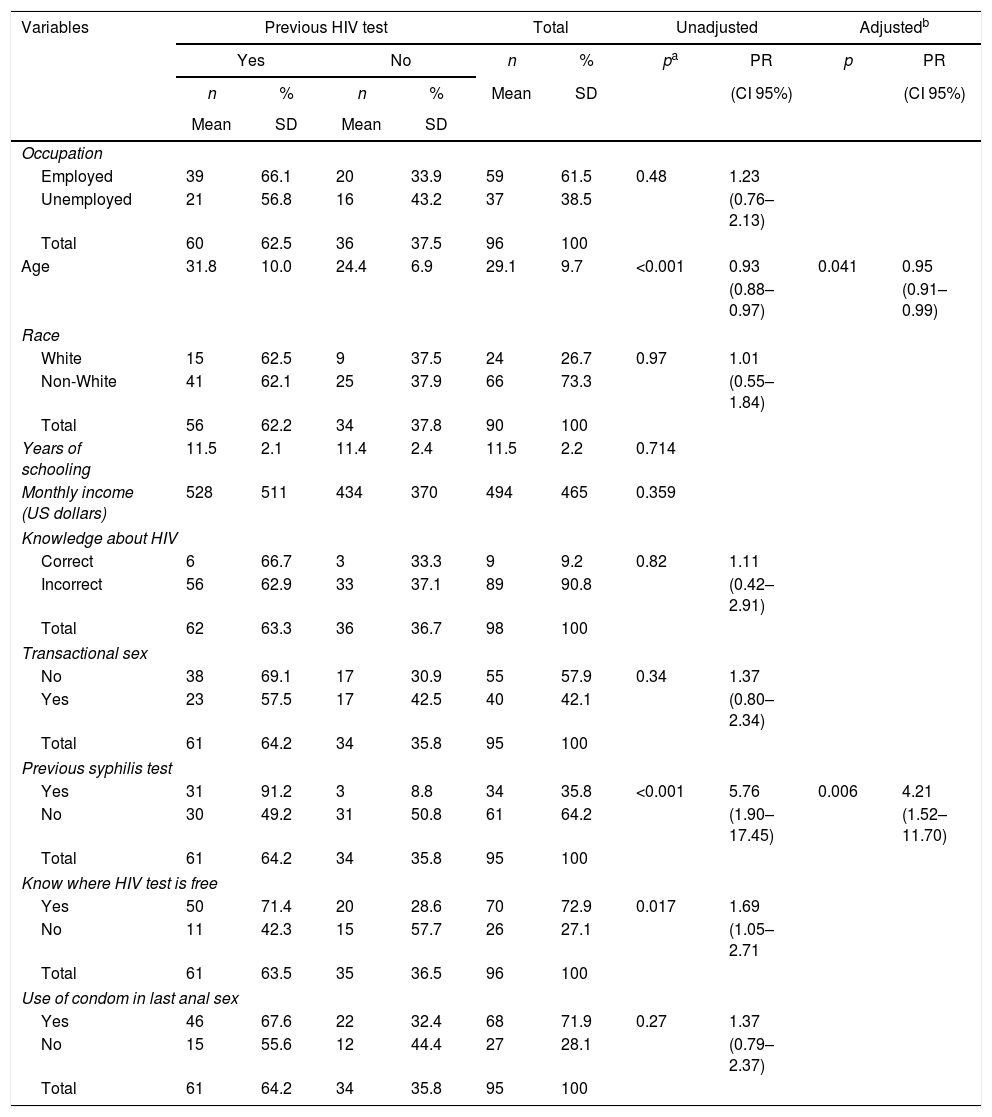
In univariate analysis, age (PR 0.93; 95% CI, 0.88–0.97; p<0.001) and previous syphilis test (PR 1.85; 95% CI, 1.41–2.44; p<0.001) were associated with HIV testing. Knowing a place where the HIV test could be done free-of-charge was also associated with HIV testing (PR 1.69; 95%CI, 1.05–2.71; p=0.017), as most MSM did the test in public services (Table 5). In adjusted analysis, resulted from Poisson modeling, the variables “age”, “previous syphilis test”, and “knowing where HIV test was free” where included in a stepwise logistic regression analysis. In the final predictive model only “age” and “previous syphilis test” remained independently associated with previous HIV testing (Table 5).
