The distribution of hepatitis B virus genotypes in Saudi Arabia is largely unknown. To the best of our knowledge there are no data available about HBV genotypes in southwestern region of the country. This study aimed to determine the epidemiologic distribution of hepatitis B virus genotypes in chronic hepatitis B patients in southwestern region, and to verify possible correlations between these genotypes and the clinical symptoms. A total of 160 patients with chronic hepatitis B infection were enrolled in this study. Sera were tested for liver function tests, hepatitis B virus markers and DNA load by standard procedures. HBV genotyping was performed by 2-tube nested PCR for determination of six genotypes (A–F). Genotype D was the most common, found in 135 (84.4%) patients, followed by A (18; 11.3%) and E (7; 4.3%). The rate of HBeAg positivity in genotype D patients was significantly lower compared with that in genotype A and E patients (p=0.01). There was no significant association between HBV genotypes and age, gender, liver function tests, or HBV DNA load. Genotypes D and E were predominant in chronic hepatitis B patients in southwestern Saudi Arabia. Awareness of hepatitis B virus serologic and genotypic patterns might help in the formulation of management plans, predicting clinical outcomes and updating prevention strategies.
Hepatitis B virus (HBV) infection is a potentially life-threatening liver disease and represents a major global health problem. About two billion people have been infected with HBV worldwide, and 400 million among them are suffering from chronic HBV (CHB) infection.1,2 In Saudi Arabia, the prevalence of HBV infection has declined considerably since the introduction of the HBV vaccine in the national immunization program in 1989.3 However, different reports have shown that HBV infections continue to be a major burden on the Saudi healthcare system. According to Algarni et al., 23,236 cases of HBV infection have been reported to the Saudi Ministry of Health during the 5-year period from 2009 to 2013 and the incidence rates were 19.3 and 14.7 per 100,000 populations in 2009 and 2013, respectively.4
According to the molecular evolutionary analysis of genomic DNA sequence, HBV strains isolated in various countries are classified into ten genotypes, designated A–J, and arbitrarily defined by an inter-group sequence divergence of more than 8% based on complete genomes.5,6 Genotype distribution shows variations between countries, and even between geographical regions within countries. Genotype A is widespread in sub-Saharan Africa, Northern Europe, and Western Africa; genotypes B and C are common in Asia; genotype C is primarily observed in Southeast Asia; genotype D is dominant in Africa, Europe, Mediterranean countries, and India; genotype E is found in central and western Africa; genotype F is dominant in Latin America and Alaska; genotype G is reported in France, Germany, and the United States; and genotype H is commonly encountered in Central and South America. Genotype I has recently been reported in Vietnam and Laos. The newest HBV genotype, genotype J, has been identified in Japan.6–11
Genotyping of HBV is essential for characterization of patient groups and for epidemiological studies. The clinical significance of different HBV genotypes has become increasingly recognized in patients with acute and CHB infection.8–10 Moreover, several studies have shown a strong relationship between HBV genotypes and mutations in the pre-core and core promoter regions that abolish or diminish the production of hepatitis B e antigen (HBeAg). The course of HBV infection depends on several factors such as host genetic factors, age and genetic variability of the virus. In addition to the epidemiological importance, HBV genotypes may influence the disease pattern and response to treatment.6,12
The distribution of HBV genotypes in the Kingdom of Saudi Arabia is largely unknown, and only a few studies have reported the predominance of HBV genotype D in some locations.13,14 To the best of our knowledge there are no data available about HBV genotypes in the southwestern region. Hence, the aims of our study were to determine the epidemiologic distribution of HBV genotypes in Saudi patients with CHB in Najran, a city in southwestern Saudi Arabia, and to verify possible correlations between these genotypes and the clinical symptoms.
