Early diagnosis of tuberculosis (TB) is essential for effective treatment of patients; however, traditional diagnostic modalities suffer from low sensitivity and are inadequate for rapid identification of Mycobacterium tuberculosis. Molecular methods targeting detection of M. tuberculosis DNA might represent an alternative, being more sensitive and rapid. IS6110 has been widely used as a target for polymerase chain reaction-(PCR) based diagnosis of TB, although some M. tuberculosis isolates may not have a copy of this element, thereby reducing the sensitivity of IS6110 PCR.1 The gene encoding mpt64, a secretary mycobacterial antigen present only in M. tuberculosis complex,2 has been found to be useful for diagnosis of TB.3,4 We evaluated the utility of in-house mpt64 real-time PCR (RT-PCR) for the diagnosis of M. tuberculosis in pulmonary and extra-pulmonary specimens at a tertiary care center, the Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, in Northern India.
A total of 102 (72 cases, 30 controls) pulmonary and extra-pulmonary specimens from admitted patients were evaluated by mpt64 real-time PCR, conventional tests (smear for Ziehl-Neelsen's [ZN] acid-fast staining, Lowenstein-Jensen [LJ], and BACTEC MGIT 960 culture), and IS6110 PCR, from July to December, 2010. Informed consent was obtained from the patients, and the study was approved by the Ethics Committee of the PGIMER. The patients were categorized as follows: group A (n=30) were controls with no evidence of M. tuberculosis infection; group B (n=51) included patients with clinical features of TB with laboratory confirmation based on ZN staining and/or culture positivity; and group C (n=21) were clinically diagnosed TB patients who were AFB smear- and culture-negative but had clinical, histopathological, and radiological evidence of TB. In-house mpt64 RT-PCR was performed using the following primers: mpt64 (forward) – 5’CCTCGGCCACATACCAGTCC3’ and mpt64 (reverse) – 5’TGTCCGGTCTGCTTGCTCAG3’, and IS6110 PCR was carried out as described previously.5M. tuberculosis H37RV was used as positive control, and PCR grade water was used as negative control. The outcome parameters, i.e., sensitivity, specificity, positive predictive value, and negative predictive value were calculated using groups B and C (B+C) as the reference standard.
All the tests were found to be negative in the control group, thus showing a specificity of 100% (95% CI; 88.4-100). Of the 72 patients (groups B+C), 31 (43.1%, 95% CI; 31.4-55.3) were smear-positive, 47 (65.3%, 95% CI; 53.1-76.1) were culture-positive, mpt64 RT-PCR was positive in 48 (76.4%, 95% CI; 64.9-85.6), and IS6110 could detect TB in 37 (52%, 95% CI; 39.3-63.4) patients, thus mpt64 RT-PCR detected the maximum number of cases. Of the 51 patients in group B, 37 (72.5%) were detected by IS6110 PCR and 43 (84.3%) by mpt64 RT-PCR assay, while of the 21 clinically diagnosed patients (smear- and culture-negative), mpt64 RT-PCR was positive in five (23.8%) patients, thus it detected five additional patients.
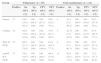
Amongst the 50 pulmonary specimens of group B+C (44+6), mpt64 RT-PCR was positive in 37 patients, showing a sensitivity of 74% (95% CI; 59.7-85.4), while the sensitivity of IS6110 PCR was found to be 66% (95% CI; 51.2-78.8). Amongst the 22 extra-pulmonary specimens, mpt64 RT-PCR showed the highest sensitivity and was able to detect 11 (50%, 95% CI; 28.2-71.8) patients; IS6110 PCR was positive in four (18%, 95% CI; 5.2-40.3) patients, while AFB smear and culture were positive in four (18%, 95% CI; 5.2-40.3) and five (22.7%, 95% CI; 7.8-45.4) patients respectively (Table 1).
Comparison of results in pulmonary and extra-pulmonary specimens (controls, n=30).
| Group | Pulmonary (n=50) | Extra-pulmonary (n=22) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Positive | Sn (95% CI) | Sp (95% CI) | PPV (95% CI) | NPV (95% CI) | Positive | Sn (95% CI) | Sp (95% CI) | PPV (95% CI) | NPV (95% CI) | |
| Smear | 27 | 54.0 (39.3–68.2) | 100 (88.4–100) | 100 (87.2–100) | 56.6 (42.3–70.2) | 4 | 18.2 (5.2–40.3) | 100 (88.4–100) | 100 (39.8–100) | 62.5 (47.4–76.1) |
| Culture | 42 | 84.0 (70.9–92.8) | 100 (88.4–100) | 100 (91.6–100) | 79.0 (62.7–90.5) | 5 | 22.73 (7.8–45.4) | 100 (88.4–100) | 100 (47.8–100) | 63.8 (48.5–77.3) |
| IS6110 PCR | 33 | 66.0 (51.2–78.8) | 100 (88.4–100) | 100 (89.4–100.0) | 63.8 (48.5–77.3) | 4 | 18.2 (5.2–40.3) | 100 (88.4–100) | 100 (39.8–100) | 62.5 (47.4–76.1) |
| mpt64 RT-PCR | 37 | 74.0 (59.7–85.4) | 100 (88.4–100) | 100 (90.5–100) | 69.8 (53.9–82.8) | 11 | 50.0 (28.2–71.8) | 100 (88.4–100) | 100 (71.5–100) | 73.2 (57.1–85.8) |
CI, confidence interval; Sn, sensitivity; Sp, specificity; PPV, positive predictive value; NPV, negative predictive value.
In our study, M. tuberculosis infection in pulmonary and extra-pulmonary specimens could be detected with a higher analytical sensitivity by the mpt64 RT-PCR assay when compared to IS6110 PCR and other conventional diagnostic modalities. IS6110 PCR may fail to detect many such cases, as has been previously reported,6,7 indicating the need to have alternate gene targets for the diagnosis of TB. We observed that mpt64 RT-PCR detected 11 of the 22 extra-pulmonary specimens, while culture and IS6110 PCR could detect only five and four patients, respectively. Also, in clinically diagnosed TB patients (group C), mpt64 RT-PCR was positive in five patients, while IS6110 PCR, culture, and smear examination missed these patients; thus, mpt64 RT-PCR detected the maximum number of cases from paucibacillary specimens.
In conclusion, an integrated approach for the early identification of TB is the need of the hour. Molecular diagnosis by RT-PCR using mpt64 is useful for early detection of TB, and is especially helpful to secure the diagnosis in extra-pulmonary smear-negative cases.
Conflict of interestAll authors declare to have no conflict of interest.