Univariate analysis of selected characteristics of MSM and prior HIV testing in Natal city, Brazil, 2012.
| Variables | Previous HIV test | Total | Unadjusted | Adjustedb | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | n | % | pa | PR | p | PR | |||
| n | % | n | % | Mean | SD | (CI 95%) | (CI 95%) | |||
| Mean | SD | Mean | SD | |||||||
| Occupation | ||||||||||
| Employed | 39 | 66.1 | 20 | 33.9 | 59 | 61.5 | 0.48 | 1.23 | ||
| Unemployed | 21 | 56.8 | 16 | 43.2 | 37 | 38.5 | (0.76–2.13) | |||
| Total | 60 | 62.5 | 36 | 37.5 | 96 | 100 | ||||
| Age | 31.8 | 10.0 | 24.4 | 6.9 | 29.1 | 9.7 | <0.001 | 0.93 | 0.041 | 0.95 |
| (0.88–0.97) | (0.91–0.99) | |||||||||
| Race | ||||||||||
| White | 15 | 62.5 | 9 | 37.5 | 24 | 26.7 | 0.97 | 1.01 | ||
| Non-White | 41 | 62.1 | 25 | 37.9 | 66 | 73.3 | (0.55–1.84) | |||
| Total | 56 | 62.2 | 34 | 37.8 | 90 | 100 | ||||
| Years of schooling | 11.5 | 2.1 | 11.4 | 2.4 | 11.5 | 2.2 | 0.714 | |||
| Monthly income (US dollars) | 528 | 511 | 434 | 370 | 494 | 465 | 0.359 | |||
| Knowledge about HIV | ||||||||||
| Correct | 6 | 66.7 | 3 | 33.3 | 9 | 9.2 | 0.82 | 1.11 | ||
| Incorrect | 56 | 62.9 | 33 | 37.1 | 89 | 90.8 | (0.42–2.91) | |||
| Total | 62 | 63.3 | 36 | 36.7 | 98 | 100 | ||||
| Transactional sex | ||||||||||
| No | 38 | 69.1 | 17 | 30.9 | 55 | 57.9 | 0.34 | 1.37 | ||
| Yes | 23 | 57.5 | 17 | 42.5 | 40 | 42.1 | (0.80–2.34) | |||
| Total | 61 | 64.2 | 34 | 35.8 | 95 | 100 | ||||
| Previous syphilis test | ||||||||||
| Yes | 31 | 91.2 | 3 | 8.8 | 34 | 35.8 | <0.001 | 5.76 | 0.006 | 4.21 |
| No | 30 | 49.2 | 31 | 50.8 | 61 | 64.2 | (1.90–17.45) | (1.52–11.70) | ||
| Total | 61 | 64.2 | 34 | 35.8 | 95 | 100 | ||||
| Know where HIV test is free | ||||||||||
| Yes | 50 | 71.4 | 20 | 28.6 | 70 | 72.9 | 0.017 | 1.69 | ||
| No | 11 | 42.3 | 15 | 57.7 | 26 | 27.1 | (1.05–2.71 | |||
| Total | 61 | 63.5 | 35 | 36.5 | 96 | 100 | ||||
| Use of condom in last anal sex | ||||||||||
| Yes | 46 | 67.6 | 22 | 32.4 | 68 | 71.9 | 0.27 | 1.37 | ||
| No | 15 | 55.6 | 12 | 44.4 | 27 | 28.1 | (0.79–2.37) | |||
| Total | 61 | 64.2 | 34 | 35.8 | 95 | 100 | ||||
Our study found that 62.6% of MSM from Natal had been tested for HIV before. This rate was higher than the national average of 37% estimated for the general population in 201113 and the 51.6% found by Brito et al. in MSM from 10 Brazilian cities in 2009.10 These rates are rather disappointing as MSM is a group with a high prevalence of HIV infection. The World Health organization and the Centers for Disease Control and Prevention (CDC) in United States, recommend that persons at high risk for HIV infection should be screened for HIV at least annually.17,18 It should be pointed out that testing at any time was accounted for, rather than being restricted to the last year. If only testing in the previous year were considered the rate would be even lower (46.2%). Previous studies conducted in Argentina, Peru, and China showed HIV testing rates varying between 48% and 58%,9,11,19 but studies from United States and Puerto Rico had a much better result (82–90%).20,21
Lack of knowledge about HIV transmission is one of the reasons that lead to low perceived risk of being infected. Hall et al. found that testing was higher among high school students if they were taught at school about AIDS or HIV.22 Although adequate knowledge about HIV transmission was not significantly associated with HIV testing, it is noteworthy the low level of knowledge, despite the high educational level. The percentage of adequate knowledge in a study with the Brazilian general population was much higher, reaching 57.1%,13 but Guimarães et al. indicate a decrease in the proportion of MSM with adequate HIV knowledge from 35.2% in 2009 to 23.7% in 2016.23 Campaigns carried out by the Ministry of Health in Brazil have focused primarily on condom use as a way to avoid HIV infection, leaving aside clarification on situations that have no risk of transmission, such as sharing a meal or use of public toilets. In our country, AIDS is still a topic rarely addressed in schools, and even when this approach is carried out, it is usually not systematic. The school is often the only place where young people