This cross-sectional study was conducted at King Khalid Hospital, a 350-bed tertiary care hospital in Najran during a 6-month period from February to October 2014. A total of 160 patients with CHB infection, followed as outpatients at the department of internal medicine were enrolled in this study. Sixty-five (40.6%) patients received treatment with lamivudine monotherapy. Five (3.1%) patients received lamivudine followed by add-on adefovir, while none of the remaining 90 (56.3%) patients had ever received antiviral treatment. The inclusion criteria were all patients who were serum HBsAg positive for at least six months with elevated ALT levels (>1.5 times the upper limit of normal; 65U/L). All of the patients were diagnosed after they had been previously followed for at least 12 months. The exclusion criteria were patients with acute HAV, HBV, HCV, or HDV, patients with evidence for hepatocellular carcinoma (HCC), or concomitant of HCV, HDV, HIV infection, metastatic or autoimmune liver disease and drug induced acute hepatitis. The socio-demographic data and laboratory tests results were recorded using a standardized questionnaire, including the age, gender, underlying medical conditions, signs and symptoms at presentation, findings on physical examination, laboratory findings, and definitive clinical diagnosis.
The levels of serum total bilirubin, albumin, alanine aminotransferase (ALT) and aspartate transaminase (AST) were determined with routine automated techniques. The HBV markers (HBsAg, HBsAb, HBeAg, HBeAb, HBcAb, and anti-HBc Ab IgM) were measured using the enzyme-linked immunosorbent assay (ELISA) kits (Roche Laboratories, Branchburg, NJ, USA). Serum HBV DNA load in patients with CHB was measured by a sensitive PCR based assay (COBAS Amplicor, Roche Diagnostics, Branchburg, NJ, USA) with a lower detection limit of approximately 200copies/mL. HBV genotyping was performed by 2-tube nested PCR, using type specific primers for determination of six genotypes A through F of HBV according to a method previous described by Farazmandfar et al.15
Data were analyzed using the Statistical Package for the Social Sciences (SPSS), Version 15.0 (SPSS Inc., Chicago, IL, USA). Statistical significance was defined as a p-value less than 0.05.
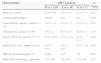
The demographic, serological and virological characteristics of the patients are summarized in Table 1. The patients were between 32 and 52 years of age with a median age of 41 years. Of these patients, 124 (77.5%) were male and 36 (22.5%) were female. Hepatitis B genotyping revealed that 135 patients (84.4%) had genotype D, 18 patients (11.3%) had genotype A, and 7 patients (4.3%) had genotype E. No other HBV genotype or mixed infections were detected in patients enrolled for this study. The demographic, serological and virological characteristics were compared among patients with the different genotypes (Table 2). Univariate analysis indicated that the rate of HBeAg positivity in genotype D patients was significantly lower compared with that in genotype A and E patients (p=0.01). However, there was no significant association between HBV genotypes and age, gender, liver function tests, or HBV DNA load.
Characteristics of 160 patients with chronic HBV infection.
| Characteristics | Values |
|---|---|
| Mean age (years) | 41.6±4.9 |
| Gender (male/female) | 124/36 |
| Total bilirubin (μmol/L; normal: 3–17) | 16.5±1.3 |
| Albumin (g/L; normal: 34–50) | 39.4±2.5 |
| Serum AST (U/L; normal: 15–37) | 86.2±32.1 |
| Serum ALT (U/L; normal: 25–65) | 168.7±58.9 |
| HBeAg (positive/negative, n) | 74/86 |
| HBV DNA load (log10copies/ml) | 15.5±3.4 |
| Genotype D (n, %) | 135, 84.4% |
| Genotype A (n, %) | 18, 11.3% |
| Genotype E (n, %) | 7, 4.3% |
Characteristics of 160 patients with chronic HBV infection, classified by HBV genotype.
| Characteristics | HBV genotype | p-Value | ||
|---|---|---|---|---|
| D (n=135) | A (n=18) | E (n=7) | ||
| Mean age (years) | 42.9+4.9 | 39.7+4.1 | 41.4+5.3 | 0.12 |
| Gender (male/female) | 102/33 | 16/2 | 6/1 | 0.28 |
| Total bilirubin (μmol/L; normal: 3–17) | 16.5±1.4 | 16.4±1.3 | 16.2±1.2 | 0.85 |
| Albumin (g/L; normal: 34–50) | 39±2.1 | 39.5±2.7 | 40.4±2.7 | 0.19 |
| Serum AST (U/L; normal: 15–37) | 95.9+29.1 | 73.4+31.6 | 81.3+32.1 | 0.06 |
| Serum ALT (U/L; normal: 25–65) | 167.1+59.2 | 161.2+56.1 | 193.3+55 | 0.48 |
| HBeAg (positive/negative, n) | 55/80 | 13/5 | 3/4 | 0.01 |
| HBV DNA load (log10copies/ml) | 1.2×106 | 1.8×105 | 2.3×105 | 0.25 |
CHB is an important medical problem in Saudi Arabia, which is currently classified by the WHO as an area of high endemicity (≥8% of population are HBsAg positive).1 Detection of HBV genotype is very important to clarify the pathogenesis, routes of infection and virulence of the virus. However, there is a paucity of information on HBV genotype patterns in Saudi Arabia. In this study, we found that the majority (84.4%) of patients were infected with HBV genotype D, followed by genotypes A (11.3%) and E (4.3%). These results are consistent with previous findings from Saudi Arabia. In a previous Saudi study, 85% of 54 CHB patients had genotype D, while 5.7% and 1.4% had genotypes A and E, respectively.14 In another study, Abdo et al. showed that 81%, 5.7% and 1.4% of 70 hepatitis B patients had genotypes D, E, and A, respectively.13 Reports from the Mediterranean area, Middle East and central and south Asia showed that 70–80% or more of the HBV infections are caused by genotype D.7,8,16–19
The clinical significance of different HBV genotypes has become increasingly recognized in patients with acute and chronic infection. However, the clinical impact of HBV genotype D has been studied less extensively. In this study, similar to previous reports, age, gender, serum total bilirubin, liver enzymes, and HBV DNA levels were not significantly different between patients infected with genotype D and those infected with genotypes A or E.9,10 Contrary to these findings, Youssif et al.18 and Nabuco et al.11 found a significant association between ALT levels and HBV genotypes with lower ALT levels observed in genotype D patients and higher DNA levels in genotype E patients. The clinical outcome of HBV infection and the severity of liver disease with genotype D and E are still controversial. It is well known that patients with CHB may have fluctuating serum ALT and HBV-DNA levels. Further analyses in large-scale longitudinal studies are required to better delineate this relationship.
In chronic infection, levels of viremia are generally low. Long-term prognosis is poorer among HBeAg negative individuals compared to their counterparts who are HBeAg positive.5 In this study, a significantly lower rate of HBeAg positivity in patients with genotype D was reported compared to genotype A and E patients. In agreement, Yousif et al.18 showed a significantly higher frequency of HBeAg positivity in genotype E-infected patients compared to genotype D-infected patients (29.2% versus 8.3%, p<0.05). HBeAg negative CHB is mostly associated with mutations in the pre-core and basal core promoter regions that result in prevention or reduction of HBeAg synthesis without affecting the replicative ability of the virus.12,17,19 Zaky et al.17 found that 94% of 83 Egyptian patients infected with HBV genotype D were HBeAg negative, presumably indicating pre-core or core promoter mutation. Sitnik et al.12 examined hepatitis genotypes in 103 Brazilian patients. Pre-core mutants were found in 32 patients, with a higher frequency in those infected with genotype D (22 cases).
HBeAg negative CHB is characterized by frequent exacerbation of hepatitis, which probably increases the risk of cirrhosis, hepatic failure, and HCC.5 Baig et al.20 found that 8 of 9 HCC patients had HBV genotype D and 4 of 5 cirrhotic patients had HBV genotype A. Our study did not include patients with cirrhosis or HCC. However, in Saudi Arabia, HCC is the second most common cancer,3 and in a country where HBV is endemic this could imply a correlation between the most prevalent genotype D and HCC.
This study had some limitations. Firstly, the relatively small sample size may have limited our ability to detect differences even though it included the highest number of patients genotyped in Saudi Arabia. Secondly, the study included only CHB group of patients. Therefore, large-scale studies including different HBV clinical groups are required to obtain further information on the role of genotype D and E and their impact on the progression of liver diseases.
In conclusion, our findings further illustrate HBV genotype patterns in Saudi Arabia. Genotypes D and E were predominant in CHB patients, and D is the most prevalent genotype in Najran, southwestern Saudi Arabia. The majority of the patients were HBeAg negative suggesting pre-core or core promoter mutations. Awareness of HBV serologic and genotypic patterns might help in the formulation of management plans, predicting clinical outcomes and updating prevention strategies.
Conflicts of interestThe authors declare no conflicts of interest.
This work was supported by a grant from the Deanship of Scientific Research, Najran University (MID 13/26).