can receive reliable information. However, most often school teachers are NOT well prepared, and may end up delivering incomplete information. Alternative interventions like peer education and internet and social media strategies to access MSM have proven to be useful in studies from Peru and United States.19,24 In 2015, a team of governmental, research, and non-governmental organizations in the city Curitiba in South Brazil launched and evaluated a multi-component implementation science project to improve HIV outcomes for MSM. This project, called “A Hora é Agora” (“The Time is Now”) implemented a web-based platform and associated mobile application designed to provide HIV prevention information, allowing for self-assessment of risk and delivering HIV self-test kits. The project exceeded all expectations with 7352 HIV self-test requests over 24 months, as the initial goal was to distribute 1000 test kits per year, and was able to reach a large percentage (31%) of MSM who had never been tested before, with those between 18 and 28 years old reporting a higher percentage of first-time testers (36%) than those 29 years or older (18%).25 The same project is now being implemented in the city of São Paulo.26
Younger age was associated with never testing for HIV in this study, which is worrisome since the last national epidemiological report data showed that the HIV epidemic is increasing in this group.1 A study evaluating sexual risk behavior among MSM from 10 Brazilian cities showed that to be aged 25 years or less was independently associated with higher scores of risky behavior.27 A recent study from Germany also showed that younger age (<25 years) was associated with lower rates of HIV testing.28 The very absence of testing could be a contributing factor to the increased number of infections in this population, since people with HIV on antiretrovirals are less likely to transmit the virus than those who do not use them, a category which include HIV carriers that have not been diagnosed.29,30 The proposal of treatment as prevention relies on a model of universal testing, reinforcing that barriers to HIV testing will become more relevant to the full spectrum of HIV care. Maximizing testing opportunities and reducing barriers to regular testing should be a central component of HIV prevention programs.31
This study has some limitations. The RDS technique was not effective for the population of MSM from Natal, as it has not reached the sample size initially calculated. Few seeds had enough waves to disperse the sample and make it closer to a probabilistic sample, even with all efforts from the research team to improve recruitment. Similar difficulties have been reported with the use of RDS technique by researches in Singapore.32 We ended up analyzing our entire group as a non-probabilistic sample as a consequence of these difficulties. Therefore, these results may not be representative of the entire Natal MSM population. Some of the results that did not show statistical significance may have been influenced by the sample size that may have not been sufficient to show associations. However, there is relevance to the study because it represents a population that is difficult to access in a location where no similar study had been performed previously.
ConclusionThe study shows that HIV testing rates are low among this sample of MSM, and younger age and previous syphilis test were associated with never testing in multivariate analysis. Knowing a place where the HIV test can be done free-of-charge was associated with HIV testing in univariate analysis but lost significance in the multivariate model. Actions that prioritize the dissemination of places where HIV testing can be done for free and targeted at young people seem to be most suitable for scaling up HIV testing among MSM in our reality. Also important is the fact that knowledge about HIV transmission was low, despite the high educational level of the participants, emphasizing the need for innovative approaches to disseminate prevention information for MSM.
Sources of supportNational Fund of Health, Ministry of Health, Brazil.
Conflicts of interestThe authors declare no conflicts of interest.